Abstract
Cervical cancer is a major cause of suffering and premature death among women in the developing world, yet it is largely prevented in most higher-income countries. From an equity perspective, cervical cancer is unequally distributed globally in ways that are unnecessary, avoidable and unjust. Although cost-effectiveness analyses demonstrate that prevention measures are justified in low-resource countries, affordability and lack of prioritisation have contributed to a lack of progress. This paper describes the inequities in cervical cancer disease burden, barriers in access to and utilisation of services, and the underlying conditions of poverty and low socio-economic status that put women in a disadvantaged position. These social disadvantages are aggravated by the disease itself, with serious consequences for women, their families and communities. Remedies are available in the form of new prevention and treatment approaches, including vaccines against human papillomavirus (HPV), rapid HPV testing, visual inspection of the cervix with acetic acid (VIA) and cryotherapy. These technologies could help to overcome the social, economic, and political disadvantages that contribute to disparities in cervical cancer incidence and mortality through an optimal combination of vaccination, screening and treatment. In the long run, however, increasing women’s access to care will also require societies to address structural barriers related to health systems and poverty.
Résumé
Le cancer du col de l’utérus est une cause majeure de souffrance et de décès prématuré dans le monde en développement. Pourtant, il est surtout prévenu dans les pays riches. Cette forme de cancer est répartie inégalement dans le monde pour des motifs évitables et injustes. Même si les analyses de rentabilité montrent que les mesures de prévention sont justifiées dans les pays à faible revenu, les coûts et une priorité insuffisante ont contribué à un manque de progrès. Cet article décrit les inégalités de la charge de morbidité du cancer du col de l’utérus, les obstacles à l’accès et à l’utilisation des services, ainsi que la pauvreté et le médiocre statut socio-économique qui placent les femmes dans une position défavorisée. Ces handicaps sociaux sont aggravés par la maladie elle-même, qui a de graves conséquences pour les femmes, leur famille et leur communauté. Les solutions sont disponibles avec de nouvelles méthodes de prévention et de traitement, notamment les vaccins contre le papillomavirus humain (PVH), les tests rapides du PVH, l’inspection visuelle après application d’acide acétique (VIA) et la cryothérapie. Ces techniques pourraient surmonter les handicaps sociaux, économiques et politiques qui contribuent aux disparités dans l’incidence de la maladie et sa mortalité par une association optimale de vaccination, dépistage et traitement. Néanmoins, à long terme, élargir l’accès des femmes aux soins exigera aussi des sociétés qu’elles lèvent les obstacles structurels liés aux systèmes de santé et à la pauvreté.
Resumen
El cáncer cervical es una causa principal de sufrimiento y muerte prematura entre las mujeres de los países en desarrollo; sin embargo, en países con ingresos más elevados, se evita en gran medida. Desde un punto de vista de equidad, el cáncer cervical es distribuido de manera desigual mundialmente, en formas que son innecesarias, evitables e injustas. Aunque los análisis de costo-eficacia demuestran que las medidas de prevención se justifican en países con escasos recursos, se han logrado pocos avances debido a la falta de asequibilidad y priorización. En este artículo se describen las injusticias en el impacto de la enfermedad del cáncer cervical, las barreras en el acceso a los servicios y la utilización de estos, y las condiciones subyacentes de pobreza y baja condición socioeconómica, que no favorecen a las mujeres. Estas desventajas sociales son agravadas por la enfermedad en sí, con graves consecuencias para las mujeres, sus familias y sus comunidades. Existen remedios en la forma de nuevas modalidades de prevención y tratamiento, como vacunas contra el virus del papiloma humano (VPH), pruebas rápidas de VPH, inspección visual del cérvix con ácido acético (IVAA) y crioterapia. Estas tecnologías podrían ayudar a superar las desventajas sociales, económicas y políticas que contribuyen a las disparidades en la incidencia del cáncer cervical y la mortalidad a causa de éste, mediante una combinación óptima de vacunación, tamizaje y tratamiento. No obstante, a la larga no sólo será necesario ampliar el acceso de las mujeres a la atención médica sino también vencer las barreras estructurales relacionadas con los sistemas de salud y la pobreza.
