Abstract
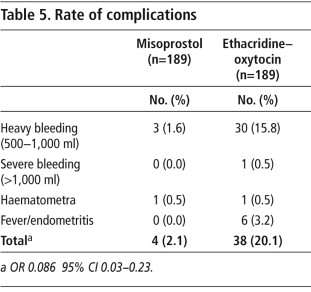
Outdated second trimester abortion methods are still being used in some countries, and very few studies have compared them to currently recommended methods. To this end, we studied the efficacy and safety of vaginal misoprostol used alone for abortions in 189 women at 13–20 weeks gestation, in 2004–2006. We also retrospectively collated similar data from an historical cohort of 189 women drawn consecutively and chronologically from hospital records from 2003–2006, also at 13–20 weeks gestation, who had had abortions with a combination of extra-amniotic 0.1% ethacridine lactate solution, oxytocin and sharp curettage. At 24 hours, misoprostol was 92.6% effective in inducing abortion versus 76.2% with the ethacridine lactate regimen (OR 4.2, 95% CI 2.3–8.0). The misoprostol cohort experienced fewer complications than the ethacridine cohort (4 vs. 38 cases, OR 0.086, 95% CI 0.03–0.23). We conclude that in the absence of mifepristone, misoprostol alone is preferable to the ethacridine regimen for the termination of pregnancy in the second trimester, because it works faster, has a higher success rate in a shorter period of time, and fewer complications.
Résumé
Des méthodes obsolètes d'avortement du deuxième trimestre sont encore utilisées dans certains pays en développement et très peu d'études les ont comparées avec des méthodes actuellement recommandées. Nous avons étudié l'efficacité et la sécurité du misoprostol administré seul par voie vaginale chez 189 femmes ayant avorté à 13–20 semaines de gestation en 2004–2006. Nous avons aussi examiné rétrospectivement des données similaires,obtenues de manière consécutive et chronologique à partir des dossiers hospitaliers, relatives à une cohorte historique de 189 femmes, qui avaient avorté en 2003–2006 avec une association d'éthacridine en solution à 0,1% par injection extra-amniotique, d'oxytocine et de curetage. Sous 24 heures, le misoprostol était efficace dans 92,6% des cas contre 76,2% avec le régime d'éthacridine (OR 4,2, IC à 95% : 2,3–8,0). Le fait que les femmes sous éthacridine aient mis plus longtemps à avorter était attendu. La cohorte sous misoprostol a enregistré moins de complications que la cohorte sous éthacridine (4 cas contre 38, OR 0,086, IC à 95% : 0,03–0,23). Nous en concluons que, faute de mifépristone, le misoprostol seul pour l'avortement médicamenteux au deuxième trimestre avec un régime bien accepté est préférable à l'association avec éthacridine car il agit plus vite, a un taux supérieur de réussite sur un délai plus court et présente moins de complications.
Resumen
En algunos países en desarrollo aún se utilizan métodos anticuados de aborto en el segundo trimestre, y muy pocos estudios los han comparado a los métodos recomendados actualmente. Con este fin, estudiamos la eficacia y seguridad del misoprostol vaginal solo utilizado para abortos en 189 mujeres con 13 a 20 semanas de gestación, entre 2004–2006. Además, recopilamos retrospectivamente datos de una cohorte histórica similar de 189 mujeres,seleccionadas consecutiva y cronológicamente de registros hospitalarios entre 2003–2006, con gestación de 13 a 20 semanas, que habían tenido abortos con una combinación de solución de etacridina extra-amniótica al 0.1%, oxitocina y legrado uterino instrumental. A las 24 horas, misoprostol fue un 92.6% eficaz contra un 76.2%con el régimen de etacridina (OR 4.2, 95% CI 2.3–8.0). La cohorte de misoprostol presentó menos complicaciones que la cohorte de etacridina (4 contra 38 casos, OR 0.086, 95% CI 0.03–0.23). Concluimos que en ausencia de mifepristona, misoprostol solo para la interrupción del embarazo con medicamentos en el segundo trimestre con el régimen recomendado es preferible al régimen de etacridina, porque funciona más rápido, tiene una tasa de eficacia más alta, en un plazo más corto, y menos complicaciones.
