Abstract
Deaths resulting from unsafe induced abortions represent a major component of maternal mortality in countries with restrictive abortion laws. Delays in obtaining care for maternal complications constitute a known determinant of a woman’s risk of death. However, data on the role of delays in providing care at health care facilities are sparse. The association between the cause of maternal death (abortion versus post-partum haemorrhage or eclampsia) and the time interval between admission to hospital and the initiation of treatment were evaluated among women who died at the Maternité du Centre Hospitalier de Libreville, Gabon, between 1 January 2005 and 31 December 2007. The women’s characteristics and the time between diagnosis of the condition that led to death and the initiation of treatment were compared for each cause of death. After controlling for selected variables, the mean time between admission and treatment was 1.2 hours (95% CI: 0.0—5.6) in the case of women who died from post-partum haemorrhage or eclampsia and 23.7 hours (95% CI: 21.1—26.3) in the case of women who died of abortion-related complications. In conclusion, delay in initiating care was far greater in cases of women with complications of unsafe abortion compared to other pregnancy-related complications. Such delays may constitute an important determinant of the risk of death in women with abortion-related complications.
Résumé
Les décès dus aux avortements provoqués à risque représentent une composante majeure de la mortalité maternelle dans les pays où les lois sur l'avortement sont restrictives. Le retard de prise en charge thérapeutique des complications induites par ces avortements constitue un déterminant connu du risque de mourir pour ces femmes. Cependant, les données sur le rôle de ce retard d’administration des soins sont clairsemées. L'association entre la cause du décès maternel (avortement, hémorragie du post-partum et éclampsie) et l’intervalle entre l’admission à hôpital et l'initiation du traitement a été évaluée parmi les femmes décédées à la maternité du Centre hospitalier de Libreville, au Gabon, entre le 1er janvier 2005 et le 31 décembre 2007. Les caractéristiques de ces femmes et les délais de prise en charge ont été comparés pour chaque cause de décès. Il ressort que le temps moyen écoulé entre l’admission et le début du traitement était de 1,2 heure (95% IC: 0,0-5,6) pour les femmes mortes d'hémorragie du post-partum et d’éclampsie, contre 23,7 heures (95% IC : 21,1-26,3) pour les femmes mortes de complications d’avortement. En conclusion, le retard de prise en charge était beaucoup plus long dans le cas des femmes présentant des complications d’avortement à risque que pour les deux autres complications obstétricales étudiées. De tels délais pourraient constituer un facteur de risque élevé de décès pour les femmes avec complications de avortement.
Resumen
Las muertes provocadas por complicaciones de aborto inseguro representan un importante componente de la mortalidad materna en los países con leyes restrictivas sobre aborto. El retraso en obtener asistencia es un conocido determinante del riesgo de muerte materna, pero hay muy poca información sobre el papel de las demoras en la prestación de servicios después que la mujer llega al establecimiento de salud. Se estudió la asociación entre la causa de muerte (aborto comparado con hemorragia posparto o eclampsia) y el intervalo de tiempo entre la admisión al hospital y el inicio de tratamiento entre las mujeres que murieron en el Centre Hospitalaire de Libreville, en Gabón, entre el 1 de enero de 2005 y el 31 de diciembre de 2007. Se compararon las características de las mujeres y el tiempo entre ingreso e inicio de tratamiento para cada causa de muerte. Después de controlar por variables seleccionadas, el intervalo medio entre el diagnóstico y el comienzo del tratamiento fue de 23.7 horas (95% CI 21.1-26.3) en los casos de aborto y de 1.2 (95% CI 0.0-5.6) en los casos de eclampsia o hemorragia posparto. Se concluye que la demora en iniciar el tratamiento fue mucho mayor para las mujeres con complicaciones de aborto inseguro que en aquéllas con las dos otras complicaciones. Esta demora puede constituir un importante determinante de muerte entre las mujeres con complicaciones de aborto.
According to the World Health Organization (WHO), about 13% of all maternal deaths are associated with unsafe abortion and almost all take place in countries with restrictive abortion laws. In contrast, in countries with liberal laws, abortion-related deaths are very low or negligible.Citation1 It is commonly thought that in countries with restrictive laws women die due to the unsafe conditions in which the abortion is carried out. Little attention has been paid to whether care is provided at all or to the quality of the care received when women with complications seek help at health care facilities following a clandestine abortion, particularly with respect to how post-abortion care affects the risk of death in countries where abortion is mostly illegal.