The past decade has seen a significant emphasis placed on the efficiency of health interventions, as measured by DALYs (disability-adjusted life years), cost-effectiveness analyses and affordability.Citation1Citation2 Complementing these has been growing attention to equity in measurement of health systems performance and priority-setting in allocation of health care resources.Citation1,3,4 While it is essential to include these issues in health policy-making, other factors should also be considered.Citation5
The meaning of equity in relation to health has evolved since Whitehead offered her classic definition of inequity as differences in health that are unnecessary, avoidable, unfair and unjust.Citation6 Although disparities are objective and evident in data, equity also involves values and individual judgement. To these principles has been added the idea that differences must be systematic rather than occasional or sporadic, and that they should result from and contribute to social disadvantage.Citation7 These differences may be evidenced in health status or health care availability or utilisation. Not all inequalities are matters of equity, since some are due to biology or geography. While every untimely death, illness and suffering is of concern, a widely accepted principle of social justice says those who are most vulnerable to illness or less able to access services, because of social or demographic characteristics over which they have little control, are entitled to special consideration.Citation6 Poverty is the most commonly identified source of inequity, but other aspects include gender, ethnicity, religion, geography, age, education and social status,Citation8Citation9 especially when these cluster and magnify negative effects.Citation6
These concepts of inequity, both in health status and access to health services, resonate strongly with regard to cervical cancer. This paper presents examples of disparities in who gets cervical cancer and the impact it has on those who are affected by it. In view of the unfair distribution of cervical cancer, it also points to promising new approaches that could help to overcome the social and political disadvantages that contribute to the disparities in cervical cancer burden. All women should be able to benefit from the preventative measures that have brought rates of cervical cancer down to the historic low levels now seen in Europe and North America.
Unequal disease burden, service availability, utilisation of care and impact
Incidence and mortality
The global burden of cervical cancer is significant, at nearly 500,000 new cases each year and about 274,000 deaths, and its unequal distribution is striking.Citation10 While relatively low incidence rates prevail in Europe, North America and Japan (generally about 10/100,000 women), rates in sub-Saharan Africa are many times higher, as are those for poorer countries in Latin America and the Caribbean, Melanesia, South and Southeast Asia. Countries in East and Southern Africa have some of the highest reported age-standardised rates per 100,000 women: Tanzania (68.6), Lesotho (61.6), Zambia (53.7) and Guinea (50.9).Citation11 In the Americas, Haiti has the highest estimated rate (87.3), but other countries in the region, such as Bolivia and Belize, also experience incidence rates above 50/100,000.Citation11 Simple geography does not explain the disparity in rates between North America and the rest of the Americas or Africa. In fact, the United States and Europe both experienced much higher rates of cervical cancer well into the 20th century until screening and treatment programmes were established. In the United States, for example, rates have fallen by 75% or more since the 1960s when screening was instituted.Citation12
The difference in mortality due to cervical cancer parallels to some extent the difference in incidence rates, but the ratio of mortality to incidence further differentiates rich from poor countries. While the global average ratio of deaths to new cases is 55%, the ratios range from just 20% in Switzerland to more than 80% in most African countries, with countries in Latin America and South Asia having ratios of 40–55%.Citation11 The greater availability of services for early detection and cancer treatment in Latin America and India enable those areas to ameliorate the toll of cervical cancer, more like the wealthy countries, in a way that is not available to women in Africa. The advanced clinical stage at which most cervical cancers are identified and the inadequacy of treatment in many developing countries accounts for their much higher mortality rates.Citation13
In additional to national and regional differences, there are disparities in disease rates within countries according to urban and rural residence and by class, race and ethnicity. In Mexico, for example, rural women had a three-fold higher risk of cervical cancer mortality than urban women.Citation14 In Australia, Aboriginal women living in metropolitan areas were more than four times as likely as non-Aboriginal women to die from cervical cancer, while Aboriginal women living in remote areas were more than 18 times as likely to die.Citation15
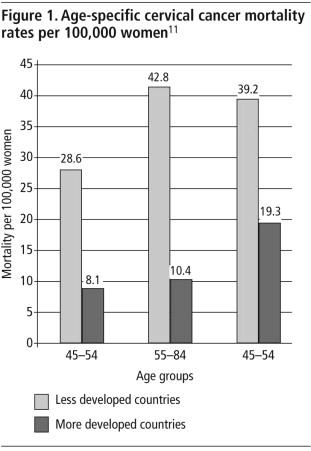
A further disparity in the epidemiology of the disease is in age distribution, whereby women in developing countries are more likely to die from cervical cancer at younger ages than women in wealthier countries (). The higher levels of access to and utilisation of screening services and of cancer treatment among younger women in wealthy countries probably explain most of the age differences. (Elderly women in both high and low-resource settings may be less likely to avail themselves of services.) However, the earlier onset of sexual activity and higher rates of early childbearing in low-resource countries may also contribute to differentials in age distribution. Overall, all these differences are largely due to socio-economic and health service issues related to underlying conditions of poverty and social status.