Since 1973 Cuba has provided safe and legal pregnancy termination at women's request.Citation1 Abortion rates in Cuba have declined with increasing contraceptive use from 40–50 abortions per 1,000 women of reproductive age in 1980–90 to about 20 per 1,000 in 2005. Most abortions occur in the first trimester, and a small proportion in the second trimester.Citation2 For the last several decades and until very recently, the combination of ethacridine lactate, oxytocin and sharp curettage has been the standard procedure for abortions between 13–20 weeks of pregnancy in Cuban hospitals.Citation3 Ethacridine lactate (also known as Rivanol) is an organic compound based on acridine. Its primary use is as an antiseptic in solutions of 0.1%. When used as an agent for second trimester abortion, it is thought to spur endogenous prostaglandin production.Citation3 Up to 150 ml of 0.1% ethacridine is instilled extra-amniotically, using a Foley catheter and usually after 20–40 hours, labour ensues.
The World Health Organization (WHO) recommends the use of the antiprogestin, mifepristone, followed by misoprostol, as the medical method for second trimester abortion.Citation4 Due to limited access to and cost of mifepristone in many developing countries, including Cuba, second trimester abortions are often performed by the administration of misoprostol alone, using a variety of doses and routes.Citation5–7 WHO does not recommend Rivanol.
The Latin American Federation of Obstetrics and Gynaecology Societies (FLASOG) published a guideline in 2007Citation8 for obstetric and gynaecological uses of misoprostol that recommends the following misoprostol regimens based on the concept of the minimum effective dose: 400 mcg misoprostol at gestations of 13–15 weeks, and 200 mcg at 16–20 weeks. The initial dose is repeated if there has been no response at 6–12 hours. Should there still be no response at 24 hours, the initial dose is doubled (800 mcg at 13–15 weeks, and 400 mcg at 16–20 weeks), and repeated at 8-hourly intervals if there is no evidence of abortion, up to a maximum of four additional doses. Lower doses of misoprostol alone are required as pregnancy advances in the second trimester.Citation9
We decided to test this misoprostol regimen and to compare its efficacy and safety with an ethacridine lactate regimen which had been used in 2003–2006 in a cohort of women.
Methods
We conducted a prospective study of a cohort of patients who received vaginal misoprostol for the termination of pregnancy in the second trimester, using the FLASOG-recommended second trimester regimens, and compared them with an historical group of patients who received extra-amniotic ethacridine, oxytocin and sharp curettage.
In order to achieve an 80% power to detect a difference of 10% or more in the efficacy of the two methods at 48 hours, based on available efficacy estimates of 98% (ethacridine/oxytocin) and 90% (misoprostol) respectively, a minimum of 139 cases were needed in each group (n=278). To permit stratification by gestational age, it was desirable to increase the sample size by 25%, requiring 189 in each group.
The inclusion criteria for the misoprostol cohort included women aged 18 years and older who requested voluntary termination of pregnancy at 13–20 weeks gestation. The exclusion criteria were intolerance or allergy to misoprostol, haemoglobin below 10.0 g/l, history of cerebral or cardiovascular disease, with blood pressure above 160/90 Mm Hg, diabetes mellitus, previous uterine bleeding, or symptomatic reproductive tract infection.
In the initial consultation, women were informed of the study, gestational age was confirmed by transvaginal ultrasound and women were screened for eligibility for the misoprostol regimen. They were informed that in case of failure, sharp curettage, the standard surgical procedure in Cuba, would be carried out. Symptoms, signs and complementary examinations were described. Written, informed consent was obtained from eligible women willing to participate in the study. No economic incentives were involved.
The historical comparison group of 189 women who had had an abortion with the ethacridine regimen were drawn consecutively and chronologically from hospital records from January 2003–December 2006. Preference for ethacridine among both providers and women decreased substantially after the introduction of misoprostol in Cuba, and is practically no longer used, which is why it was not possible to do a prospective ethacridine arm.
All patients were hospitalised for the duration of the abortion following the standards of the Cuban Ministry of Health.Citation3 Blood samples were obtained to determine haemoglobin, hematocrit, complete blood count, basic STI serology, HIV, blood group and Rh factor, before the beginning of the procedure. Vaginal flora were cultured for symptoms of sexually transmitted infections necessitating treatment. In order to reduce the discomfort of side effects, both an anti-emetic and analgesics were provided before each dose of misoprostol.
Outcomes of interest included complete or incomplete abortion confirmed by ultrasound within 24 hours, without subsequent curettage for suspicion of retained products; the need for a surgical procedure to terminate the pregnancy, failure to expel the products of conception by 24 hours, or a severe complication that required emergency uterine evacuation.
Misoprostol protocol used
For patients at 13–15 weeks of pregnancy, 400 mcg (two tablets, 200 mcg each) were moistened with 2–3 drops of water and placed, one on each side of the vaginal fornix. This was repeated every 8 hours up to completing 3 doses. If abortion had not begun within 24 hours, the dosage was doubled and the procedure repeated.