It is widely recognized that to prevent maternal mortality the sooner appropriate care is provided the higher the chances of survival. The effect of delays in providing care has long been accepted as a principal determinant of maternal death. Three typical forms of delay have been described: (1) delay in the woman’s decision to seek care, (2) delay in the woman arriving at a health care facility, and (3) delay in the provision of adequate care.Citation2
A review of studies carried out in developing countries found that distance and cost were major obstacles in the decision to seek care and reach a facility.Citation3 On the other hand, there is evidence from Bolivia and Argentina that women seeking medical care for complications of unsafe abortion are often left waiting for treatment for longer periods of time than other patients.Citation4Citation5 A longer waiting period prior to treatment — whether related to treatment exigencies or discrimination against women who have had an abortion — may increase women’s risk of dying, the third form of delay.
To the best of our knowledge, however, there are no publications from developing countries with restrictive abortion laws that demonstrate the possible effect of delay in providing care for abortion-related complications on the risk of dying. With the aim of contributing to greater understanding of the possible effect of discrimination on abortion-related mortality, this study compared the time between diagnosis of the condition that led to maternal death and the initiation of care in a large maternity hospital in Libreville, Gabon, as a consequence of post-partum haemorrhage (PPH) or eclampsia as opposed to complications of unsafe abortion.
Subjects and methods
Gabon is a small country on the Atlantic coast of Central Africa with a population of 1.34 million inhabitants, about 35% of whom live in the capital city Libreville and a further 25% who reside in the Estoire province, in which Libreville is situated. Gabon has the highest per capita income in sub-Saharan Africa and several social indicators reflect the positive economic conditions of the country. Over 90% of children are in school and over 70% of women are literate. Up to 95% of all births are supervised by skilled birth attendants and 80% of pregnant women attend four or more antenatal consultations.
This study was carried out at the Maternité du Centre Hospitalier de Libreville (CHL) and included all women who died during pregnancy, labour or in the post-partum period up to 42 days following delivery at CHL in the period between 1 January 2005 and 31 December 2007. Although there are three other public hospitals in Libreville, all were undergoing renovations at the time of the study and were closed. CHL was therefore the only maternity hospital serving Libreville and the whole Estoire province during the study period. For that reason, it was usually overcrowded, performing an average of 30 deliveries and 6—10 major surgical procedures daily.
Data on all the women who died and on the circumstances surrounding their deaths were prospectively recorded during this three-year period by a maternal mortality committee, which began meeting at CHL as from 1 January 2005. The committee was chaired during the three years that the study took place by the obstetrician in charge of the delivery room, who is one of the co-authors of this paper (SMT). Meetings to review each maternal death took place on the day following the death in any part of the hospital, in accordance with 2004 WHO guidelines.Citation6 Participants included the physicians on duty at the time of the death, the chief midwife, the midwife responsible for the delivery and the health care team on duty at the time in the surgical theatre. Maternal death reviews continue to date; however, a cut-off date of 31 December 2007 was established for the purposes of this study.
Data on the women’s characteristics, the mechanism of admission to hospital (whether by the woman herself or by referral from a primary care facility), time of admission and time of initiation of treatment (medical or surgical) were obtained from hospital records or directly from staff involved and recorded on forms specifically designed for this purpose and stored in the committee’s files. The time of admission to hospital and the time of initiation of treatment for the main complication that resulted in death were recorded, and the time that elapsed between these.
All women were cared for by a team consisting of a senior gynaecologist, a resident in obstetrics and gynaecology and three interns. If the recommended treatment was surgical, the woman was transferred to the surgical theatre and the time at which surgery began was recorded on the anaesthesia form and in the surgical theatre records. This information was later transcribed onto the committee’s form as representing the time at which treatment was initiated. When the treatment was medical (antibiotics, blood transfusion, anticonvulsants), the patient was transferred to the gynaecology ward or the intensive care unit and the time at which administration of the medicines was begun was recorded as the time of initiation of treatment.
Characteristics of the women recorded on the forms were: age, parity, marital status (with or without a long-term partner), occupation (student or other), and mechanism of admission to hospital (either self-referral or referred).
The main causes of death were analysed. The women’s characteristics and the time between diagnosis of the condition that led to death and the initiation of treatment were compared for each cause of death. A multiple regression analysis was carried out to identify the risk factors associated with the time between diagnosis and treatment. The women’s characteristics and their cause of death were included as independent variables. Finally, the mean delay in implementing care for women who died from abortion-related complications or other causes was estimated following adjustment for all other variables.
Findings
Seventy-six maternal deaths occurred in the three years of the study – 25 in 2005, 26 in 2006 and 25 in 2007. The main causes of death were post-partum haemorrhage (23 women or 30.3%), eclampsia (20 women or 26.3%) and abortion-related complications (19 women or 25%). The abortions were induced in all cases, as reported by the patient herself or by a member of her family. Twelve women died from indirect causes, principally AIDS-related, and two were as a result of ectopic pregnancy.
