Abstract
Thailand in 2000 and Ghana in 2001 initiated cervical cancer prevention programmes using a single-visit approach with visual inspection with acetic acid (VIA) with cryotherapy for pre-cancerous lesions. This service was integrated into existing reproductive health services, provided by trained nurses. The providers maintained a high level of competence and performance, including after the withdrawal of external funding. In Ghana, independent co-assessments revealed a high level of agreement in diagnosis between providers and a Master Trainer. In Thailand, high quality performance was associated with quality assurance mechanisms such as peer feedback and review of charts and service statistics. Provider performance was maintained at a high level in both countries: an average of 74% of providers from both countries met 85% or more of performance standards. The successful transition from a demonstration project to a national programme in Thailand was dependent on a strong commitment from government health bodies and health professionals. In contrast, the lack of health infrastructure and political will has prevented scale-up to a national programme in Ghana. However, this study shows that a single-visit approach with VIA and cryotherapy is programmatically feasible and sustainable and should be considered in national investments to control cervical cancer. © Reproductive Health Matters
Résumé
La Thaïlande en 2000 et le Ghana en 2001 ont lancé des programmes de prévention du cancer du col de l’utérus utilisant l’approche de visite unique avec inspection visuelle après application d’acide acétique (VIA) et cryothérapie des lésions précancéreuses. Ce service a été intégré dans les services existants de santé génésique et assuré par des infirmières formées. Les prestataires ont maintenu un niveau élevé de compétence et de performance, même après le retrait du financement extérieur. Au Ghana, des évaluations indépendantes conjointes ont révélé un excellent niveau d’accord sur le diagnostic entre les prestataires et le formateur principal. En Thaïlande, la valeur des performances a été associée à des mécanismes d’assurance qualité comme les informations des pairs et l’examen des tableaux et des statistiques de service. Les deux pays ont maintenu les performances des prestataires à un niveau élevé : en moyenne, 74% des prestataires des deux pays ont satisfait à 85% ou plus des normes de performance. La transition réussie d’un projet de démonstration à un programme national en Thaïlande est due au ferme engagement des organes sanitaires gouvernementaux et des professionnels de la santé. Par contre, au Ghana, le manque d’infrastructure et de volonté politique a empêché le passage au niveau national. Néanmoins, cette étude montre que l’approche de visite unique avec VIA et cryothérapie est faisable et viable, et qu’elle devrait être envisagée dans les investissements nationaux pour lutter contre le cancer du col de l’utérus.
Resumen
En Tailandia, en el año 2000, y en Ghana, en el 2001, se iniciaron programas para la prevención del cáncer cervical utilizando la estrategia de una sola consulta con inspección visual con ácido acético (IVAA) y crioterapia para lesiones pre-cancerosas. Este servicio fue integrado a los servicios establecidos de salud reproductiva, proporcionados por enfermeras capacitadas, quienes mantuvieron un alto nivel de aptitud y desempeño en el trabajo, aun después de terminado el financiamiento externo. En Ghana, co-evaluaciones independientes revelaron un alto nivel de consenso entre los prestadores de servicios y el capacitador principal en cuanto a los diagnósticos. En Tailandia, el desempeño de alta calidad estaba asociado con los mecanismos de garantía de la calidad como la retroalimentación de pares y la revisión de expedientes y estadísticas de servicio. El desempeño de los prestadores de servicios permaneció en un alto nivel en ambos países: un promedio del 74% de los prestadores de servicios de ambos países cumplió con el 85% o más de las normas de desempeño. La transición exitosa de un proyecto de demostración a un programa nacional en Tailandia dependió de un compromiso sólido por parte de los organismos sanitarios gubernamentales y los profesionales de la salud. Por contraste, la falta de infraestructura de salud y voluntad política ha impedido la ampliación a un programa nacional en Ghana. Sin embargo, este estudio muestra que la estrategia de una sola visita con IVAA y crioterapia es factible y sostenible en términos programáticos y debería considerarse en inversiones nacionales para controlar el cáncer cervical.
In 2002, 83% of the more than 493,000 new cases of cervical cancer and 85% of all cervical cancer deaths globally occurred in developing countries.Citation1 This high burden of disease is due to the lack or inefficiency of cytology-based screening programmes that have significantly reduced mortality due to cervical cancer in deve loped countries. However, effective, practical and affordable alternative screening approaches do exist.