Service availability
The differences in avertable disease incidence and mortality are due primarily to differential access to services for screening and treatment once cancer is discovered. Unlike the developed world, where Pap smear screening has become a routine part of women’s health care, most women in developing countries have little or no access to screening or prevention services.Citation16 In the developed world, more than 75% of women have participated in some type of screening programme in the past five years, while less than 5% of women in the developing world have been screened. The challenges of implementing cervical cancer screening programmes include financial resource constraints, competing health needs, limited human resources, and poor infrastructure and logistical capacity of health systems.Citation17 The disparities are consistent with gross disparities in health service expenditure globally more broadly,Citation18Citation19 exacerbated by the concentration of high quality medical resources in urban areas, so that service availability, especially for older women in rural areas, is often limited. China is an example of this.Citation20
Moreover, health care systems in low-income countries tend to favour curative services for adults over preventative care, in response to perceived demand.Citation21 Health sector reforms that have instituted cost-recovery have also favoured curative care except for services such as immunisation and family planning, which are free. Preventative services that do exist tend to be focused on pregnant and breastfeeding women and children under five, especially with the influx of donor funding in the late 1990s.Citation22 For example, measles immunisation coverage rates in least-developed countries increased from 56% to 74% between 1990 and 2006, in notable contrast to the stagnant nature of cervical cancer services.Citation23 Despite calls for greater attention to chronic diseases in the developing world in recent years, most policymakers and donors have yet to address cervical cancer.Citation24 Services for older women are considered a lesser priority.Citation25 But even where services do exist, women may not be able to access them due to economic and social barriers.
More recently, a debate has emerged suggesting that the prioritisation of specific diseases, such as HIV and AIDS treatment and prevention in developing countries, is displacing funding for other health issues and, in some cases, further increasing disparities in services by age, gender and socio-economic status.Citation26 The same effect may be occurring with the Millennium Development Goals, which seem to be associated with a marginalisation of reproductive and sexual health care funding.Citation27
Utilisation of services
Poverty at community and household level is the dominant factor affecting who within communities and households is most likely to receive care. Although some progress has been made to reduce the number of people living on one dollar a day, in regions such as sub-Saharan Africa extreme poverty has worsened.Citation28 In Asia, where levels of extreme poverty have declined, countries still experience pockets of poverty, as well as growing income disparities between the wealthy and the poor.
User fees and the lack of reasonable health care insurance have led to unequal access to health services, as many households cannot afford even the most basic medical care, let alone the costs associated with catastrophic illnesses such as cervical cancer.Citation29 Poor households spend less on health care and are more likely to forego treatment or self-treat rather than seek care in a modern public or private facility.Citation30 Both out-of-pocket payments for health care and indirect costs of lost hours of productive work associated with illness impose a greater burden on the poor than on wealthier households.Citation31
In remote rural settings people have to travel long distances for services, consuming scarce personal resources of time and money. In addition to the opportunity costs of missed hours and days of work both within and outside the home, alternative sources of childcare may be needed. With Pap smear screening, women must return for their results. If additional diagnosis or treatment is required, women must travel further and stay in urban referral facilities. Even when treatment is provided free of charge or covered by health insurance, the non-medical costs of cancer can represent up to 50% of total family income.Citation32Citation33 These considerations are likely to influence household decisions about whether to seek screening or further care. Among women with cancer in a Nigerian study, more than 68% reported that disease-related expenditures had made a major impact on family living conditions.Citation34 Despite new approaches to screening at local health posts, which remove some of these logistical constraints, access to treatment services still requires sufficient resources to attend higher level facilities.
