Abstract
Breast cancer is a serious threat to the health of women globally, and an unrecognised priority in middle-income countries. This paper presents data from Mexico. It shows that breast cancer accounts for more deaths than cervical cancer since 2006. It is the second cause of death for women aged 30–54 and affects all socio-economic groups. Data on detection, although under-reported, show 6,000 new cases in 1990, and a projected increase to over 16,500 per year by 2020. Further, the majority of cases are self-detected and only 10% of all cases are detected in stage one. Mexico’s social security systems cover approximately 40–45% of the population, and include breast cancer treatment. As of 2007, the rest of the population has the right to breast cancer treatment through the Popular Health Insurance. Despite these entitlements, services are lacking and interventions for early detection, particularly mammography, are very limited. As of 2006 only 22% of women aged 40–69 reported having a mammogram in the past year. Barriers exist on both the demand and supply sides. Lobbying, education, awareness-building and an articulated policy response will be important to ensure expanded coverage, access to and take-up of both treatment and early detection.
Résumé
Le cancer du sein menace gravement la santé des femmes dans le monde et c’est une priorité non reconnue dans les pays à revenu intermédiaire. Des données au Mexique montrent que, depuis 2006, il provoque plus de décès que le cancer du col de l’utérus. C’est la deuxième cause de décès des femmes âgées de 30 à 54 ans et le cancer du sein touche tous les groupes socio-économiques. En 1990, malgré une sous-notification, 6000 nouveaux cas avaient été détectés et les projections prévoient plus de 16 500 par an d’ici à 2020. De plus, la majorité des cas sont détectés lors d’un auto-examen et 10% seulement des cas sont décelés au stade 1. La sécurité sociale mexicaine couvre environ 40–45% de la population et prévoit le traitement du cancer du sein. En 2007, le reste de la population pouvait bénéficier d’un traitement au titre de l’Assurance populaire. Malgré ces droits, les services font défaut et les interventions de dépistage précoce, particulièrement la mammographie, sont très limités. En 2006, 22% seulement des femmes âgées de 40 à 69 ans ont indiqué avoir subi une mammographie l’année précédente. Des obstacles existent aussi bien du côté de l’offre que de la demande. Les groupes de pression, l’éducation, la sensibilisation et une riposte politique articulée seront des facteurs importants pour élargir la couverture du traitement et du dépistage précoce, ainsi que l’accès et le recours à ces services.
Resumen
El cáncer de mama es una grave amenaza para la salud de las mujeres mundialmente y una prioridad no reconocida en países de ingresos medios. En ese artículo se exponen datos de México. Se muestra que el cáncer de mama ocasiona más muertes que el cáncer cervical desde 2006. Es la segunda causa de muerte entre las mujeres de 30 a 54 años de edad y afecta a todos los grupos socioeconómicos. Los datos sobre su detección, aunque subreportados, muestran 6,000 casos nuevos en 1990, y un aumento previsto en más de 16,500 al año al cabo de 2020. Más aún, la mayoría de los casos son autodetectados y sólo el 10% de todos los casos se detectan en la primera etapa. Los sistemas de seguridad social de México cubren aproximadamente entre el 40 y el 45% de la población e incluyen tratamiento para el cáncer de mama. Desde 2007, el resto de la población tiene derecho a recibir tratamiento del cáncer de mama mediante el Seguro de Salud Popular. Pese a estos derechos, los servicios son escasos y las intervenciones para la detección temprana, particularmente la mamografía, son muy limitadas. Desde 2006 sólo el 22% de las mujeres de 40 a 69 años informaron haber tenido una mamografía en el último año. Existen barreras tanto en demanda como en oferta. El cabildeo, la educación, la concienciación y una respuesta articulada de políticas serán importantes para garantizar mayor cobertura, acceso al tratamiento y a las intervenciones de detección temprana, y la aceptación de ambos.
The breast cancer epidemic is an established health priority in developed countries. In middle-income countries, insufficient attention has been paid to this emerging health problem. Recent evidence shows that breast cancer is now a leading cause of death and disability among women in developing countries.Citation1 At the same time, research has produced new treatment options, many of which are costly. Thus, the breast cancer epidemic represents a new challenge for health system financing and financial protection, especially for developing countries.