Visual inspection using acetic acid (VIA) is one of the most promising alternatives to cytology-based screening. The sensitivity of VIA is equivalent to or better than that of a Papanicolaou (Pap) smear, although its specificity is lower.Citation2 VIA is effective in detecting pre-cancerous lesions and provides immediate results so the woman can be linked to treatment or referralCitation3–8 using a single-visit approach. This approach was shown to be safe, acceptable and feasible in demonstration projects in Ghana and Thailand.Citation4,8,9 In addition, a one-or two-visit screening and treatment approach is the most cost-effective approach for reducing lifetime risk of cervical cancer.Citation10
Internationally recognised manuals and resources provide programmatic guidance for roll-out of cervical cancer prevention programmes using a single-visit approach.Citation11Citation12 A recent study showed a significant decline in cervical cancer incidence and mortality after seven years in a population receiving one round of VIA screening and concluded that “good training and sustained quality assurance” must be present to achieve such results.Citation13 Systems for ensuring good training and quality assurance are indeed critical in this regard, but these systems, and their impact on provider performance, have not yet been described in the literature.
Jhpiego – an affiliate of Johns Hopkins University – and its partners in the Alliance for Cervical Cancer Prevention (ACCP), together with the governments of Thailand and Ghana, introduced a single-visit approach in Ghana and Thailand as a part of demonstration projects conducted from 2000 to 2004.Citation14
Human and material resources for health are scarce in Ghana and infrastructure is poor. Crude incidence rates of cervical cancer are higher than in the rest of West Africa (19.4 vs. 17.8 per 100,000 women).Citation15 In contrast, Thailand is undergoing rapid development and has a relatively strong health infrastructure. Thailand also has a higher incidence rate of cervical cancer than the rest of the region (19.2 vs. 15.9 per 100,000 for southeast Asia).Citation16 It is estimated that more than 2,000 Ghanaian women and 6,200 Thai women per year develop cervical cancer.Citation15Citation16 Neither country had implemented a large-scale cervical cancer screening programme before the ACCP demonstration projects.
When external funding for the demonstration projects ended in 2004, Jhpiego sought to determine how well the programmes continued to perform by measuring: (1) the maintenance of quality of services and provider performance in both countries, and (2) screening coverage in Thailand.
Methods
Because of differences between Ghana and Thailand in factors such as health infrastructure, available resources, policy, and integration of cervical cancer prevention services within the public health system, parts of the study methodology differed. Therefore, the methods and findings are presented separately for each country.
Thailand
A district was eligible for inclusion in the study if it had been offering cervical cancer prevention services for at least six months as of December 2005. Fifty-four of 83 eligible districts in nine provinces were selected, using a systematic random sampling approach based on the length of time they had been offering services. Length of time was chosen as a factor because it corresponds to the “generations” of service providers who have been trained. Two districts were later excluded from the sample because the study was pre-tested in those districts. Another three districts were lost to the study – two stopped providing VIA services and one hospital director declined to participate. Within the 49 districts that were enrolled until the end of the study, 66 health facilities (including every district hospital) were visited and every provider who was actively providing cervical cancer prevention services (n=113) was sampled.
Data were collected by ten Thai research assistants who underwent training on the research protocol and completed a three-day course to standardise their skills. All research assistants were nurses with 3–5 years of experience providing VIA and cryotherapy, and all were trainers for the national programme. The research assistants interviewed the service providers and their supervisors and used performance standards checklist to observe the providers performing VIA and cryotherapy. These checklists, based on the national training programme, included all tasks necessary for correctly providing VIA and cryotherapy, and all providers had been trained using these performance standards.
Screening coverage was calculated using Thailand’s Cervical Pre-Cancer Information System (CPIS), which collects routine health information on screening and treatment using VIA.
Data quality in Thailand was ensured by a quality assurance advisor (author WE), double entry of data, and two monitoring visits by a representative of the Bill and Melinda Gates Foundation, who provided additional suggestions to strengthen data quality systems. Analysis of performance standards data was conducted using SPSS version 15.0 software. The Chi-square or Fisher exact test was used to compare groups where appropriate. The data on screening coverage in Thailand were obtained from CPIS, with a secondary analysis conducted using Microsoft Excel. Ethical oversight was provided by the Western Institutional Review Board (WIRB) and the Ethical Review Committee for Research in Human Subjects, Ministry of Public Health (MOPH), Thailand.