Gender adds another dimension to women’s unequal access in relation to need. Women represent a greater number of the unemployed and account for 60% of the world’s working poor (earning less than one dollar a day).Citation35 Within the household, where gender and poverty intersect, social values may favour males over females seeking health care. In India, gender bias in care-seeking and treatment completion for long-term illness was evident in poorer families.Citation36
Women also face information gaps and stigma associated with preventative care for cervical cancer. In some communities, women may not know about cervical cancer or its impact in their community, and few are aware that cervical cancer and its precursors are detectable through simple screening procedures. In many cultures, the notion of preventing an illness years in the future may not be valued within the household.Citation37 Potential socio-cultural barriers to seeking care include embarrassment about the pelvic examination, fear of the procedure or of being associated with sexually transmitted infections, or fear of learning they have cancer. Women may also mistrust health care providers, either because they have been treated badly by them in the past or because they have heard of poor treatment from others.Citation38
Impact of cervical cancer on family, community and society
Women have a significant influence on family welfare throughout their lives, playing central roles as managers of food security, wage earners, caretakers of children and grandchildren, carers for those who are ill,Citation39 community leaders in social and political life, and family advisors. In settings where HIV and AIDS are affecting a significant proportion of younger people, older women are taking on an even greater role in maintaining community structure and caring for affected adults and orphaned children.Citation40Citation41 The loss of women’s labour has an impact beyond individual families in developing countries, where almost 75% of food production each year is directly dependent on women’s work.Citation42
Women’s families are penalised economically by their illness and premature death, both in terms of the loss of income and the out-of-pocket medical expenses. In both urban and rural areas in sub-Saharan Africa, women are the main income earners in approximately one-third of households.Citation43 In rural areas in developing countries, the number of female-headed households is increasing as men migrate for employment.Citation44 Women are often responsible for non-income-generating work that is also critical to family well-being, such as gathering water and firewood, preparing food and tending to livestock.Citation45
In these settings, the effect of a disease like cervical cancer on children and other dependants can be devastating. In the Nigerian study mentioned earlier, 70% of women with breast or cervical cancer reported that the family had experienced a major loss of revenue due to the illness; 62% of patients reported not being able to attend work; and 33% reported that their illness disrupted a relative’s work.Citation34
Evidence from a study in Tanzania suggests that in households where an adult woman had died within the past 12 months, children spent half as much time in school as did children from households where such a death had not occurred or where an adult male had died.Citation42 When a grandmother falls ill or dies 10–20 years prematurely, her family suffers the loss of this critical nurturing or must pay to replace this care, with the consequent reduction in available household resources.
Making screening and pre-cancer treatment accessible
A central element that characterises inequity is that the conditions involved are avoidable. Is it feasible to provide effective screening and pre-cancer treatment within the resource-constrained settings of low-income countries? In the past decade, the Alliance for Cervical Cancer Prevention has demonstrated that there are feasible options for providing basic preventative services.
Cost-effective screening methods like visual inspection with acetic acid (VIA), followed by treatment with cryotherapy or freezing of pre-cancerous cervical tissue, can substantially reduce the incidence of cervical cancer and identify invasive cancer at an earlier, more treatable stage.Citation46Citation47 In a study of nearly 80,000 women in India aged 30–59 screened with VIA, there was a 25% reduction in cervical cancer incidence and 35% reduction in cancer deaths, as compared to a control group that was not screened. Benefits were most marked for women in their 30s.Citation48 The advantages of VIA are that it is less expensive than traditional cytology, can be offered by lower-level health workers at primary care facilities that are more accessible and acceptable to women (especially rural women), and provides immediate results that make it more likely that women with a positive screening test will get timely treatment. At least seven countries in Africa (Angola, Ghana, Kenya, Mali, Mozambique, South Africa, Tanzania), three countries in Asia (Bangladesh, India, Thailand), and three in Latin America (Bolivia, Guatemala, Peru) have allocated government funding to support or scale up VIA screening programmes, while numerous others have incorporated VIA into national cancer guidelines or used donor funds to launch or continue new screening programmes using VIA and cryotherapy.
