Abstract
Decades after its introduction, dilatation and evacuation (D&E) is still not universally offered by gynaecologists who provide second trimester abortion. Three lines of evidence point to D&E as the preferred method for most women. First, the uterus has evolved to expel its contents early and late in pregnancy, not in the middle. Hence, induction of labour with medical abortion forces the uterus to perform a task it is not designed to do. Second, cohort studies and randomised, controlled trials over the past 30 years have consistently shown that D&E is safer and more effective than labour induction abortion, regardless of the abortifacient used. Third, the ethical principles of beneficence, autonomy and justice require that D&E be routinely offered by gynaecologists who perform second trimester abortions. The uneven geographical availability of D&E may stem from lack of information, lack of requisite equipment and training, or lack of motivation. According to the principles of evidence-based medicine and bioethics, these barriers to better care for women can and should be overcome.
Résumé
Des décennies après son introduction, la technique de la dilatation et évacuation n'est toujours pas proposée par tous les gynécologues qui réalisent des avortements du deuxième trimestre. Trois arguments montrent qu'il s'agit de la méthode préférée par la plupart des femmes. Premièrement, l'utérus a évolué pour expulser son contenu au début ou à la fin de la grossesse, pas au milieu. L'induction du travail par avortement médicamenteux force donc l'utérus à accomplir une tâche pour laquelle il n'est pas préparé. Deuxièmement, les études de cohorte et les essais contrôlés randomisés des 30 dernières années ont montré que la technique par dilatation et évacuation est plus sûre et plus efficace que l'avortement médicamenteux, quel que soit l'abortif utilisé. Troisièmement, les principes éthiques de bienfaisance, d'autonomie et de justice exigent que cette technique soit proposée systématiquement par les gynécologues qui réalisent des avortements du deuxième trimestre. Sa disponibilité géographique inégale peut provenir d'un manque d'information, d'un manque des équipements ou de la formation nécessaires, ou encore d'un manque de motivation. Conformément aux principes de la médecine factuelle et de la bioéthique, ces obstacles à de meilleurs soins pour les femmes peuvent et doivent être levés.
Resumen
Décadas después de su lanzamiento, el procedimiento de dilatación y evacuación (D&E) aún no es ofrecido universalmente por ginecólogos que proporcionan servicios de aborto en el segundo trimestre. Tres líneas de evidencia señalan a la D&E como el método preferido para la mayoría de las mujeres. En primer lugar, el útero ha evolucionado para expulsar su contenido temprano y tarde en el embarazo, no a la mitad. Por tanto, la inducción del parto con el aborto por inducción del parto fuerza al útero a realizar una tarea para la cual no está diseñado. En segundo lugar, los estudios de cohorte y ensayos controlados aleatorizados en los últimos 30 años han mostrado sistemáticamente que la D&E es más segura y más eficaz que el aborto con medicamentos, sin importar el abortivo utilizado. En tercer lugar, los principios éticos de beneficencia, autonomía y justicia exigen que la D&E sea ofrecida rutinariamente por los ginecólogos que efectúan abortos de segundo trimestre. La desigualdad en la disponibilidad geográfica de la D&E posiblemente se deba a la falta de información, falta de capacitación y equipos necesarios, o falta de motivación. Según los principios de la medicina basada en evidencia y la bioética, estas barreras a una mejor atención para las mujeres pueden y deben superarse.
The choice of second trimester abortion method has been hotly – and widely – debated for three decades. The publication of a new Cochrane systematic review of second trimester abortion methodsCitation1 prompts reconsideration of the issue. In this essay, I will show how evolutionary biology, published evidence and the principles of bioethics converge on the conclusion that dilatation and evacuation (D&E) is the method of choice for most women.
Evolution of the uterus
Spontaneous abortion plays a fundamental role in the survival of our species. Although a wide range of fertilisations and implantations occur, most abnormal pregnancies are identified and rejected through spontaneous abortion, or miscarriage.Citation2 Miscarriage may be beneficial in other ways, such as spacing pregnancies further apart. In this respect, miscarriage may be an inborn form of family planning.
Most miscarriages occur early in pregnancy. Expulsion of the embryo in the first few weeks carries the least risk to the woman. (The efficiency of miscarriage is why medical abortion in early pregnancy is successful and complete in a high proportion of patients.) In contrast, were spontaneous abortion to occur primarily in mid-pregnancy, the risks of bleeding or infection would be higher. The uterus has evolved to recognise and eject abnormal pregnancies earlier, rather than later.