For patients at 16–20 weeks of pregnancy, one 200 mcg tablet was similarly prepared and placed, repeating the dosage every 8 hours. If there was no abortion activity in 24 hours, the same regimen was repeated.
For those without complete expulsion after 72 hours, curettage was performed, taking advantage of the dilation due to misoprostol.
Ethacridine + oxytocin protocol used
Following Cuban standards and protocols,Citation3 an antiseptic solution was applied in the vagina and the cervix prior to visual inspection of the cervix with a speculum. The anterior lip of the cervix was clamped and a probe of Nelaton of 14 or 16 mm was introduced among the membranes and the uterine wall, as high as possible, nearly at the base of the uterus.
Using a probe, 100 cc of a solution 0.1% of ethacridine lactate was injected slowly, closing the distal extreme of the probe with a thread in order to prevent the solution from leaking to the exterior. A total dose of 100 ml was administered to all patients. Gauze was placed vaginally to preclude the probe sliding through the cervix. Efforts were made to prevent reflux of the injected solution.Citation3 An infusion of oxytocin (20 IU in 500 cc of dextrose to pass in 8 hours) was administered during the first 24–36 hours, followed by expectant management. The national norms in Cuba call for routine sharp curettage with this protocol. Before 2005, once the products of conception were expelled, instrumental curettage was carried out in almost all cases; after 2005, physicians began to assess the need for this by ultrasound in 2005.
Clinical progress in both cohorts was monitored regularly by medical and nursing professionals in the abortion service unit in accordance with institutional protocols.Citation3 If expulsion did not occur within 24–36 hours, women in the ethacridine–oxytocin cohort were given the option of repeating the regimen, using misoprostol or having sharp curettage. If any of these failed, a mini-caesarean section (hysterotomy) was conducted. For comparison's sake, we only considered for the statistical analysis what happened in each group within the first 24 hours of treatment. However, we also report the outcomes and procedures for women in both groups whose abortions were not complete by 24 hours.
Statistical analysis
Quantitative analyses were conducted with SPSS 14.0. The two cohorts were assessed on socio-demographic and reproductive characteristics to assure comparability. Student t-tests were used for detecting differences between means, and odds ratios were calculated to identify significant differences between proportions. Using an alpha of 0.05, 95% confidence intervals were calculated for all point estimates. This protocol was reviewed and approved by the Commission of Ethics and of the Scientific Council of the Institution.
Results
Characteristics of participants
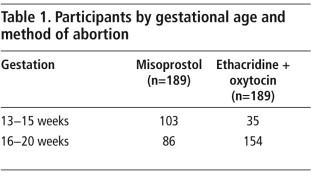
For the period of the misoprostol study, January 2004–December 2006, 470 eligible women presented to the facility for second trimester pregnancy termination. Among those eligible to participate, 189 women with pregnancies of 13–20 weeks chose misoprostol. Table 1 shows the number of women treated by length of pregnancy and method.
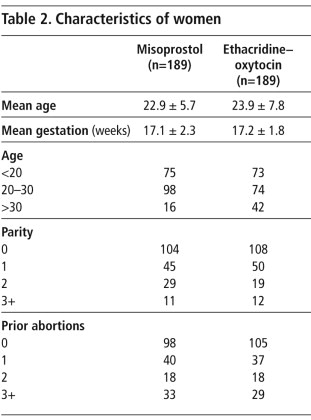
In both groups, the women tended to be young and nulliparous, with similar reproductive histories and mean weeks of pregnancy (Table 2). They were comparable as regards age, number of children, education level, ethnic background and previous abortions, rendering them appropriate for comparison.
Efficacy of the two methods
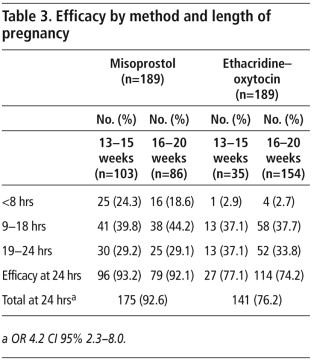
In the misoprostol cohort, the regimens used led to as high an efficacy in the 16–20 week group as in the 13–15 week group (92.1% versus 93.2%, p=0.79).
A comparison of the efficacy of the two methods up to 24 hours after first treatment (Table 3) found that at all three stages within the first 24 hours, misoprostol was effective earlier in more women than ethacridine–oxytocin (OR 4.2 95% CI 2.3–8.0). In the two 13–15 week cohorts, the efficacy of misoprostol was double (OR 2.0 95% CI 1.1–11.0), and in the two 16–20 week cohorts, it was almost triple (OR 2.9 95% CI 1.2–7.0).