A rapid, inexpensive human papillomavirus (HPV) test soon to be available commercially also offers women the possibility of taking a cervical specimen themselves to send for laboratory processing, which may overcome some of the cultural barriers associated with screening.Citation49 Decision modelling has demonstrated that a screening programme that is targeted at women in their 30s, even if screening can only be provided once or twice in a lifetime, can be cost-effective and affordable for health systems.Citation50
Because socio-cultural and economic barriers can prevent women from taking up the opportunity to be screened, attention to their fears and perceptions should be incorporated into outreach and educational programmes to inform communities. It is also possible to overcome the effects of negative local images of cervical cancer as a death sentence, or of a positive screening test as a sign of marital infidelity, by careful messaging in educational materials and interactions.Citation37 As with other clinical services, ensuring that women are treated with respect and that services are perceived to be of good quality is an important determinant of women’s willingness to take up screening and encourage others to do so.Citation51
Offering HPV vaccine to young adolescent girls
The availability of two new HPV vaccines provides a complementary strategy that could prevent as much as 70% of all cervical cancers (with nearly universal coverage of eligible recipients and long-term duration of protection) and overcome many of the barriers that contribute to the current unfair distribution of disease. The vaccines, which require three doses over a six-month period, are highly effective in preventing persistent infection with HPV types 16 and 18 and the subsequent pre-cancerous lesions and 70% of cervical cancer worldwide associated with them.Citation52Citation53 Since the vaccines are not effective against HPV once a person has been infected with it, and acquisition of HPV infection can occur relatively quickly after sexual debut,Citation54Citation55 it is widely accepted that providing young adolescent girls with the vaccine before the onset of sexual activity is the most cost-effective strategy.Citation56Citation57 Unlike screening, though, which has a proven track record of reducing cervical cancer rates when high quality services are made widely available, questions about the overall effectiveness of HPV vaccination programmes need time to be resolved.
Can the vaccine overcome some of the barriers to preventative services faced by adult women? Immunisation is widely accepted by communities as a valuable preventative service, and is recognised as an efficient way to reduce inequities in health.Citation58Citation59 Delivering HPV vaccine will, in all likelihood, require different approaches than infant vaccines, and several promising options have been identified. School-based immunisation of girls in later primary grades offers the possibility of reaching a high proportion of eligible girls. In recent years, the number of girls attending primary school in developing countries has risen, from 78% in 1990 to 85% in 2005, wiping out the gender gap with boys in East Asia, Latin America, and Eastern and Southern Africa. The gender gap in education has also narrowed in both urban and rural settings and within each economic quintile.Citation23 Community outreach activities that deliver multiple health interventions are a possible strategy for reaching girls who are out of school as well.
Although there have been suggestions that communities may have concerns about the vaccine, because of its link to a sexually transmitted infection and its targeting of girls, preliminary data from studies in Peru, Uganda and Viet Nam suggest that the main barriers to acceptance are largely related to lack of awareness of the burden of cervical cancer and fears about potential fertility effects or overall safety of the vaccine. These same studies showed a positive overall view of HPV immunisation and support for schools as a reasonable venue for HPV vaccine delivery.Citation60 Preliminary data from a Peru study also showed that once girls agree to vaccination in school, completion of the three-dose regimen is above 90%.Citation61
Government-supported delivery of HPV vaccination in schools or the community, with appropriate education and financing, has great potential to overcome the disadvantages faced by screening programmes for adult women. There is less need to tap special family resources, or replace adult women’s labour for service seeking, and less stigma in being vaccinated than in having a vaginal exam. Although the initial high cost of the vaccine presents a formidable barrier, international financing sources like the GAVI Alliance subsidise other vaccines. In June 2008, GAVI signalled that it would likely support HPV vaccines for the 72 poorest countries, which means countries would pay only a $0.15 or $0.20 per dose co-financing charge. In addition, there is no reason to think that HPV vaccines will not follow the pattern of other new vaccines with declines in price over time as the volume of sales climbs and other manufacturers come into the market.Citation62
It will take time to resolve the remaining uncertainties about long-term vaccine protection, possible cross-protection against non-vaccine HPV types, and the feasibility and cost of delivering the vaccine to appropriate groups. But vaccination, along with an appropriate screening programme for adult women, raise real possibilities of overcoming the long-standing barriers that have led to the current disparities in disease impact.