In Mexico, with a population of just over 100 million, breast cancer is now one of the most serious challenges to the health of adult women. This remains a little known fact and misconceptions abound. Cervical cancer continues to be perceived as a much greater threat to the health and lives of poor women. Breast cancer is widely believed to be heavily concentrated among those of higher socio-economic status. In fact, poorer women today face the double burden of high rates of both breast and cervical cancers. Breast cancer is now responsible for a greater number of deaths in Mexico than cervical cancer overall, and affects adult women of all ages and levels of income. It is now the second largest cause of death among adult Mexican women aged 30–54.Citation2
As regards policy, in 2003, the Ministry of Health extended and expanded official health regulations and legislation concerning the management of breast cancer through a technical directive (Norma Oficial Mexicana).Citation3 More stringent criteria were established to steward public and private health services in prevention, diagnosis, treatment, control and surveillance of the disease. To promote early detection, the directive stresses self-examination, clinical examination and mammography. Annual clinical examination by trained personnel is established for all women aged 26 or older who visit a health clinic. Mammography is recommended annually or bi-annually for women aged 40–49 with specific risk factors and annually for all women aged 50 and over. While this directive is important in providing a normative framework that covers the entire health sector, it does not guarantee resources or enforcement. Hence, coverage remains far from adequate.
In terms of financing and provision of treatment for cases that are detected, Mexico’s social security systems cover approximately 40–45% of the population, and breast cancer treatment is included in the range of services covered.Citation4Citation5 While waiting times are typically problematic and drugs are often not available and must be paid for out-of-pocket, social security-supported services do offer substantial care free of charge. Yet, access to this care is restricted to those who work in the formal sector of economy.Citation6Citation7 The rest of the population rely on historically under-funded public services from the Ministry of Health. Much of the population and especially the uninsured pay for services out of pocket, using the private sector.Citation8Citation9
A key policy initiative was the 2003 health reform and legislation that created the Popular Health Insurance.Citation9,10 This initiative included a substantial increase in financing and offered financial protection to all families that did not have access to social security, mostly concentrated in the poorer segments of the population. Roll-out of the Popular Health Insurance is taking place over seven years, gradually covering the entire target population, and expanding the package of diseases and services covered. In early 2007, breast cancer treatment, including a broad range of services and drugs, was introduced into the Fund for Protection against Catastrophic Expenditures of the Popular Health Insurance. As a result, any person diagnosed with breast cancer after that date, regardless of income or employment status, now has the right to receive publicly-funded health care.Citation11Citation12 This important policy initiative guarantees a social right de jure, but it is still in the first stages of implementation. In practice, not all women actually have access to these services. Significant barriers are present on both the demand and supply sides, which make lobbying, education and awareness-building especially important to ensure implementation.Citation13–15
One of the key issues in Mexico, as elsewhere, is improving and extending screening in order to promote early detection. Available data suggest that only 5–10% of cases in Mexico are detected in the earliest stages of disease (localised in the breast)Citation16 as compared to 50% in the United States,Citation17 making treatment more difficult, costly and uncertain for women, their families and the health system.
This paper summarises global statistics on breast cancer in developing countries, analyses trends in mortality in Mexico as compared to cervical cancer, and then presents available data on health care utilisation and barriers to access. The conclusions offer reflections on the steps required to promote early detection and improve access to care for breast cancer in Mexico and other parts of the Latin American and Caribbean region.