Ghana
The study population in Ghana consisted of all 13 nurses who were providing VIA services at the three facilities where the single-visit approach was being implemented. Six providers were at Ridge Hospital, four at Kumasi South Hospital, and three at Amasaman Health Center. Nine of the nurses were trained in 2001, and four in 2004.
The Ghanaian research team consisted of a nurse and a doctor. Both had more than five years experience with single-visit approach service provision and training and were Master Trainers. The team had been involved with training the providers they were co-assessing; this was unavoidable due to the very limited number of qualified trainers available in the country.
The research team interviewed the service providers and used a performance standards checklist to observe the providers performing VIA and cryotherapy. The checklist was essentially the same as that used in Thailand, but a team of Ghanaian experts had slightly modified it for use in Ghana. Supervisors were not interviewed in Ghana because they had not been trained or supported to perform supervision of VIA and cryotherapy services.
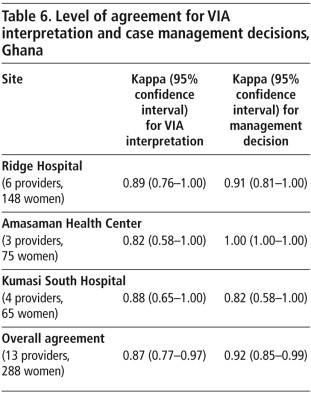
The smaller number of providers in Ghana allowed for verification of the providers’ diagnosis and case management decisions for VIA through independent co-assessment of 15–25 women per provider. Both the provider and the nurse Master Trainer, whose decision served as the reference standard, assessed the women and came to independent conclusions on the diagnosis and case management decision for each woman. These data were then analysed using the Kappa statistic to determine the level of agreement.
Analysis of performance standards data in Ghana was conducted using SPSS version 15.0 software. The Chi-square or Fisher exact test was used to compare groups where appropriate. Kappa analysis of the co-assessments was conducted in SAS version 9.1. In Ghana, the Institutional Review Board for the School of Medical Sciences for Kumasi University waived ethical oversight to WIRB. Informed consent was obtained from all providers before beginning the interviews or observations.
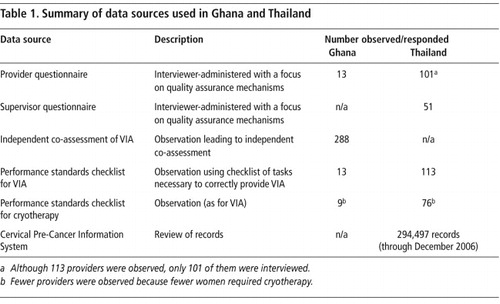
Data were collected from December 2005 to March 2006 in Thailand, and from April to December 2006 in Ghana. Table 1 presents a summary of the data sources in both countries.
Results
Provider performance and maintenance of quality
The performance of providers in Thailand and Ghana was assessed using VIA and cryotherapy performance standards. All tasks for each performance standard had to be correctly performed before a standard was considered to be met. If 85% of the standards were met, the provider was considered to be near-perfect, and if 100% of the standards were met the provider was considered to be perfect.
In Thailand, 35% of providers achieved a perfect score and 36% achieved a near-perfect score. Providers in Ghana performed at an even higher level, with 85% considered perfect and the remaining 15% near-perfect.
Thailand
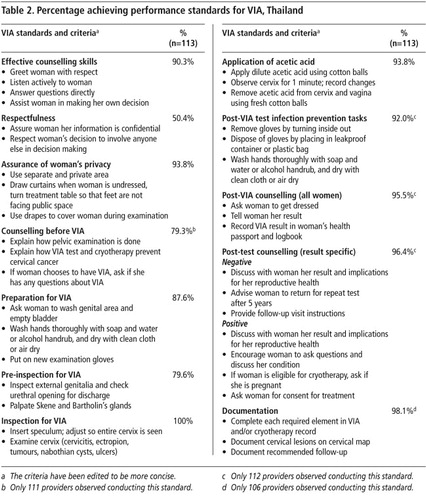
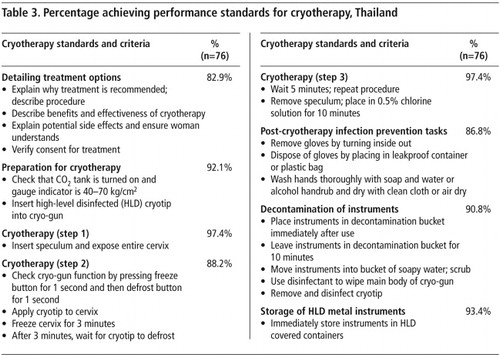
Tables 2 and 3 show how providers in Thailand performed on each standard. The lowest non-clinical achievement (50%) was in relation to respectfulness. This relatively low achievement is thought to have been because allowing others to be involved in decision-making was incompatible with the flow of service provision and the emphasis on “see and treat”.