Conclusion: building awareness and political will
Recognition of the toll of cervical cancer and of new opportunities for prevention is growing, along with commitment to tackle this critical aspect of women’s health, but there is still much work to be done. The Alliance for Cervical Cancer Prevention partners continue to spread the word about simple, effective and affordable methods for screening and pre-cancer treatment. Cervical Cancer Action, a new coalition of interested groups and individuals that launched a Call to Action in 2007, continues to build support at the global and national levels (<www.cervicalcanceraction.org>). At a PAHO meeting in Mexico in May 2008, 21 countries signed a declaration resolving to strengthen cervical cancer prevention and control (<www.paho.org/English/DD/PIN/pr080514.htm>). Champions at the national level, including parliamentarians and professional societies, are drawing attention to the unfair burden older women are carrying and the broad benefits that could be achieved by implementing HPV vaccination for young adolescent girls and appropriate screening and treatment programmes for women in their 30s and 40s. In India, Peru, and Uganda, national coalitions have been established to bring together stakeholders who want to address cervical cancer. Where decentralisation has shifted decision-making down to the local level, district officials and community groups will need to support the necessary investments in cervical cancer prevention services wherever the burden of disease warrants it. There are important new opportunities to break the cycle of preventable cervical cancer through an optimal combination of vaccination, screening and treatment. In the long run, however, increasing women’s access to care will also require societies to address structural barriers related to health systems and poverty.
References
- MA Gonzalez Block, P Sandiford, JA Ruiz. Beyond health gain: the range of health system benefits expressed by social groups in Mexico and Central America. Social Science and Medicine. 52(10): 2001; 1537–1550.
- DR Gwatkin. Health inequalities and the health of the poor: what do we know? What can we do?. Bulletin of World Health Organization. 78(1): 2000; 3–18.
- ME Kruk, LP Freedman. Assessing health system performance in developing countries: a review of the literature. Health Policy. 85(3): 2008; 263–276.
- M Whitehead, G Dahlgren, D McIntyre. Putting equity center stage: challenging evidence-free reforms. International Journal of Health Services. 37(2): 2007; 353–361.
- AM Dans, L Dans, AD Oxman. Assessing equity in clinical practice guidelines. Journal of Clinical Epidemiology. 60(6): 2007; 540–546.
- M Whitehead. The Concepts and Principles of Equity and Health. EUR/ICP/RPD 414. 1990; World Health Organization Regional Office for Europe: Copenhagen.
- P Braveman. Health disparities and health equity: concepts and measurement. Annual Review of Public Health. 27(1): 2006; 167–194.
- DR Gwatkin. 10 best resources on … health equity. Health Policy and Planning. 22(5): 2007; 348–351.
- P Braveman, S Gruskin. Defining equity in health. Journal of Epidemiology and Community Health. 57(4): 2003; 254–258.
- DM Parkin, F Bray. Chapter 2: The burden of HPV-related cancers. Vaccine. 21(24 Suppl 3): 2006; S11–S25.
- Ferlay J, Bray F, Pisani P, et al. Globocan 2002: Cancer Incidence, Mortality and Prevalence Worldwide. [Version 2.0]. 2004. Lyon: IARC Press. IARC CancerBase No. 5.
- HC Kitchener, PE Castle, JT Cox. Chapter 7: Achievements and limitations of cervical cytology screening. Vaccine. 21(24 Suppl 3): 2006; S63–S70.
- R Sankaranarayanan, J Ferlay. Worldwide burden of gynaecological cancer: the size of the problem. Best Practice and Research. Clinical Obstetrics & Gynaecology. 20(2): 2006; 207–225.
- LS Palacio-Mejia, G Rangel-Gomez, M Hernandez-Avila. Cervical cancer, a disease of poverty: mortality differences between urban and rural areas in Mexico. Salud Pública de México. 45(Suppl 3): 2003; S315–S325.
