Abstract
Abstract
A case study of Muhammadiyah's Islamic charitable health services in the islands of Java and Sumatra, Indonesia, was undertaken in 2008, to assess the impact of privatization of health care on this socially-oriented service provider, especially in terms of access for the poor. Findings presented here relate primarily to the effects on Muhammadiyah's maternal and child health and contraceptive services. In order to survive and thrive amidst private and public competitors, Muhammadiyah's primary care units, mostly consisting of maternal and child health centres and maternity clinics, when not closed altogether, have been directed toward providing curative hospital services, and more expensive and sometimes unnecessary treatment. A shift in the patient population away from the poor has also occurred, as market pressures transform this charitable enterprise into a commercial one, prejudicing reproductive health care and reducing access for those most in need. An improved stewardship role by government is needed to regulate the private sector, along with serious thinking about the future of primary and preventive care and health promotion, including for comprehensive reproductive health care. The neglect of these core primary care elements in Indonesia may worsen as privatization proceeds and profit considerations become more pressing with increased competition.
Résumé
Une étude de cas des services de santé caritatifs islamiques de Muhammadiyah sur les îles de Java et Sumatra, Indonésie, a évalué en 2008 l'impact de la privatisation des soins de santé sur ce prestataire de services à vocation sociale, en particulier du point de vue de l'accès des pauvres. Les conclusions présentées ici concernent principalement les retombées sur les services contraceptifs et de santé maternelle et infantile de Muhammadiyah. Afin de survivre face à des concurrents privés, les unités de soins primaires de Muhammadiyah, consistant essentiellement en centres de santé maternelle et infantile et en maternités, quand ils n'ont pas été tout simplement fermés, assurent désormais des services hospitaliers curatifs, et un traitement plus onéreux et parfois superflu. La population de patients a aussi changé pour compter moins de pauvres, alors que les pressions du marché transforment cette łuvre caritative en entreprise commerciale, nuisant aux soins de santé génésique et réduisant l'accès des personnes qui en ont le plus besoin. Les pouvoirs publics doivent mieux jouer leur rôle d'administrateur afin de réguler le secteur privé; il convient aussi de réfléchir sérieusement à l'avenir des soins de santé primaires et préventifs et de la promotion de la santé, notamment pour des soins génésiques complets. Le désintérêt pour ces éléments centraux des soins de santé primaires en Indonésie pourrait s'aggraver avec la poursuite de la privatisation et la recherche plus pressante du profit face à une concurrence accrue.
Resumen
En el año 2008 se realizó un estudio de caso de los servicios sanitarios benéficos de Muhammadiyah Islámico en las islas de Java y Sumatra, en Indonesia, con el fin de evaluar el impacto de la privatización de los servicios de salud en este prestador de servicios con conciencia social, especialmente con relación al acceso para las personas pobres. Los hallazgos presentados aquí están relacionados principalmente con los efectos en los servicios de salud materno-infantil y anticonceptivos de Muhammadiyah. A fin de sobrevivir y prosperar entre competidores privados, las unidades de atención sanitaria primaria de Muhammadiyah, la mayoría centros de salud materno-infantil y clínicas de maternidad, cuando no son cerradas, han sido dirigidas hacia proporcionar servicios curativos hospitalarios, así como tratamiento más costoso y a veces innecesario. Además, la población de pacientes se ha desviado de las personas pobres, a medida que las presiones del mercado transforman a esta empresa benéfica en una comercial, perjudicando los servicios de salud reproductiva y reduciendo el acceso para las personas más necesitadas. Es necesario que el gobierno desempeñe un mejor papel administrativo para regular al sector privado y que piense seriamente en el futuro de la atención primaria y preventiva y la promoción de la salud, incluso para los servicios de atención integral a la salud reproductiva. El descuido de estos importantes elementos de la atención primaria en Indonesia podría empeorar a medida que continúa la privatización y que las consideraciones de ganancias se vuelven cada vez más apremiantes según va aumentando la competencia.
The size and reach of private health care services in Indonesia is considerable. About half, or 657, of the 1,320 hospitals counted in 2008 belonged to the private sector.Citation1 Private practices, run by physicians, nurses and midwives, with or without an official permit, can be found in the most far-flung regions,Citation2 and patients can choose from among a great variety of informal providers, ranging from drug-sellers to traditional herbalists, masseurs, birth attendants and healers. Charitable, faith-based groups also play an important role in health care delivery, offering a wide array of services across the country. They continue the medical tradition of Christian missions and early Muslim charities, which contributed to the introduction and expansion of biomedicine in Indonesia in the 19th and 20th centuries.