The standards achieved in relation to clinical decision-making and management were generally very high. The clinical standard with the lowest achievement was for pre-inspection for VIA, although 80% of providers achieved that standard.
During their training, providers and supervisors are taught a number of performance enhancing strategies such as co-assessment, peer feedback, use of job aides, etc. Out of a diverse range of quality assurance mechanisms identified by providers, several quality assurance mechanisms emerged as having a significant effect on provider performance.
Table 4 presents three quality assurance mechanisms that appeared to be among the factors that boosted near-perfect performance to perfect performance. These were managerial rather than clinical in nature. The findings suggest that supportive supervision and job aides may also contribute to high performance in Thailand.
Ghana
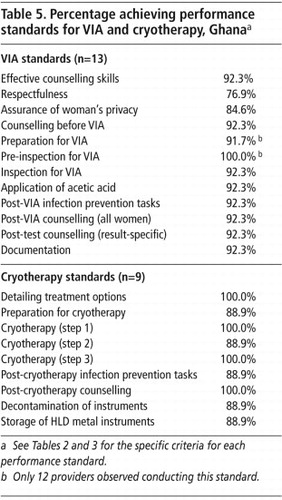
Table 5 shows how the Ghanaian providers performed on each standard. As in Thailand, the lowest achievement in Ghana (77%) was observed for the pre-VIA standard for respectfulness.
Provider performance at each of the three sites in Ghana was independently co-assessed by a Master Trainer. The results were compared and the level of agreement between the two assessments was measured. Table 6 shows the level of agreement presented as a Kappa statistic for each facility and for all facilities combined. In general, the closer the Kappa is to 1.0, the higher the level of agreement.
For both the diagnosis of the cervix and the case management decision, there was a high level of agreement in diagnosis between the providers’ assessments and those of the Master Trainer. The Kappa statistics ranged from 0.82 to 1.0; even the lowest figure falls into the category labelled by Landis and Koch as “almost perfect”.Citation17
Screening coverage
Thailand
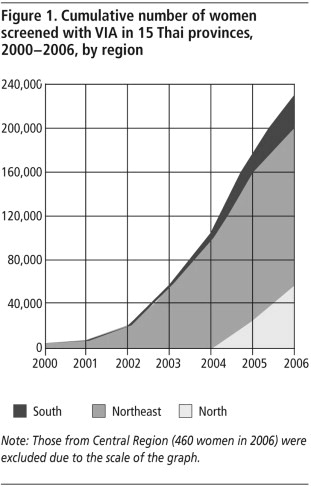
Before the year 2000, cervical cancer screening programmes were unorganised in Thailand. In 2003, provincial health authorities had a choice to implement cervical cancer screening with VIA alone, VIA and Pap smear, or only Pap smear.Footnote* At the end of 2006, 15 of the 75 provinces in Thailand elected to implement single-visit approach programmes, and an additional four provinces have adopted this approach since then. These provinces are not reported on, since at the time of the analysis they did not have complete data in the CPIS.
The CPIS records district service statistics of 2–4 years in scope with the aim of measuring all the accomplishments of the national VIA-based cervical cancer prevention programme.Footnote† However, district reporting is of variable consistency and completeness, making the CPIS useful but not definitive.
According to the CPIS, between 2000 and 2006, 450 providers and 77 trainers were trained in the 15 provinces of Thailand that have adopted VIA. By the end of 2006, 294,497 total VIA screenings were performed and 233,082 women had been screened at least once. The providers screened an average of 227 women per year (in addition to all their other normal service provision). In the provinces included in CPIS, providers had screened 10–45% of eligible women using VIA, with an average coverage rate of 25%. Some districts had reached up to 70% of eligible women. The highest coverage was found in Pon Sai District of Roi Et Province, where VIA was introduced in March 2002.
presents the cumulative number of women screened with VIA from 2002–2006 in the 15 Thai provinces. Cumulative coverage is defined as the percentage of eligible women screened using VIA over the total number of eligible women in the province.