- ED O’Brien, RS Bailie, PL Jelfs. Cervical cancer mortality in Australia: contrasting risk by aboriginality, age and rurality. International Journal of Epidemiology. 29(5): 2000; 813–816.
- J Bradley, M Barone, C Mahe. Delivering cervical cancer prevention services in low-resource settings. International Journal of Gynecology and Obstetrics. 89(Suppl 2): 2005; S21–S29.
- L Denny, M Quinn, R Sankaranarayanan. Chapter 8: Screening for cervical cancer in developing countries. Vaccine. 24(Suppl 3): 2006; S71–S77.
- DR Gwatkin, A Bhuiya, CG Victora. Making health systems more equitable. Lancet. 364(9441): 2004; 1273–1280.
- P Braveman, E Tarimo. Social inequalities in health within countries: not only an issue for affluent nations. Social Science and Medicine. 54(11): 2002; 1621–1635.
- L Bogg, D Hengjin, K Wang. The cost of coverage: rural health insurance in China. Health Policy and Planning. 11(3): 1996; 238–252.
- JM Msuya, CN Nyaruhucha, J Kaswahili. Does preventive health care have a chance in the changing health sector in Tanzania?. East African Medical Journal. 80(3): 2003; 135–139.
- E Delamonica, A Minujin, J Gulaid. Monitoring equity in immunization coverage. Bulletin of World Health Organization. 83(5): 2005; 384–391.
- UNICEF. Progress for Children: A World Fit for Children. Statistical Review. No.6. 2007; UNICEF: New York.
- R Horton. Chronic diseases: the case for urgent global action. Lancet. 370(9603): 2007; 1881–1882.
- C Elias, J Sherris. Reproductive and sexual health of older women in developing countries. BMJ (Clinical Research ed.). 327(7406): 2003; 64–65.
- J Shiffman. Has donor prioritization of HIV/AIDS displaced aid for other health issues?. Health Policy and Planning. 23(2): 2008; 95–100.
- SW Sinding. Keeping sexual and reproductive health at the forefront of global efforts to reduce poverty. Studies in Family Planning. 36(2): 2005; 140–143.
- A Ahmed, R Vargas Hill, L Smith. The World’s Most Deprived: Characteristics and Causes of Extreme Poverty and Hunger. Report No.2020. Discussion Paper 43. 2007; International Food Policy Research Institute: Washington DC.
- DB Huong, NK Phuong, S Bales. Rural health care in Vietnam and China: conflict between market reforms and social need. International Journal of Health Services. 37(3): 2007; 555–572.
- F Castro-Leal, J Dayton, L Demery. Public spending on health care in Africa: do the poor benefit?. Bulletin of World Health Organization. 78(1): 2000; 66–74.
- D McIntyre, M Thiede, G Dahlgren. What are the economic consequences for households of illness and of paying for health care in low-and middle-income country contexts?. Social Science and Medicine. 62(4): 2006; 858–865.
- PS Houts, A Lipton, HA Harvey. Nonmedical costs to patients and their families associated with outpatient chemotherapy. Cancer. 53(11): 1984; 2388–2392.
- M Stommel, CW Given, BA Given. The cost of cancer home care to families. Cancer. 71(5): 1993; 1867–1874.
- JU Ohaeri, OB Campbell, AO Ilesanmi. The psychosocial burden of caring for some Nigerian women with breast cancer and cervical cancer. Social Science and Medicine. 49(11): 1999; 1541–1549.
- M Chen, J Vanek, F Lund. Progress of the World’s Women 2005: Women, Work and Poverty. 2005; United Nations Development Fund for Women: New York.
- A Iyer, G Sen, A George. The dynamics of gender and class in access to health care: evidence from rural Karnataka, India. International Journal of Health Services. 37(3): 2007; 537–554.
- A Bingham, A Bishop, P Coffey. Factors affecting utilization of cervical cancer prevention services in low-resource settings. Salud Pública de México. 45(Suppl 3): 2003; S408–S416.
- I Agurto, S Arrossi, S White. Involving the community in cervical cancer prevention programs. International Journal of Gynecology and Obstetrics. 89(Suppl 2): 2005; S38–S45.