The primary sources of data on Mexico used in the paper are the National Institute for Statistics, Geography and Information/Ministry of Health database on mortality from 1979–2006,Citation18Citation19 the World Health Organization mortality database prior to 1979.Citation20 the National Population Council population projections for 1950–2050,Citation21 the Ministry of Health (General Directorate for Health Information) calculations of the burden of disease among women in Mexico and the calculation of avoidable deaths for 2000–2004,Citation22 the National Survey of Health 2000 and the National Survey of Health and Nutrition 2006.Citation6Citation7
The health burden of breast cancer in developing countries
Breast cancer is now a leading cause of death and disability in the developing world, with 45% of new cases reported in developing countries.Citation23 With some notable exceptions, breast cancer mortality is also greater in poorer countries, accounting for an estimated 55% of deaths.Citation23
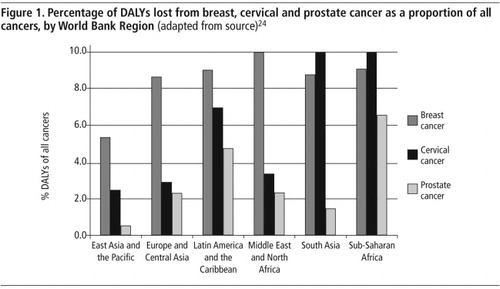
Recent analysis of mortality and morbidity trends illustrate the burden of the disease in developing countries.Citation24 As a proportion of all Disability Adjusted Life Years (DALYs) lost to cancer, breast cancer exceeds cervical and prostate cancer in all developing world regions except South Asia and sub-Saharan Africa. In the Latin American and Caribbean region, breast cancer is the leading cause of lost DALYs from cancer at 9%, followed by cervical cancer at 7%. These differences are larger in other regions. In Europe and Central Asia, as well as the Middle East and North Africa, breast cancer accounts for three to four times more DALYs lost to cancer than cervical or prostate cancers, and twice as many in East Asia and the Pacific. ().
Mortality trends in Mexico
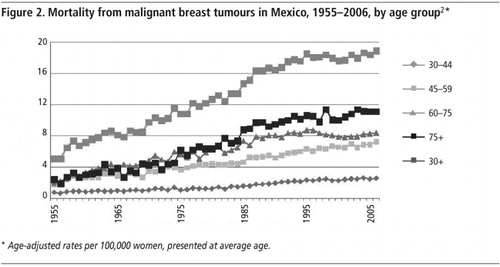
Breast cancer mortality rates in Mexico show an important increase over the past five decades.Footnote* Between 1955 and 1960, when the first reliable data were available, the rate was about two to four deaths per 100,000 women. It then rose steadily in adult women of all ages () to about nine per 100,000 by the mid-1990s, and has remained more or less stable since then.
Breast cancer is producing a heavy burden of premature death, as 60% of the women who die are aged 30–59. There is also some evidence that the average age at onset is lower in developing than in developed countries.Citation25Citation26
By 2006, breast cancer had become the second most common cause of death among women aged 30–54, and the third most common among women aged 30–59 (after diabetes and cardiovascular disease). Although breast cancer is still more common in population groups of higher socio-economic status, it is now affecting all population groups.Citation2,25,26 In the Mexican Institute of Social Security, which includes employees and families from the private sector and hence a higher average income bracket, breast cancer is the second most common cause of death among women aged 30–59. In the rest of the population, with a lower average income, breast cancer is the sixth most common cause.
The distribution of mortality by state also suggests that breast cancer is increasingly affecting both rich and poor, although it is still more concentrated in the wealthier parts of the country. It is the second most common cause of death among women aged 30–59 in 11 of Mexico’s 32 states, most of which are wealthier and where health services are most available. Still, this is also the case in a few of the poorest states, such as Veracruz.Citation2 This list includes Mexico City, which accounts for approximately 20% of the Mexican population.
Reliable national level data on prevalence and incidence are not available due to the lack of a cancer registry. Published estimates suggest that there were some 6,000 new cases of breast cancer in Mexico in 1990, and this is projected to rise to more than 16,500 per year by 2020.Citation25 Lack of access to early detection also suggests that there is a large backlog of undetected cases.