Ghana
Screening coverage was not calculated in Ghana because accurate information about the target population was not available. However, a review of the registers at the three Ghanaian health facilities showed that more than 19,000 women were screened by 13 providers from 2002 to 2006.
Return visits
Thailand
According to Thai policy, VIA negative women are counselled to return after five years for re-screening, and VIA positive women who have undergone cryotherapy are counselled to return after one year. CPIS data for Roi Et Province (the province implementing VIA the longest) were reviewed to gain insight into how many women returned for their follow-up visit. Although the timing of the visit (i.e. how long the women waited to return) was not analysed, close to 8,000 women returned for a follow-up visit between 2005 and 2006 (5–6 years following the onset of the programme). The proportion of women returning for a follow-up visit out of all women in Roi Et Province progressively increased from 0.3% in 2000 to 49.3% in 2006.
A study is currently underway to track the clinical outcomes of the original cohort of women screened in Roi Et Province and provide more information on health outcomes and the timing of return visits.
Discussion
The single-visit approach for secondary prevention of cervical cancer is fully established as a low-cost and cost-effective intervention that benefits individual women and improves public health outcomes. This study provides important insight into the maintenance of quality in two such programmes.
Provider performance was maintained at a high level in both Ghana and Thailand: an average of 74% of providers from both countries met 85% or more of performance standards. Providers in Ghana achieved, on average, an almost perfect level of agreement with a Master Trainer regarding diagnosis. This was true even when providers had been trained up to seven years before the assessment or when providers had been trained second generation, i.e. they were trained by national trainers rather than by the original programme.
The most frequent instances of low performance were related to counselling rather than clinical performance, and are not likely to result in misdiagnosis or under-treatment of women. However, counselling skills are important to ensure that informed consent is obtained for cryotherapy and that women return for follow-up and other key services. These findings indicate the need for increased emphasis on counselling training, particularly in Thailand.
The high achievement in provider performance is relevant to the scale-up of cervical cancer screening and treatment programmes using VIA. The apparent subjectivity of VIA as a method can be overcome with the high-quality, competency-based training approach used with many of the Thai and Ghanaian providers. To complement and support providers after training, quality assurance methods, such as exit interviews with women or reviewing service statistics, can boost and maintain performance. An independent co-assessment conducted at least once a year, together with frequent use of the performance standards checklist as a supervisory tool, is also recommended to maintain high performance.
The programme in Thailand has screened some 250,000 eligible women using VIA as of June 2007. Some districts that have provided services for several years are reaching the level of coverage (70–75%) needed to reduce cancer mortality. These high levels of coverage are noteworthy, given that in 2003, the national annual coverage in Thailand using cytology-based screening was just 5%.Citation4
Cervical cancer screening is fully integrated into the day-to-day activities of public sector nurses in both countries; no additional human resources have been deployed for this purpose. The high number of Thai women returning for a follow-up visit is encouraging in that it shows a high level of compliance, an important aspect of scale-up of the programme. This may or may not occur in other country programmes.
The results achieved and lessons learned by Thailand and Ghana can serve as a guide for other low-resource countries. The successful transition from a demonstration project to a national programme in Thailand was dependent on a strong commitment from the Department of Health, Ministry of Public Health, Royal Thai College of Obstetricians and Gynaecologists, key trainers, supervisors and champions. It also benefited from the presence of all the necessary components – advocacy and policy development, competency-based training, availability of equipment and supplies, feasible service delivery and referral systems, appropriate information management systems, and community outreach and education. The current national policy in Thailand is to use VIA for women aged 30–45 years and regular cytological screening for women aged 45–60, with support for the referral system from the National Health Security Office.
In contrast, the lack of health infrastructure and political will in Ghana has prevented scale-up to a national programme. Specific challenges in Ghana include the low priority of cervical cancer prevention, lack of a comprehensive national programme despite existing policy, lack of awareness among communities of cervical cancer and how to prevent it, and a lack of skilled providers. In order to move forward, Ghana must develop a national cervical cancer prevention programme, implement an in-country training programme to increase the number of skilled providers, develop new sites to increase access and coverage, and improve outreach in order to increase demand in the community.
This paper documents the largest application of a single-visit approach with VIA and cryotherapy to date. It shows that such an approach is programmatically feasible and sustainable and should be considered in national investments to control cervical cancer.