The growth of the private sector in the last two decades has been impressive. Confronted with increasing health care costs, the Indonesian government has opted to encourage greater private participation and commercialization of some public services, rather than increasing the public health budget, which is currently among the lowest in the region.Citation3 In the 1990s, new regulations liberalized hospital ownership and allowed public health units, especially hospitals, to charge their own fees and manage revenues.Citation1,4,5 Since the formation of the ASEAN Free Trade Area (AFTA) in 1992 and the opening of the health sector to foreign investment up to a 49% hospital ownership limit in 2000,Footnote* relatively new players, such as local construction and property development companies, have joined with foreign parties in establishing private hospitals in major cities across Indonesia.Citation1,4–6
In recent years, the number of private hospitals has been increasing at a rate of about 2% per year and their patients at an annual rate of 7%, with an estimated total of 3.5 million patients projected by 2010.Citation1Citation5 Across Indonesia, two-thirds of hospital ambulatory care, half of hospital contacts and 30–50% of deliveries are provided by the private sector at higher costs than in the public sector, but not always with higher quality.Citation7Citation8 This growth can be attributed to the still-limited number of hospital beds (around 1:1,580 in 2009), increasing burden of chronic diseases with the ageing population, rising income levels, and perceived poor quality of public primary health care, motivating patients to seek hospital care even for minor problems.Citation8
The under-funded and under-staffed public health system struggles to provide quality services. Indonesian health experts expect the government to focus on improving primary health care.Citation7Citation9 However, increasing dependence on user fees to cover operating expenses and raise revenues is leading to an emphasis on hospital care and expansion of curative care in public health centres at the cost of preventive and promotive functions. The introduction of a government-run health insurance scheme for the poor in 2005, now called Jaminan Kesehatan Masyarakat, has increased utilization of public health facilities from 46.6% in 2004 to 65% in 2007 for in-patient curative services, but financial constraints remain.Citation3 In the 2007 National Socioeconomic Survey (Susenas) 45% of people reported that during their last episode of illness they relied on self-treatment or traditional medicine while 13% sought no treatment at all.Citation9
To better understand the impact of privatization on health care provision and utilization, the World Bank's Jakarta office carried out a review of the Indonesian health system in 2007–08, including charitable health services within the private sector. This included a commissioned case study of Persyarikatan Muhammadiyah (Association of Followers of Prophet Muhammad, or Muhammadiyah in short), because of its consistent engagement in the health sector, extensive network of private health outlets and concern for maternal and child health (MCH).Citation10 Founded in 1912 in Yogyakarta, Central Java, this Sunni Islam reformist socio-religious association is the second largest Muslim organization in Indonesia with an estimated 29 million members and chapters and sub-chapters down to the district, sub-district and village levels.Citation11Citation12 It comprises seven autonomous organizations, the largest of which is Aisyiyah, a semi-independent, parallel structure for women members. Established in 1917, Aisyiyah aims to promote women's and family welfare from an Islamic perspective, including MCH and family planning services.Citation13
The case study analyzed how Muhammadiyah and AisyiyahFootnote† tried to address human resources and service delivery issues, and how their health services compared with other private options and with the public sector, especially regarding the extent to which they were reaching the poor and disadvantaged groups. Between May and August 2008, published and gray literature on Muhammadiyah and the health sector in Indonesia, in both English and Indonesian, was gathered from various libraries, organizations and electronic sources and analyzed. Selected Muhammadiyah and Aisyiyah health care facilities across Java (in Jakarta, Yogyakarta, Bantul, Klaten, Solo, Surabaya, Sidoarjo, and Malang) and in Pekanbaru in East Sumatra were visited and in-depth interviews with 60 Muhammadiyah and Aisyiyah leaders, officers, and providers were undertaken. Informal interviews were also held with other stakeholders, especially users and non-users of the health facilities, to understand their health care-seeking behaviour and assessment of the services provided.Citation10
The insights presented in this paper are mainly derived from the observations and the information provided by the informantsFootnote** during the case study, with some additional knowledge gained this past year through informal conversations and conference attendance.Footnote* Only findings related to or affecting the provision of reproductive health services are presented.
Muhammadiyah and its charitable health enterprises
Along with education, health has always been a priority focus of Muhammadiyah as “the best way for propagating Islam, empowering the Islamic community and improving the social conditions of Muslims”.Citation14 The first health clinic was founded in 1923 in Yogyakarta to provide relief to the suffering.Citation12Citation15 This initial mandate was later expanded to “establish hospitals to help neglected sick people, while giving Islamic education to those who come for treatment”.Citation16 In this context, health care facilities are not only meant to assist the needy and poor, but are a means of worship and propagation of Islamic values. By providing faith-based health facilities that are professional and Islamic, Muhammadiyah strives “to enhance society's health standards so that people are in an optimal condition to worship and able to realize ideal Muslim families as part of the larger society”.Citation16
Muhammadiyah's health care activities boost its image as well as its finances, and figure prominently in its history. They serve as tangible good deeds to society, demonstrating Muhammadiyah's added value in comparison with other organizations, secular and not. As amal usaha (charitable enterprises), the financial performance of the health outlets is also pertinent to the sustainability of the entire organization. Their 10% annual profit is used for Muhammadiyah's organizational development, proselytizing activities, and cross-subsidy for social welfare activities, such as orphanages and retirement homes. The remaining profit is divided between funding for the health facilities themselves (75%) and bonuses for the management and staff (15%).Citation16 Increasingly, Muhammadiyah strives to transform existing facilities into commercial clinics, thriving on profit and able to compete with other providers in attracting a varied clientele.Citation12 A competitive orientation is encouraged in order for the charitable enterprises to meet growing societal expectations and succeed in an increasingly tight market economy.Citation17 Thus, health facilities' leaders and personnel are confronted with complex choices regarding what to prioritize, charitable or commercial goals.