Divergence in mortality: breast cancer vs. cervical cancer
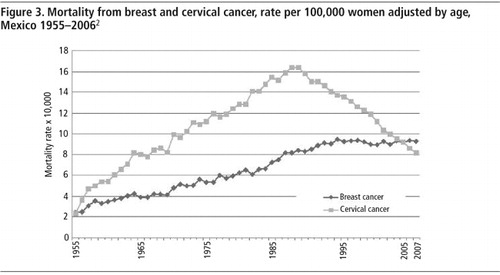
Age-adjusted (for world population) mortality rates, presented in , show that mortality from cervical cancer among Mexican women exceeded mortality from breast cancer from 1955 to 2005. As of 2006, the risk of dying from breast cancer exceeded that of cervical cancer. By contrast, in 1980 the risk of dying from cervical cancer was double that of breast cancer in all age groups. While deaths attributable to both cervical and breast cancer rose steadily from the mid-1950s through 1990, death rates from cervical cancer increased much more than from breast cancer, reaching a high of more than 16 deaths per 100,000 women. As of 1990, however, death rates from cervical cancer began a rapid decline that continued through 2006, reaching a low of just over eight deaths per 100,000. Over the same period, rates of death attributable to breast cancer rose and then leveled off. In 2005, the rate of deaths from cervical and breast cancer were about equal. By 2006, they had crossed, with breast cancer exceeding cervical cancer for the first time. There is substantial evidence at the global level to support these trends.Citation27Citation28
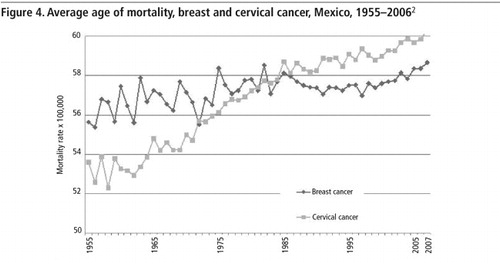
Further, the age at death from breast cancer has remained quite stable, while that of cervical cancer has risen substantially ().Citation2 Prior to 1985, the average age at death from cervical cancer was below that of breast cancer, while the opposite is now the case. The average age of Mexican women who died from breast cancer in 2005 was almost two years younger than those who died from cervical cancer.
Further, while cervical cancer is still more common among the poorer segments of the population, breast cancer is quickly gaining ground among them.Citation2 This is evident comparing data across states over time. In particularly poor states, such as Chiapas, Oaxaca, Puebla and Guerrero, the risk of dying from cervical cancer continues to be higher than from breast cancer, although the gap is closing. By contrast, in states such as Nuevo León, Jalisco, Baja California, and in Mexico City, the opposite has been the case for several years. In Mexico City and Nuevo Leon, for example, the rates crossed in the late 1980s while in Jalisco this occurred in 2001.Citation2
Health care utilisation in Mexico
Data on health care access and utilisation for breast cancer in Mexico are scarce, as is true for the rest of Latin America as well. Available evidence points to a lack of access to health services, and particularly to coverage in screening mammography. A study of 256 Mexican women diagnosed with breast cancer showed that in 90% of cases it was identified by the woman herself, and only 10% were diagnosed in stage one.Citation29 The same study also showed that only 30% of women undertook self-examination and even fewer did it properly.Citation29 At the same time, education for women on breast health continues to be lacking, although evidence suggests that with training women are much more likely to detect a lesion.Citation14
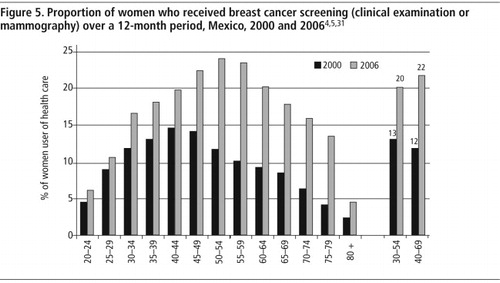
Although rates continue to be very low, there is some evidence that use of screening has increased. The most recent National Health SurveysCitation6Citation7 include a question on whether the woman had gone to a health clinic for any type of breast cancer screening in the year prior to the survey.Footnote* These data show that only 12% of women aged 40–69 had had a clinical examination (including a mammogram) in 2000, while in 2006, 22% of women had had a mammogram. The increase occurred in all age groups, but was greater for ages 45 and over. This can be viewed as a positive shift due to the greater efficacy of mammography among older women with reduced breast tissue density ().Citation30 Further, these increases are present in the majority, though not all, the states, indicating that use of services is spreading throughout the country. There is also some evidence of an increase in the proportion of women who reported receiving the results of their mammogram, from 78% to 87%. Unfortunately, there is no information available on follow-up screening.