In the middle part of pregnancy, the uterus should retain its contents tenaciously. In the last phase of pregnancy, the uterus should expel the fetus when its prospects for survival outside are good. Evolutionary biology explains why labour induction methods are inferior to surgical abortion in the second trimester. Labour induction forces the uterus to perform a physiological function contrary to its role: to retain its passenger. As a result, to whip the uterus into action in the middle of pregnancy takes massive pharmacological stimulation. For example, because of the paucity of oxytocin receptors in the myometrium at this stage of pregnancy,Citation3 doses of oxytocin to accomplish abortion are much higher than those effective at the end of pregnancy.Citation4 Similarly, much higher doses of misoprostol are needed to effect labour in mid-pregnancy compared with late pregnancy; these high doses carry noxious side effects, including nausea, vomiting, diarrhoea and fever. In addition, the cervix stubbornly resists opening in the middle of pregnancy.Citation3 No abortifacient can readily overcome our genetic programming.
The evidence: comparative studies
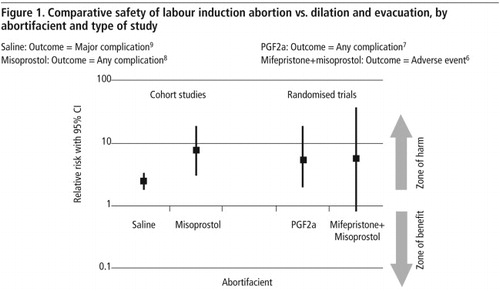
Clinical practice should reflect the best available evidence as well as the patient's preferences.Citation5 The superiority of D&E in both regards has been consistently documented for three decades. The recent Cochrane reviewCitation1 summarised the two randomised controlled trials, both of which found D&E to be safer than the abortifacients of their eras. Cohort studies have been consistent as well (). The abortifacients compared to D&E have included hypertonic saline, urea, prostaglandins, antiprogestins, and combinations of these. While modern abortifacient regimens such as mifepristone–misoprostol are superior to regimens of past decades, they are still inferior to D&E in safety and efficacy. Regardless of the abortifacient regimen, complications or adverse events are 2.6 to 7.9 times more common with labour induction abortion than with D&E ().Citation6–9 These are large and clinically important differences. Until and unless large clinical trials contradict the current best evidence, gynaecologists who ignore these disparities expose their patients to preventable complications.
Complications requiring hysterectomy denote serious morbidity. Cohort studies in the US from 1970 to 1978 examined the frequency of hysterectomy as treatment of abortion complications.Citation10 The frequency with labour induction abortion was 8.0 per 10,000 abortions. For D&E abortions at 13–15 weeks, the corresponding figure was 6.8 and at 16–20 weeks, 10.0. Because of small numbers of events, the confidence intervals around these proportions are wide and overlapping.
Nationwide surveillance of abortion mortality also provides insight into comparative safety. In the US from 1972–1987, the case-fatality rate associated with labour induction abortion was 7.1 per 100,000 procedures. The corresponding figure for D&E was 3.7.Citation11
The evidence: a “C” change in thinking
In the 1970s, women with access to D&E quickly abandoned labour induction in favour of this new method. While physicians liked the superior safety and efficiency of D&E,Citation12 women were drawn to the method for several non-medical “C” words: cost, convenience, comfort and compassion. As an outpatient procedure, D&E is generally less expensive, and a recent cost analysis confirms this advantage.Citation13 Indeed, D&E has practical advantages for developing countries, where hospital facilities are limited.Citation14 Since hospitalisation is not required, the abortion is generally more convenient for women. It is also more convenient for providers: the placement of osmotic dilators and timing of operation are elective and predictable, unlike the unpredictability of labour.
Labour hurts.Citation15–17 Since D&E avoids labour, women swap labour lasting hours to days for some cramping with osmotic dilators. Paracervical anaesthesia with bupivacaine for laminaria insertion may minimise cramping, since most swelling takes place in the first six hours. Pain serves important roles in human biology, such as signalling disease (e.g. frostbite or abscess). In the setting of abortion, pain has no biological value and should thus be avoided.
D&E is more compassionate as well. By the time a woman requests a second trimester abortion, she has usually suffered greatly. Studies have shown that women's negative reactions to abortion are directly related to their contact with the fetus.Citation18 D&E shifts the emotional burden of the procedure from the woman to the physician, and that is entirely appropriate. One of our most important roles as physicians is to ease suffering, both physical and emotional.