From Yogyakarta, health facilities have multiplied to other regions of Indonesia forming a health care structure paralleling the public health system, with primary, secondary and tertiary care provided at village, sub-district, district and province level facilities. Hospitals are concentrated in provincial and district centres, polyclinics and maternity clinics in sub-districts, and MCH centres and health posts in villages and religious schools. However, differently from the public health system, these institutions form a referral system only insofar as they belong to the same chapter, or are satellite units of a larger facility. The most recent directory of Muhammadiyah health facilitiesCitation16 in 2005 records 272 self-governing health outlets of various types.Footnote† Polyclinics are the most numerous (98), followed by general and specialist (mostly MCH) hospitals (69) and maternity clinics (62), with the remainder consisting of MCH centres, health centres and health posts. Although Muhammadiyah health outlets are spread over 23 provinces, almost 70% are concentrated in Java. This Java-centric bias is particularly evident in hospital care, with 58 out of 69 hospitals located there, especially in urban areas because of the larger consumer market and the higher purchasing power of the population.Citation16
Traditional focus on reproductive health services
Traditionally, Muhammadiyah's facilities have had a strong focus on reproductive health. Aisyiyah's prominent (and gendered) role in health care provision, initiating a greater number of facilities than its parent organization, means that a majority of outlets have been specialist MCH hospitals and particularly maternity clinics and MCH centres. Community activities are also meant to pay attention to reproductive health, with integrated health posts incorporating antenatal care and family planning with child nutrition, immunization and diarrhoea control.
Aisyiyah also plays a pivotal role in many government and donor-supported, reproductive health outreach programmes, through mobilization of its women members. Most renown is their contribution to the promotion of family planning, making modern contraceptive methods accessible in villages through MCH centres and health posts, presenting contraception as instrumental for family health and thus the realization of the ideal Muslim family and society. In recent years, Aisyiyah has participated in projects promoting adolescent and women's reproductive health (albeit formally opposing abortion),Footnote* advocated women's protection from violence, and engaged in HIV/AIDS education.
Muhammadiyah's high profile in reproductive health, and more generally in primary health care, is set to change, however. An internal factor in this is that since 2000, Aisyiyah has taken a greater interest in developing hospitals and providing curative services, following the lifting of institutional restrictions on its doing so. Before then, while Muhammadiyah chapters had no limitations on establishing primary, secondary or tertiary facilities, Aisyiyah chapters could only found MCH centres or maternity clinics. There was no incentive to develop them into hospitals, as the parent organization would take over.Footnote† Most importantly, however, the ongoing shift toward privatization and decentralization of health care in Indonesia is compelling Muhammadiyah to invest more heavily in tertiary hospital care and reduce investments in primary health care.
Transforming MCH clinics into hospitals
A common, albeit not exclusive, pattern in the development of Muhammadiyah health facilities has been for them to start as MCH centres or maternity clinics and later add a range of curative services, gradually evolving into full-fledged hospitals. Prominent examples are PKU Muhammadiyah General Hospital in Yogyakarta and the Aisyiyah Muhammadiyah General Hospital in Padang.Citation6 This trend has intensified in recent years, even though public health experts and activists within Muhammadiyah have made efforts to prioritize and strengthen primary health care services.Footnote** In 2006, at the National Congress of the Muhammadiyah Health and Social Welfare Committee in Surakarta, a phased approach was elaborated to encourage the “establishment and development of smaller outlets as embryos of Muhammadiyah or Aisyiyah hospitals”.Citation18 Village chapters were to establish at least a health post, so as to introduce villagers to the organization and ensure referral to higher care levels. Sub-district chapters were to develop health centres into polyclinics and expand maternity clinics with curative services, and district and provincial chapters to upgrade existing facilities to hospitals. Finally, at the central level, efforts were to be made to enhance the quality of national hospitals as referral hospitals and teaching hospitals for students from Muhammadiyah medical, nursing and midwifery institutions.Citation18
Since then, a growing number of MCH centres and maternity clinics have evolved into hospitals. Although quantitative evidence is not available, recent literature and direct observations confirm this pattern.Citation10Citation12 During our field visits in Java and Sumatra, a majority of the original maternity clinics were in transition, having recently been inaugurated as hospitals. They still had only temporary permits, but aimed at earning full accreditation as small specialist hospitals by completing the minimum requirement of one specialist in each of the four essential clinical areas, namely internist, paediatrician, surgeon, and obstetrician/gynaecologist, available 24 hours a day. The facilities that are being prioritized for development are those strategically situated along main roads in urban and semi-urban, lower-middle class neighborhoods, or in district centres, with little investment being made in the maintenance and expansion of village-based outlets and outreach activities except for referral purposes or when supported by international donors.