Information on access to treatment is also lacking. Data from the Mexican Social Security Institute show a rising trend in hospital discharge rates associated with breast cancer, with an increase of 80% in the period 1986–2003. This rate of increase is substantially above that for other illnesses, such as heart disease or diabetes. In the same period, hospital discharge rates associated with cervical cancer declined by approximately 25–30%.Citation31
Conclusions and recommendations
Breast cancer is a serious threat to the health of women, the well-being of families, the health system and society in many developing countries. This is particularly evident in middle-income countries where the epidemiological and demographic transitions have advanced substantially. In Mexico, 50 years of evidence from mortality trends support this conclusion.
Some of what was true (or believed to be true) about the nature of breast cancer in Mexico is no longer the case. First, it is no longer clear that cervical cancer affects substantially more women or causes more deaths. In Mexico, as of 2006, mortality from breast cancer exceeded that from cervical cancer. There are competing hypotheses to explain the rise of breast cancer – later and fewer pregnancies, less breastfeeding, hormone replacement therapy, environmental risk factors, nutrition, epidemiological transition, among others.Citation25–27,29,32,33 At the same time, there are also several possible and overlapping explanations for the decline in cervical cancer rates, including increased screening and treatment programmes, the decline in birth rates, and increases in coverage of health education.Citation28,34,35 While more research might better explain the causal factors behind each of these trends, the basic facts are clear: breast cancer rates have risen while cervical cancer rates have fallen, and it is breast rather cervical cancer that today accounts for more deaths overall among Mexican women.
Second, breast cancer affects both younger and older women. A large proportion of deaths from breast cancer in developing countries – in many countries about 50% – occur in women below the age of 54.Citation23Citation27 Breast cancer treatment should become a part of wider sexual and reproductive health services for women.
Third, breast cancer was often thought of as the cancer of the rich and cervical cancer the cancer of the poor. Today, breast cancer affects both rich and poor women, although cervical cancer remains much more common among the poor. Thus, poor women face a double burden – a high risk of contracting and dying from both types of cancer – primarily due to lack of prevention (in the case of cervical cancer), and early detection and adequate treatment options for both cancers.
There are significant barriers on both the demand and supply sides for detecting and treating breast cancer.Citation13Citation14 Comprehensive data on availability of, and access to, these services are not readily available for Mexico, but a national, qualitative study is being undertaken through the National Institute of Public Health to identify these barriers.Citation36
Breast self-examination is stressed by non-governmental organisations and the Ministry of Health services network, in part due to lack of access to mammography.Citation16,37–39 Moreover, in general, clinical examination often does not include a breast examination. When it does, it is often not a technically sound procedure.Citation14 Access to mammography is also lacking and this is due to a shortage of units and trained personnel, especially in rural areas.Citation14,15,26,29,39 One qualitative study highlighted the difficulties in access to treatment due to cost, paperwork, lack of information, distance and lack of child care.Citation40
There are also barriers related to misconceptions and lack of knowledge on the part of women. Many women have little information about the importance of early detection, treatment and risk factors for breast cancer. Initial interviews carried out in Mexico City with practitioners show that particularly low-income women are uncomfortable with or afraid of mammography and are discouraged from having it by their partners.Citation36
Priorities for research and policy
In the face of these barriers, what are the most important strategies? Many countries in the Latin American and Caribbean region, including Mexico, have national health plans that include breast cancer as a priority. These initiatives could be greatly enhanced by applying the approach of the Breast Health Global Initiative, which is to develop evidence-based norms appropriate to the economic and cultural reality of each country, to improve clinical outcomes. The strategy promotes an integrated and systematic approach to health education, clinical examination, mammography and treatment.Citation41
A priority is to collect more and better data and keep detailed clinical records. In this paper, we were able to analyse a long-time series on mortality for Mexico, but satisfactory data on prevalence, perceptions, health care provision and utilisation are not available. As is the case for most of the region, cancer registries are either poor or do not exist in Mexico.