Neither mifepristone nor misoprostol is feticidal. Although the fetus usually succumbs to the trauma of labour, a small proportion of immature fetuses aborts with signs of life, despite assertions to the contrary.Citation16 These occurrences are emotionally difficult for the patient and her caregivers. According to federal law in the United States, such fetuses, independent of gestational age at expulsion, must be registered as live births, followed by a newborn death certificate. D&E obviates the possibility of signs of life and the need for feticidal injections.Citation16
An early cohort study compared the psychological reactions of women to D&E or labour induction abortion, and the findings were predictable.Citation19 Although women in the two groups were similar psychologically before the abortion, three weeks after the abortion the D&E patients scored significantly higher on the Profile of Mood States Scale for vigour. The labour induction group noted significantly more anger and depression. A lingering sense of guilt was reported by none of the D&E patients but by 24% of the labour induction group. The latter group reported that the induction termination hurt more than they had anticipated and that it was more like labour or the loss of a child. For these reasons, when women are offered a choice between D&E and labour induction, most choose the former.Citation6Citation7 When women were approached about participating in a randomised controlled trial of D&E vs. labour induction with mifepristone-misoprostol, D&E was especially preferred by those with fetal anomalies.Citation6
Ethics
Three fundamental principles of bioethics govern medical practice: beneficence, autonomy and justice.Citation20 Beneficence refers to the physician's obligation to provide the best care for the patient. As noted by Macklin:
“The principle of beneficence has always been central to medical practice, as it obligates physicians to recommend treatments or procedures likely to have the most beneficial health outcomes for their patients.” Citation21
The inverse is non-maleficence, or avoidance of harm to the patient, such as the psychological impact of labour induction abortion.Citation18Citation19 Based on the comparative studies, beneficence requires that D&E be recommended to most women. Conversely, not offering D&E because a gynaecologist is experienced and comfortable with labour induction contradicts this ethical principle.
By analogy, assume that a gynaecologist does not offer vaginal hysterectomy to her patients. Her explanation is that she is adept with abdominal hysterectomy. While this may be true, vaginal hysterectomy is the superior operation for womenCitation22 and, based on beneficence,Citation20Citation21 should be offered whenever appropriate.
Autonomy specifies that the woman be allowed to make her choice of treatment freely, without coercion, and with all material information necessary to make an informed decision. This principle requires that women requesting second trimester abortion be apprised of the acceptable methods and their comparative safety. Even if D&E were only similar to labour induction in safety and effectiveness, autonomy requires that D&E be discussed and offered to women seeking second trimester abortion.
Justice implies an equitable distribution of health care. Abortion services offered should be independent of age, race, marital status, ability to pay or geography. To quote Macklin:
“The principle of justice mandates that all individuals who need them should have equitable access to health services that are available to others. A precondition for access is information about the existence and nature of the services.” Citation21
Thus a gynaecologist who provides second trimester abortions should discuss and provide all safe, effective methods, not just local favourites.
The utilisation gap
In some parts of the world, only labour induction (or, worse, hysterotomy) is available to women seeking second trimester abortion. This deficiency may stem from several sources: lack of knowledge, lack of training and equipment, or lack of motivation.
The recent Cochrane reviewCitation1 capped three decades of consistent research, so claims of lack of awareness about comparative safety are no longer tenable. Lack of training and equipment is a more plausible explanation, but training can be readily obtained. Four to six weeks is adequate for residents. Even less may suffice for seasoned gynaecologists. Those of us who perform and teach D&E are happy to help colleagues learn. The instruments needed for D&E are few, inexpensive and durable (not disposable).
Personal motivation is likely the major obstacle to wider use of D&E. For example, “performing may be punishing,” or conversely, “not performing may be rewarding.”Citation23 Regarding performing, D&E is not pleasant for some gynaecologists.Citation16Citation19 This objection to D&E, however, suggests that aesthetics should influence surgical decision-making. Regarding not performing, writing orders in the chart, then leaving the patient and nurses to cope, frees the doctor to do other things. Another analogy may help: assume that a woman with a large, painful Bartholin's duct abscess in her vulva needs it incised and drained. Her gynaecologist, who finds the sight and smell of pus distasteful, admits the woman to the hospital for antibiotics instead of performing the appropriate outpatient surgical procedure.
Conclusion
In summary, the uterus evolved to eject its contents early and late in pregnancy, but not in the middle. Hence, bypassing labour is usually the appropriate way to empty the uterus mid-pregnancy. Comparative morbidity and mortality studies over three decades have found D&E superior to medical abortifacients, even modern ones. Finally, ethical principles require physicians to provide patients with the best therapy, let them choose freely among the options, and provide them equal access to best therapy. This means that D&E must be discussed and offered.
In settings with skilled gynaecologists, D&E should be the method of choice for most women; labour induction should also be an option for those who desire it. If the gynaecologist is unwilling or unable to perform the operation, then he or she is ethically obliged to refer the patient to someone who will. In locales without skilled gynaecologists, medical abortion should be the norm, since its singular advantage is that it requires no skill at all to start.
D&E has two prerequisites: an open cervix and an open mind. The uneven geographical availability of D&E today suggests that the latter prerequisite is the more difficult to achieve.