- J Knodel, S Watkins, M VanLandingham. AIDS and older persons: an international perspective. Journal of Acquired Immune Deficiency Syndrome. 33(Suppl 2): 2003; S153–S165.
- UNAIDS. 2004 Report on the Global AIDS Epidemic. 4th Global Report. 2004; UNAIDS: Geneva.
- EJ Schatz. “Taking care of my own blood”: older women’s relationships to their households in rural South Africa. Scandinavian Journal of Public Health. 69(Suppl): 2007; 147–154.
- World Bank. A New Agenda for Women’s Health and Nutrition. 1994; World Bank: Washington DC.
- CE Levin, MT Ruel, SS Morris. Working women in urban settings: traders, vendors, and food security in Accra. World Development. 27(11): 1999; 1977–1991.
- UN Food and Agriculture Organization. Women and food security. FAO Focus March 1997. At: <www.fao.org/FOCUS/E/Women/Sustin-e.htm. >. Accessed 3 March 2008.
- UN Population Fund. Food for the Future: Women, Population, and Food Security. 1996; UNFPA: New York.
- R Sankaranarayanan, L Gaffikin, M Jacob. A critical assessment of screening methods for cervical neoplasia. International Journal of Gynecology and Obstetrics. 89(Suppl 2): 2005; S4–S12.
- R Sankaranarayanan, R Rajkumar, PO Esmy. Effectiveness, safety and acceptability of ‘see and treat’ with cryotherapy by nurses in a cervical screening study in India. British Journal of Cancer. 96(5): 2007; 738–743.
- R Sankaranarayanan, PO Esmy, R Rajkumar. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster-randomised trial. Lancet. 370(9585): 2007; 398–406.
- PATH. Innovation in biochemical cervical cancer screening. November. 2007; PATH: Seattle. At: <www.path.org/files/RH_start_biochem_scr_fs_en.pdf. >. Accessed 10 March 2007.
- SJ Goldie, L Gaffikin, JD Goldhaber-Fiebert. Cost-effectiveness of cervical cancer screening in five developing countries. New England Journal of Medicine. 353(20): 2005; 2158–2168.
- J Winkler, A Bingham, P Coffey. Women’s participation in a cervical cancer screening program in northern Peru. Health Education Research. 23(1): 2008; 10–24.
- KA Ault. Effect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trials. Lancet. 369(9576): 2007; 1861–1868.
- J Paavonen, D Jenkins, FX Bosch. Efficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trial. Lancet. 369(9580): 2007; 2161–2170.
- A Hildesheim, R Herrero, S Wacholder. Effect of human papillomavirus 16/18 L1 viruslike particle vaccine among young women with preexisting infection: a randomized trial. JAMA. 298(7): 2007; 743–753.
- R Winer, Q Feng, J Hughes. Risk of female human papillomavirus acquisition associated with first male sex partner. Journal of Infectious Diseases. 197(2): 2008; 279–282.
- JA Kahn, RD Burk. Papillomavirus vaccines in perspective. Lancet. 369(9580): 2007; 2135–2137.
- FT Cutts, S Franceschi, S Goldie. Human papillomavirus and HPV vaccines: a review. Bulletin of World Health Organization. 85(9): 2007; 719–726.
- UNICEF. State of the World’s Children 2008. 2008; UNICEF: New York.
- FE Andre, R Booy, HL Bock. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bulletin of World Health Organization. 86(2): 2008; 140–146.
- LaMontagne DS, Bingham A, Katahoire A, et al. HPV vaccine implementation in developing countries: understanding the socio-cultural context, health systems environment and policy landscape for successful vaccine delivery. Presented at: 24th International Papillomavirus Conference, Beijing, 7 November 2007.
- Instituto de Investigación Nutricional. Strategies for the Introduction of the Human Papillomavirus (HPV) Vaccine for the Prevention of Cervical Cancer: Final Report to PATH. 2008; Instituto de Investigación Nutricional: Lima. (Forthcoming).
- RT Mahoney, JE Maynard. The introduction of new vaccines into developing countries. Vaccine. 17(7–8): 1999; 646–652.