A research priority is to generate evidence on causal factors in Mexican women, in order to better target programmes and policies. Research should also focus on understanding the reasons for the increase in breast cancer mortality as well as the decline in cervical cancer.Citation42Citation43
More emphasis must be placed on early detection. One of the key strategies is to increase awareness and education about breast health among women, but this must be complemented by a response on the supply side. It is not realistic to assume that, in the short or even medium-run, developing countries can move to providing screening mammography to all the women who should have it. There is substantial evidence that breast self-examination, and even breast clinical examination, are not effective in reducing mortality in populations where most cases are detected in the earliest stages of the disease,Citation44–47 There is little evidence in this regard from developing countries, where detection in later stages is much more common.Citation25Citation26
Training for primary health care providers including midwives and health promoters, as well as strengthening the education of doctors and nurses on breast health and clinical examination, could support earlier detection.Citation40 Both the education of women and of providers must take into account local culture, as well as make-up of the population, including variations based on body-mass index, skin colour, age, familial cancer history and reproductive history.
Education and awareness campaigns and early detection interventions, should be provided through existing anti-poverty and health programmes and to families, including education for men. In Mexico, the key programme for this is Oportunidades, which offers primary health care services and health education to the majority of the poor (five million families).Citation48
Non-governmental organisations have an important role to play in developing and implementing an integrated response in Mexico. While there are several organisations specialised in breast cancer and working to provide information and build awareness, breast cancer appears to be much less integrated into the programmes of NGOs providing other types of services to at-risk women.Citation15Citation39 Enormous social capital can be created by these institutions in many areas, including lobbying government, increasing awareness and reaching the poorest segments of the population regarding the health of women in Mexico.
In the areas of mammography , communication technology provides an important opportunity for improving access and quality by transferring information online from the site where the examination is carried out to a site where expert radiologists can interpret the films. A short-term restriction on such an approach is the lack of technology required to send the images.
On the treatment side, a comprehensive national and local analysis is required to identify available resources. In Mexico, the legislation and norms for universal access are in place. Still, there is a long way to go to translate this into access to appropriate, high-quality health services. At the same time, both women and primary providers must be made more aware that these entitlements exist, in order to encourage women to seek care and institutions to expand their capacity to provide appropriate services. Additional tertiary level centres must be equipped and developed into regional centres of excellence.
The evidence from Mexico shows that breast cancer is a key challenge to the health of women, as well as to the health system. Early detection, through a combination of interventions, is essential to meet this challenge. In turn, improving early detection requires an articulated social response, appropriate to the conditions and resources available. These efforts must include women, family members, patients, providers and policy makers. As has been the case in North America, in Mexico as in other countries, advocacy, particularly by women, can be a powerful tool in combating the disease.
Acknowledgements
We thank Maria Cecilia Gonzalez and Liv Lafontaine for excellent research assistance.
Notes
* While some of this increase may be associated with improved data collection and reporting, the overall trend is unlikely to be explained by this.
* There is a difference in the wording of the question between the two surveys. In 2000, in parenthesis, the question asks about clinical examination, including mammograms, while in 2006 the question asks specifically about mammography. The rest of the question is exactly the same: “During the previous 12 months, did you visit a unit for preventive medicine for…” We assume that this difference is likely to underestimate improvements in coverage.
References
- CD Mathers, AD Lopez, CJL Murray. The Burden of Disease and Mortality by Condition: Data, Methods, and Results for 2001. 2006; Oxford University Press: New York, 45–93.
- R Lozano, FM Knaul, H Gómez Dantés. Tendencias en la mortalidad por cáncer de mama en México, 1979–2006. Observatorio de la Salud. Documento de trabajo. 2008; Competitividad y Salud, Fundación Mexicana para la Salud.
- Secretaría de Salud. Norma Oficial Mexicana NOM-041-SSA2.2002. Para la prevención, diagnóstico, tratamiento, control y vigilancia epidemiológica del cáncer de mama. 17 Septiembre 2003. At: <www.salud.gob.mx/unidades/cdi/nom/041ssa202.html. >. Accessed 25 July 2008.
- Instituto Mexicano del Seguro Social. Ley del Seguro Social. IMSS, 2006. At: <www.imss.gob.mx/NR/rdonlyres/15E5C49C-4938-4966-814D-D75878A6CCF1/0/LeySeguroSocial.pdf. >. Accessed 4 October 2008.
- Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado. Nueva Ley del ISSSTE. 2007. At: <www.issste.gob.mx/nuevaley/leydelissste.pdf. >. Accessed 4 October 2008.