References
- P Lohr, J Hayes, K Gemzell-Danielsson. Surgical versus medical methods for second trimester induced abortion. Cochrane Database of Systematic Reviews. 2008; CD006714.
- Z Stein, M Susser, D Warburton, J Wittes, J Kline. Spontaneous abortion as a screening device. The effect of fetal survival on the incidence of birth defects. American Journal of Epidemiology. 102: 1975; 275–290.
- CH Hendricks. Physiology. GS Berger, WE Brenner, LG Keith. Second-trimester abortion. Perspectives after a decade of experience. 1981; John Wright PSG Inc: Boston, 69–78.
- J Owen, JC Hauth, CL Winkler, SE Gray. Midtrimester pregnancy termination: a randomized trial of prostaglandin E2 versus concentrated oxytocin. American Journal of Obstetrics and Gynecology. 167: 1992; 1112–1116.
- DL Sackett, WM Rosenberg, JA Gray, RB Haynes, WS Richardson. Evidence based medicine: what it is and what it isn't. British Medical Journal. 312: 1996; 71–72.
- DA Grimes, MS Smith, AD Witham. Mifepristone and misoprostol versus dilation and evacuation for midtrimester abortion: a pilot randomised controlled trial. British Journal of Obstetrics and Gynaecology. 111: 2004; 148–153.
- DA Grimes, JF Hulka, ME McCutchen. Midtrimester abortion by dilatation and evacuation versus intra-amniotic instillation of prostaglandin F2 alpha: a randomized clinical trial. American Journal of Obstetrics and Gynecology. 137: 1980; 785–790.
- AM Autry, EC Hayes, GF Jacobson, RS Kirby. A comparison of medical induction and dilation and evacuation for second trimester abortion. American Journal of Obstetrics and Gynecology. 187: 2002; 393–397.
- DA Grimes, KF Schulz, W Cates Jr, CW Tyler Jr. Mid-trimester abortion by dilatation and evacuation: a safe and practical alternative. New England Journal of Medicine. 296: 1977; 1141–1145.
- DA Grimes, ML Flock, KF Schulz, W Cates Jr. Hysterectomy as treatment for complications of legal abortion. Obstetrics and Gynecology. 63: 1984; 457–462.
- HW Lawson, A Frye, HK Atrash, JC Smith, HB Shulman, M Ramick. Abortion mortality, United States, 1972 through 1987. American Journal of Obstetrics and Gynecology. 171: 1994; 1365–1372.
- W Cates Jr, KF Schulz, DA Grimes, AJ Horowitz, FA Lyon, FH Kravitz. Dilatation and evacuation procedures and second trimester abortions. The role of physician skill and hospital setting. Journal of the American Medical Association. 248: 1982; 559–563.
- AA Cowett, RM Golub, WA Grobman. Cost-effectiveness of dilation and evacuation versus the induction of labor for second trimester pregnancy termination. American Journal of Obstetrics and Gynecology. 194: 2006; 768–773.
- W Cates Jr, KF Schulz, DA Grimes. Dilatation and evacuation for induced abortion in developing countries: advantages and disadvantages. Studies in Family Planning. 11: 1980; 128–133.
- L Mueller. Second-trimester termination of pregnancy: nursing care. Journal of Obstetrics Gynecology and Neonatal Nursing. 20: 1991; 284–289.
- S Lalitkumar, M Bygdeman, K Gemzell-Danielsson. Mid-trimester induced abortion: a review. Human Reproduction Update. 13: 2007; 37–52.
- S Grunstein, OE Jaschevatzky, A Shalit, Y Levy. Epidural analgesia in midtrimester abortion. International Journal of Gynaecology and Obstetrics. 14: 1976; 257–260.
- JB Rooks, W Cates Jr. Abortion methods: morbidity, costs and emotional impact. 3. Emotional impact of D&E vs. instillation. Family Planning Perspectives. 9: 1977; 276–277.
- NB Kaltreider, S Goldsmith, AJ Margolis. The impact of midtrimester abortion techniques on patients and staff. American Journal of Obstetrics and Gynecology. 135: 1979; 235–238.
- American College of Obstetricians and Gynecologists. Ethics in obstetrics and gynecology. Second edition, 2004; American College of Obstetricians and Gynecologists: Washington, D.C.
- R Macklin. Abortion controversies: ethics, politics and religion. DT Baird, DA Grimes, PFA Van Look. 1995; Blackwell Science: Oxford, 170–189.
- N Johnson, D Barlow, A Lethaby, E Tavender, E Curr, R Garry. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database of Systematic Reviews. 2006; CD003677.
- RF Mager, P Pipe. Analyzing performance problems, or you really oughta wanna. 1970; Fearon-Pitman Publishers, Inc: Belmont, California.