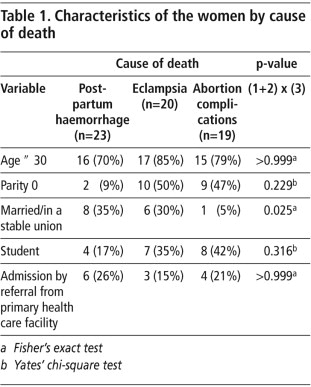
shows the characteristics of the women who died. Most of them were under 30 years of age. Only two of the 23 women who died from post-partum haemorrhage were nulliparas, while half of those who died from eclampsia and from abortion-related complications had not previously given birth. A third of those who died from post-partum haemorrhage and eclampsia had been married or in a stable union, but only one of the 19 who had abortion-related complications had been married or in a stable union. The difference in the proportion of unmarried women among those who died from abortion complications compared with the other causes was statistically significant (p= 0.025).About 20% of the women were referred from another health care institution (Table 1). These women had all initially consulted at primary health care clinics in the city of Libreville or nearby in the Estoire province.
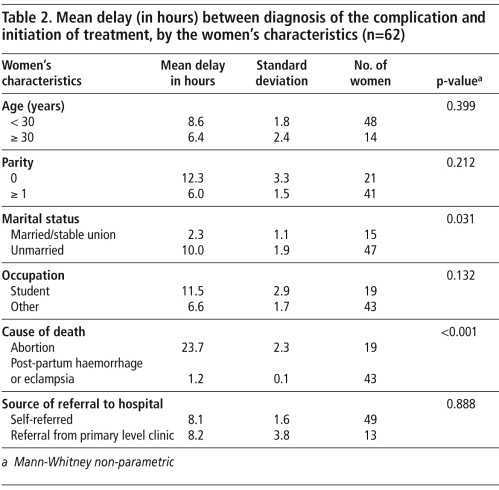
There was no difference in the mean time between diagnosis of the condition that led to death and the initiation of treatment according to age or the mechanism of admission to hospital. The mean delay in initiating treatment was double in nulliparas compared to multiparas and in students compared to women in paid employment; however, these differences were not statistically significant. The time between diagnosis and the initiation of treatment was four times longer in unmarried women compared to married women (p=0.0132) and 20 times longer in women who died from abortion-related causes compared to those who died from post-partum haemorrhage or eclampsia (Table 2
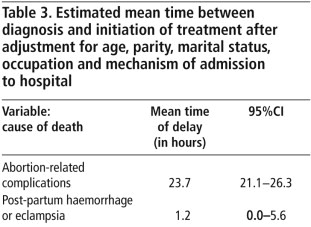
).Multiple regression analysis, including all the variables analysed in Table 2, revealed that it was only cause of death (unsafe abortion compared to post-partum haemorrhage or eclampsia) that was associated (p<0.001) with a delay in initiating care (not shown in table). The estimated time between diagnosis and initiation of care in the cases of the women who died from abortion complications remained the same as in the bivariate analysis, even with adjustment for all the other factors recorded: 23.7 hours (95% CI: 21.1-26.3) for abortion and 1.2 hours (95%CI: 0.0-5.6) for eclampsia and post-partum haemorrhage together (Table 3
).The shortest delay observed in cases of death resulting from post-partum haemorrhage or eclampsia was one hour and the longest two hours. The shortest delay for the women who died from abortion-related causes was 11 hours and the longest 48 hours.
Discussion
Although no specific qualitative study was intended, the observation of the physicians at CHL who conducted this study was that women with post-partum haemorrhage and eclampsia were admitted to the surgical theatre or the intensive care unit faster than women suffering from abortion-related complications. There is a sense that the cultural stigmatisation of women who have abortions affects the attitude of all health care personnel.
The findings described here clearly show that women who died of complications resulting from abortion were not given attention in as timely a manner as those needing care for other pregnancy-related complications at CHL. Given the relevance of the length of time between admission to hospital and the initiation of treatment as a principal determinant of life or death, it is hard not to conclude that postponement of treatment in the case of women who died from abortion-related complications in CHL was partially responsible for the fatal outcomes.
As in many other developing countries where abortion is legally restricted, induced abortion is condemned by conservative religious leaders and socially rejected in Gabon, despite being frequently practised.Citation7 Moral issues and the disapproval of health care personnel with respect to induced abortion, particularly in the case of adolescents, has already been described in other countries of sub-Saharan Africa where abortion laws are restrictive.Citation8Citation9 No data exist, however, on the possible implications of such disapproval for the quality of care offered to women seeking help for abortion-related complications.