- Instituto Nacional de Salud Pública y Secretaría de Salud. Encuesta Nacional de Salud, 2000. Vivienda, población y utilización de servicios de salud. 2003; INSP: Cuernavaca.
- Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición, 2006. 2007; INSP: Cuernavaca.
- J Frenk, E González-Pier, O Gómez-Dántes. Comprehensive reform to improve health system performance in Mexico. Lancet. 368(9546): 2006; 1524–1534.
- FM Knaul, J Frenk. Health insurance in Mexico: achieving universal coverage through structural reform. Health Affairs. 2: 2005; 1467–1476.
- J Frenk, F Knaul, O Gómez-Dantés. Fair financing and universal social protection: the structural reform of the Mexican health system. Working Paper. 2004; Ministry of Health: Mexico City.
- Secretaría de Salud. Catalogo Universal de Servicios de Salud. México, DF, 2008. At: <www.salud.gob.mx/unidades/dgpfs/contenido.php?sccsgd_id=4. >. Accessed 25 July 2008.
- Instituto Nacional de Salud Pública. Evaluación del Sistema de Protección Social en Salud, 2007. INSP/SSA. Cuernavaca, 2008.
- Poblano-Verastegui O, Figueroa-Perea JG, López-Carrillo L. Institutional factors contributing to the utilization of breast clinical examination. Salud Pública de México, 2004;46(4):294–305.
- Ortega D. Diagnóstico tardío del cáncer de mama en México: desencuentro entre las mujeres y los servicios de salud. En: Salud Reproductiva: temas y debates. Compiladores: Bronfman M, Denman C. Cuernavaca: Instituto Nacional de Salud Pública; 2003. pp.157-80.
- Observatorio de la Salud (Instituto Carso de la Salud y Fundación Mexicana para la Salud) e Instituto Nacional de Salud Pública. Reunión de Intercambio de Experiencias de la investigación en Cáncer de Mama en México. Instituto Nacional de Salud Pública, Cuernavaca, 2008. At: <www.funsalud.org.mx/competitividad/principal.html. >. Accessed 4 October 2008.
- Secretaría de Salud. Programa de Acción: Cáncer de Mama. México, 2002.
- American Cancer Society. Breast Cancer Facts & Figures 2007–2008. 2008; American Cancer Society: Atlanta. At: <www.cancer.org/downloads/STT/BCFF-Final.pdf. >. Accessed 25 July 2008.
- Secretaría de Salud. Defunciones,1979–2006. Sistema Nacional de Salud, Secretaría de Salud, México, DF, 2008. At: <http://sinais.salud.gob.mx/basesdedatos/index.html. >. Accessed 25 July 2008.
- World Health Organization. WHO Statistical Information System (WHOSIS). 2008; WHO: Geneva. At: <www.who.int/whosis/en/index.html. >. Accessed 25 July 2008.
- OE Ahmad, C Boschi-Pinto, AD Lopez. Age standardization of rates: a new WHO standard. GPE Discussion Paper Series No 31. 2000; WHO: Geneva.
- Consejo Nacional de Población (CONAPO). Proyecciones de la Población de México 1950–2050. CONAPO, México, DF, 2008. At: <www.conapo.gob.mx/. >. Accessed 25 July 2008.
- F Franco Marina, R Lozano, B Villa. La Mortalidad en México, 2000–2004. Muertes Evitables: magnitud, distribución y tendencias. 2006; Dirección General de Información en Salud, Secretaría de Salud: México DF.
- P Porter. Westernizing women’s risk? Breast cancer in lower-income countries. New England Journal of Medicine. 358: 2008; 213–216.
- ML Brown, SJ Goldie. Chapter 29. Health service interventions for cancer control in developing countries. DT Jamison, JG Bremen, AR Meashan. Disease Control Priorities in Developing Countries. 2nd ed., 2006; Oxford University Press/World Bank: New York.
- S Rodríguez-Cuevas, C Macías, S Labastida. Cáncer de mama en México: ¿enfermedad de mujeres jóvenes?. Ginecología y Obstetricia de México. 68(5): 2000; 185–190.