Acknowledgments
We gratefully acknowledge the contributions of Sydney Adadevoh, Silvia Deganus and Amanda Adu-Amankwah, who assisted with the study in Ghana, and Dr Nanta Uamkul, Director, Bureau of Technical Advisors, Department of Health, Ministry of Public Health of Thailand, who provided support to both the study and the roll-out of the cervical cancer programme in Thailand. John McGrath provided assistance with statistical analyses, and Melissa McCormick provided editing assistance. This work was supported by a grant from the Bill & Melinda Gates Foundation through the Alliance for Cervical Cancer Prevention.
Notes
* The VIA programme offers Pap smears to some extent, because according to Thai national policy, a Pap smear should be offered if the squamo-columnar junction cannot be seen.
† Limited information (simple count of the number of women) on Pap smears has recently been incorporated into CPIS in addition to the more detailed VIA information.
References
- MD Parkin, F Bray, J Ferlay. Global cancer statistics, 2002. CA Cancer Journal for Clinicians. 55(2): 2005; 74–108.
- R Sankaranarayanan, L Gaffikin, M Jacob. A critical assessment of screening methods for cervical neoplasia. International Journal of Gynecology and Obstetrics. 89(Suppl 2): 2005; S4–S12.
- SS Shastri, K Dinshaw, G Amin. Concurrent evaluation of visual, cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai, India. Bulletin of World Health Organization. 83(3): 2005; 186–194.
- Royal Thai College of Obstetricians and Gynaecologists/JHPIEGO Corporation Cervical Cancer Prevention Group. Safety, acceptability, and feasibility of a single-visit approach to cervical cancer prevention in rural Thailand: a demonstration project. Lancet. 361(9360): 2003; 814–820.
- L Denny, L Kuhn, A Pollack. Evaluation of alternative methods of cervical cancer screening for resource-poor settings. Cancer. 89(4): 2000; 826–833.
- JL Belinson, RG Pretorius, WH Zhang. Cervical cancer screening by simple visual inspection after acetic acid. American Journal of Obstetrics and Gynecology. 98(3): 2001; 441–444.
- M Arbyn, L Gaffikin, R Sankaranarayanan. Assessment of innovative approaches to cervical cancer screening, follow-up and treatment of screen-detected cervical lesions in developing countries: a pooled analysis of ACCP trial results. 2005; PATH/IPH: Seattle.
- L Gaffikin, M Lauterback, P Blumenthal. Performance of visual inspection with acetic acid for cervical cancer screening: a qualitative summary of evidence to date. Obstetrical and Gynecological Survey. 58(8): 2003; 543–550.
- PD Blumenthal, L Gaffikin, S Deganus. Cervical cancer prevention: safety, acceptability, and feasibility of a single-visit approach in Accra, Ghana. American Journal of Obstetrics and Gynecology. 196: 2007; 407.e1–407.e9.
- SJ Goldie, L Gaffikin, JD Goldhaber-Fiebert. Cost-effectiveness of cervical cancer screening in five developing countries. New England Journal of Medicine. 353(20): 2005; 2158–2168.
- Alliance for Cervical Cancer Prevention. Planning and implementing cervical cancer prevention and control programs: a manual for managers. 2004; ACCP: Seattle.
- World Health Organization. Cervical cancer screening in developing countries: report of a WHO consultation. 2002; WHO: Geneva.
- R Sankaranarayanan, PO Esmy, R Rajkumar. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster-randomised trial. Lancet. 370(9585): 2007; 398–406.
- Alliance for Cervical Cancer Prevention. Conclusions from ACCP clinical research in developing countries. Cervical Cancer Prevention Fact Sheet. At: <www.path.org/files/RH_conclusions.pdf. >. Accessed 8 February 2008.
- WHO, Institut Catala d’Oncologia. Human papillomavirus and cervical cancer summary report: Ghana 2007. At: <http://www.who.int/hpvcentre/statistics/dynamic/ico/country_pdf/GHA.pdf. >. Accessed 3 August 2008.
- World Health Organization, Institut Catala d’Oncologia. Human papillomavirus and cervical cancer summary report: Thailand 2007. At: </www.who.int/hpvcentre/statistics/dynamic/ico/country_pdf/THA.pdf. >. Accessed 3 August 2008.
- JR Landis, GG Koch. The measurement of observer agreement for categorical data. Biometrics. 33: 1977; 159–174.