All the factors described in the medical literature as representing possible causes of delay in the provision of appropriate health care affect all women who die during pregnancy, delivery or post-partum, irrespective of the complication that resulted in the maternal death. Our findings show that in the case of women with abortion-related complications, an even more important determinant of the delay in initiating care may be discrimination against women who have had an abortion.
Although the mistreatment of women who request hospital care for abortion-related complications and the inherent cruelty of this mistreatment has been described before, for example in Argentina,Citation5 Citation10 the possible association of this mistreatment with a higher risk of maternal death has not previously been investigated. To the best of our knowledge this is the first report to clearly show that women identified as having undergone an abortion may be subject to a higher risk of death and actually die as a result of long delays in initiating care.
The mean time of 24 hours between diagnosis and treatment found in this study suggests that women with severe complications of abortion were left to suffer before receiving the care they needed to survive. This was not due to any lack of life-saving equipment or supplies, or of properly trained personnel, because no such delays were observed in the treatment of the women who died from other causes in the hospital in the same time period. It appears that in the difficult environment of an overcrowded maternity ward, where several emergency cases may compete for attention, the stigma of illegal abortion may lead staff to overlook women with abortion complications without considering the potentially fatal consequences of doing so.
It may be argued that we are dealing here with a biased sample of the worst cases in which the delay in providing care contributed to the woman’s death, and that other women with abortion-related complications who did not die may not have experienced similar delays. It is hard to believe, however, that less severe cases were treated more expeditiously than those with more serious complications. Although data on this are also scarce, one study in Zimbabwe did find that women who died from abortion-related complications had received a better quality of care than those who did not die.Citation11
We hope that the publication of these findings will stimulate others toimplement similar maternal death audits to those routinely carried out at CHL.Moreover, we urge measures to be taken to identify and prevent such discriminatory practices as those witnessed inCHL. The results of a qualitative study currently being undertaken in the hospital will permit better understanding ofthe attitudes of staff, and training for all hospital personnel, with the aim of minimising delays inimplementing care for all patients without discrimination. In the near future, we expect to be able to show dramatic changes in the way women with complications of unsafe abortion are treated in CHL and a corresponding decrease in abortion-related mortality.
References
- World Health Organization. Unsafe Abortion. Global and regional estimates of incidence of unsafe abortion and associated mortality in 2003. 5th ed., 2007; WHO: Geneva.
- S Thaddeus, D Maine. Too far to walk: maternal mortality in context. Social Science and Medicine. 38(8): 1994; 1091–1110.
- D Barnes-Josiah, C Myntti, A Augustin. The “three delays” as a framework for examining maternal mortality in Haiti. Social Science and Medicine. 46(8): 1998; 981–993.
- VH Camacho, AG Murillo, M Paz. Expandiendo opciones de Planificación Familiar: Diagnóstico cualitativo de la atención en salud reproductiva en Bolivia. Secretaría Nacional de Salud. Ministerio de Desarrollo Humano. 1996; WHO: Geneva.
- S Chiarotti, MG Jurado, A Alucia. Con todo el aire. Reporte de derechos humanos sobre atención en salud reproductiva en hospitales públicos. November. 2003; Instituto de Genero, Derecho y Desarrollo: Buenos Aires, Argentina.
- C Bullough, W Graham. Facility based maternal deaths review: learning from death occurring in health facilities. Beyond the Numbers: Reviewing Maternal Deaths and Complications to Make Pregnancy Safer. 2004; WHO: Geneva.
- Barrère, M. Avortement. In Gabon. DHS, 2000. At: <www.meauresdhs.com>.
- PT Mngadi, E Faxelid, IT Zwane. Health providers' perceptions of adolescent sexual and reproductive health care in Swaziland. International Nursing Review. 55(2): 2008; 148–155.
- LU Warenius, EA Faxelid, PN Chishimba. Nurse-midwives' attitudes towards adolescent sexual and reproductive health needs in Kenya and Zambia. Reproductive Health Matters. 14(27): 2006; 119–128.
- C Steele, S Chiarotti. With everything exposed: cruelty in post-abortion care in Rosario, Argentina. Reproductive Health Matters. 12(24 Suppl.): 2004; 39–46.
- C Mudokwenuy-Rawdon, VJ Ehlers, MC Bezuidenhout. Factors influencing post abortion outcomes among high-risk patients in Zimbabwe. Curationis. 28(4): 2005; 74–85.