- S Rodríguez-Cuevas, M Capurso-García. Epidemiología del cáncer de mama. Ginecología y Obstetricia de México. 74: 2006; 585–593.
- J Ferlay, P Bray, P Pisani. GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide. IARC Cancer Base No.5, Version 2.0. 2004; IARC Press: Lyon.
- E Lazcano-Ponce. Nuevas alternativas de prevención secundaria del cáncer cervical. Salud Pública de México. 49: 2007; 32–34. Ed. Especial: VII congreso de investigación en salud pùblica.
- L López-Carrillo, L Torres-Sánchez, M López-Cervantes. Identificación de lesiones mamarias en México. Salud Pública de México. 43(3): 2001; 199–202.
- Secretaría de Salud. Programa de acción: cáncer de mama, 2007–2012. Secretaría de Salud. México, 2007.
- Knaul FM, Lozano R, Gómez Dantés H, et al. El cáncer de mama en México: cifras para la toma de decisiones. Observatorio de la Salud. Documento de trabajo. Competitividad y Salud, Fundación Mexicana para la Salud; 2008.
- WD Dupont, DL Page. Risk factors for breast cancer in women with proliferative breast disease. New England Journal of Medicine. 312(3): 1985; 146–151.
- K McPherson, CM Steel, JM Dixon. ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ. 321: 2000; 624–628. [PMID: 10977847].
- AC Hidalgo-Martínez. El cáncer cérvico-uterino, su impacto en México y el porqué no funciona el programa nacional de detección oportuna. Revista Biomedica. 17: 2006; 81–84.
- World Health Organization. World Health Report 1995. Bridging the Gaps. 1995; WHO: Geneva. At: <www.who.int/whr/1995/en/whr95_en.pdf. >.
- Nigenda G, Caballero M, González LM. Social process of breast cancer in Mexico. Research protocol. National Institute of Public Health, Cuernavaca, 2008.
- Grupo Reto. México, DF, 2008. At: <www.gruporeto.org/gruporeto.htm. > Accessed 5 October 2008.
- Fundación CIM*AB. México, DF, 2008. At: <www.fundacioncima.org. > Accessed 5 October 2008.
- Observatorio de la Salud (Instituto Carso de la Salud y Fundación Mexicana para la Salud) e Instituto Nacional de Salud Pública. Reunión de Intercambio de Experiencia en Cáncer de Mama en México con ONGs. FUNSALUD, Méx. 2008. At: <www.funsalud.org.mx/competitividad/principal.html. >. Accessed 4 October 2008.
- Unger-Saldaña K. Factores asociados al retraso en la atención médica de pacientes con cáncer de mama. Universidad Nacional Autónoma de México. Tesis de Maestría. UNAM, México, DF, Noviembre 2006.
- Breast Health Global Initiative. Report from the Breast Health Global Initiative. Seattle: Fred Hutchinson Cancer Research Center/Susan G Komen for the Cure, 2008.
- I Romieu, E Lazcano-Ponce, L Sánchez-Zamorano. Carbohydrates and the risk of breast cancer among Mexican women. Cancer Epidemiology, Biomarkers & Prevention. 13(8): 2004; 1283–1289.
- D Ortega-Altamirano, L López-Carrillo, M López-Cervantes. Estratégias para la enseñanza del autoexamen del seno a mujeres en edad reproductiva. Salud Pública de México. 42: 2000; 17–25.
- JP Kösters, PC Gøtzsche. Regular self-examination or clinical examination for early detection of breast cancer. Cochrane Database of Systematic Reviews. 2003; 2. Art. No. CD003373.
- S Robles, E Galanis. Breast cancer in Latin America and the Caribbean. Pan American Journal of Public Health. 11(3): 2002; 178–185.
- D Josefson. Breast self examination does not improve cancer survival. BMJ. 325: 2002; 793.
- DB Thomas, DL Gao, RM Ray. Randomized trial of breast self-examination in Shanghai: final results. Journal of the National Cancer Institute. 94: 2002; 1445–1457.
- Secretaría de Desarrollo Social. Oportunidades. SEDESOL, México, DF, 2008. At: <www.oportunidades.gob.mx/. >. Accessed 29 July 2008.