Abortions completed after 24 hours: procedures used
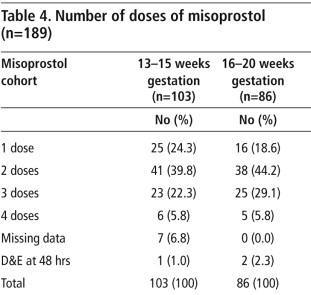
The number of doses taken by the women in the misoprostol cohort is shown in Table 4, along with the numbers that underwent D&E at 48 hours.
In total, 62 women in the ethacridine–oxytocin group were diagnosed with incomplete abortion at different stages after 24 hours, and all but one were treated with sharp curettage. Sixteen women received additional treatment interventions at 24 hours. Four women who had had a repeat ethacridine instillation had to have a hysterotomy. The decisions as to when and how to manage the patients were made by the provider in charge at the time, not the researchers.
We found no association between number of weeks of pregnancy and the mean dose of oxytocin. Women at 13–15 weeks of pregnancy received an average of 98.3 IU ± 56 (SD), while those at 16–20 weeks received 93.5 IU ± 48 (SD). There was no association between cumulative dose and abortion outcome. Among the four women who underwent hysterotomy, the mean dose of oxytocin was 120 IU ± 32 (SD). The risk of aqueous poisoning increases with prolonged oxytocin infusions, but in this group no cases of aqueous poisoning were recorded. Avoidance of prolonged use of oxytocin is, however, always preferable.Citation10
Complications
This study could not compare complication rates per se, so the findings must be viewed with caution, especially given the small sample sizes. Moreover, measurement of haemorrhage was based on differing criteria; thus, severity of bleeding in the misoprostol cohort was defined as “more than two pads totally soaked in one hour”, while in the historical cohort it was estimated visually.
However, the misoprostol cohort experienced fewer complications overall than the ethacridine–oxytocin group (2.1% vs. 20.1% OR 0.086 95% CI 0.03–0.23) (Table 5). The biggest difference was in the number of women who experienced heavy bleeding – three of 189 women with misoprostol versus 30 of 189 women with ethacridine–oxytocin. In addition, six women in the ethacridine–oxytocin group experienced a febrile syndrome indicative of possible infection compared to none using misoprostol.
Symptoms and side effects
Abdominal cramping and bleeding are misoprostol's main mechanisms of action, not side effects. In 45.5% of the 189 women using misoprostol, vaginal bleeding was greater than menstruation. For the rest, bleeding was described as the same or less than with menstruation. Abdominal cramping was reported by 92.1% of the women: 7.9% reported no pain and for 40.2% the pain was less than or equal to that experienced during menstruation. For 29.1% the cramps were slightly stronger than menstrual cramps, while for 22.8% they were at least twice as strong as with menstruation.
All the side effects observed among the women using misoprostol are known and were described by the women as tolerable. None abandoned the method because of them. Transient chills and fever during the first eight hours were common, affecting 47% and 14.8% respectively, and diminished to low levels by the end of the first 24 hours (data not shown). Nausea (28.5%), vomiting (19.6%) and diarrhoea (10.5%) were experienced by a small proportion and also declined by 24 hours and with subsequent dosages.
The side effects with ethacridine–oxytocin were not systematically recorded or in a comparable format, so we could neither analyse nor compare them.
Acceptability
Women in the misoprostol arm were asked if they would use misoprostol again if the need for second trimester pregnancy termination arose in future. The majority (75.1%) said they would choose it again. Those that would not wish to use it again pointed to the bleeding and pain, and doubts about its effectiveness, as their main hesitations. The ethacridine–oxytocin cohort were not asked this question. However, the fact that this procedure has almost disappeared in Cuba with the advent of misoprostol use in the second trimester is a strong indication of preference for misoprostol when these are the only two choices.
Limitations of the study
The use of an historical comparison group limited the comparability of findings. Since the ethacridine–oxytocin cohort was not designed as a study cohort, there was less standardisation, treatment ran for different lengths of time, there were different degrees of method choice for the women, and they were not asked about side effects or future preferences.
No standardised operational definitions were employed to measure clinical outcomes in the ethacridine–oxytocin cohort, so some slight measurement variations may have occurred in outcomes of interest. Moreover, in the ethacridine–oxytocin cohort, some women were given the option of misoprostol if the ethacridine–oxytocin had not succeeded at 24–36 hours, so that the only truly independent comparative efficacy rates were those within the first 24 hours. Although a randomised, controlled trial would obviously have been preferable, the findings remain relevant for countries still using ethacridine widely.
Discussion
This study shows what has long been argued: that there are better ways than ethacridine–oxytocin to provide second trimester abortion. Although the study design could not compare method effectiveness after 24 hours, misoprostol was more likely to yield complete expulsion within the first 24 hours (92.6% vs. 76.2% OR 4.2 95% CI 2.3–8.0). Whether or not the rates of complete abortion were more similar after 24 hours is unknown. However, it can safely be assumed, given the abandonment of ethacridine in Cuba, that longer inpatient stays due to longer induction-to-abortion times are less acceptable to both women and providers, and are clearly more costly for both women and health systems, especially in a context of scarce resources.Citation11–14
As in most studies of misoprostol,Citation15 we found minimal discomfort with the misoprostol method, and high acceptability. This finding is all the more substantive given that a significant proportion of the women in the misoprostol cohort (48.2%) had had a prior first trimester surgical abortion using electric vacuum aspiration with general anaesthesiaCitation3 as a frame of reference.
Conclusion
We conclude that misoprostol alone for second trimester termination of pregnancy, using a graduated dose of vaginal misoprostol with increasing gestation, is preferable to ethacridine–oxytocin, because it works faster, has a higher success rate in a shorter period of time, and fewer complications due to heavy bleeding and fever.
For medical abortion where mifepristone is unavailable, we recommend the incorporation of misoprostol alone into clinical guidelines for the medical termination of pregnancy as a first-line option in the second trimester. As misoprostol has become the preferred second trimester method in the Cuban context, we can report that ethacridine for second trimester terminations will no longer be recommended in the upcoming revision of the national guidelines in 2009.
Acknowledgements
We wish to acknowledge the generosity of the women, who participated in this study, our Cuban colleagues who rendered a high quality of care, as well as Ann Leonard, Traci Baird, Delphine Andrews and Bill Powell of Ipas, for providing valuable technical review of the manuscript.
References
- E Cabezas. Salud reproductiva; aborto provocado. O Rodríguez Armas, R Santiso Galvez, V Calventi. Ginecologia Fertilidad Salud Reproductiva. 1996; FLASOG: Caracas, 691–724.
- Estadisticas de Salud de Cuba 1996–2002. Dirección Nacional de Estadística del Ministerio de Salud Pública de Cuba. At: <www.dne.sld.cu/desplegables/indexcuba.htm. >.
- Manual de Diagnóstico y Tratamiento en Obstetricia y Perinatología. 1997; Ciencias Médicas: La Habana, Cuba, 520.
- World Health Organization. Safe Abortion: Technical and Policy Guidance for Health Systems. 2003; WHO: Geneva, 112.
- SW Ngai, OS Tang, PC Ho. Prostaglandins for induction of second-trimester termination and intrauterine death. Best Practice & Research Clinical Obstetrics & Gynaecology. 17(5): 2003; 765–775.
- JM Dodd, CA Crowther. Misoprostol versus cervagem for the induction of termination of pregnancy in the second and third trimester: a systematic review. European Journal of Obstetrics & Gynaecology & Reproductive Biology. 125: 2006; 3–8.
- KS Wong, CSW Ngai, AYK Wong. Vaginal misoprostol compared with vaginal gemeprost in termination of second trimester pregnancy: a randomized trial. Contraception. 58: 1998; 207–210.
- A Velazco, R Gomez Ponce de Leon. Therapeutic abortion. A Faúndes. Obstetric and Gynecological Uses of Misoprostol. 2007; FLASOG. 59–76.
- C Guix, M Palacio, F Figueras. Efficacy of two regimens of misoprostol for early second-trimester pregnancy termination. Fetal Diagnosis and Therapy. 20: 2005; 544–548.
- C Li, W Wang, S Summer. Molecular mechanisms of antidiuretic effect of oxytocin. Journal of American Society of Nephrolology. 18: 2007; 3067–3077.
- Alan Guttmacher Institute. Sharing responsibilities: women, society and abortion worldwide. 1999; Alan Guttmacher Institute: New York.
- J Benson. Evaluating abortion-care programs: old challenges, new directions. Studies in Family Planning. 36: 2005; 189–202.
- K Rogo. Improving technologies to reduce abortion-related mobidity and mortality. International Journal of Gynecology and Obstetrics. 85(1): 2004; 73–82.
- D Grimes, J Benson, S Singh. Unsafe abortion: the preventable pandemic. Lancet Sexual and Reproductive Health Series. 268: 2006; 1908–1919.
- PC Ho, P Blumenthal, K Gemzell-Danielsson. Misoprostol for the termination of pregnancy with a live fetus at 13 to 26 weeks. International Journal of Gynecology & Obstetrics. 99: 2007; 178–181.