This sweeping transformation is intended to enhance competitiveness with other faith-based and private providers, and take advantage of what is seen as a significant market opportunity.Footnote* In Indonesia, as in other parts of Asia, hospital care is considered to be one of the most lucrative segments of health care. Representatives of Muhammadiyah noted that strong demand makes curative and hospital care more profitable than MCH care, especially at the primary level. They adduce as evidence the fact that many Aisyiyah MCH centres and maternity clinics had become stagnant and, if not closed, began to attract clientele and profits when they added ambulatory and in-patient care.Footnote† These changes fit in with the desire of local governments to establish hospitals in their districts and are in line with Ministry of Health efforts to promote private sector involvement in hospital services. Most of the Muhammadiyah facilities we visited had recently received material support from the Health Ministry in the form of ambulances, equipment or building materials.
Although prioritizing hospital care may be justified by economic considerations, it conflicts with Muhammadiyah's social purposes, because it implies the sidelining of primary health care activities, including promotion of MCH and family planning, which directly benefit the poor at village level. MCH centres and health posts responsible for preventive care and reproductive health outreach activities are struggling with dwindling human and financial resources. When not closed, they become dependent on donor funding or people's willingness to bear higher out-of-pocket and transportation costs for health workers visiting their villages.Footnote** Provision of primary and reproductive health services in higher level district and provincial hospital facilities entails the concentration of services in more affluent urban areas, leading to an increase in service fees and transportation costs, with a consequent decline in access for poorer users. As such, the hospitalization trend also leads to a shift in patient population.
Towards a more affluent patient population
Muhammadiyah's health facilities were originally named, in rough translation, “helper of people in misery/suffering” and later “protector of people in misery”. These names associated ill-health with economic deprivation and stressed the need to serve the most disadvantaged. In recent years, however, new facilities are directed to have standardized names that include only the facility type, Muhammadiyah or Aisyiyah and the location, so as to promote a unified corporate image.Citation18 Could this be taken to mean that priorities have changed?
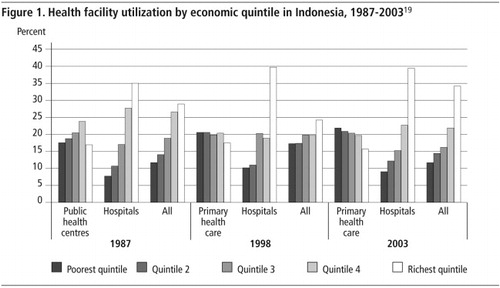
Indeed spending on secondary and tertiary hospital care cannot be considered pro-poor as the poor, when they do use services, opt for primary health care facilities as shown in .Citation19 Our observations of the patient population in the visited facilities in Java and Sumatra and our discussions with Muhammadiyah providers also revealed a shift in the target population from the poor to the lower middle class and higher. In the transition, Muhammadiyah facilities have acquired a diverse clientele. As noted by Hilman Latief:
“Unlike…[other Islamic] charitable clinics which merely cater to poorer families, Muhammadiyah's clinics have been transformed… into ‘private commercial clinics' whose clients vary, ranging from the well-off to underprivileged households… Catering for poorer families is not their main objective…” Citation12
The allocation of beds in its different hospital wards is set to change. Muhammadiyah hospitals generally have four classes of wards, rising from third class to VIP, which differ in the number of beds per ward, the degree of comfort provided, the type of care, e.g. for third-class wards generic drugs are used and for higher class wards brand name drugs, and the skills of the paramedical personnel employed (in third-class wards, lower skilled nurses or just graduated nurses, with student nurses allowed to assist, but not in other wards). The third-class wards are the most affordable for poor patients, but have a lower profit margin. As such, the proportion of third class ward beds is an indication of the social orientation of the hospitals and their intended patient population. In 2005, Muhammadiyah health facilities had the largest number of beds in second class wards, reflecting a focus on lower middle class patients, but 23–30% of beds were still in third class wards.Citation16 However, interviews with Muhammadiyah providers indicate that they have started to expand their first class and VIP wards for well-off patients, with one hospital in Jakarta planning to establish a VIP ward over four floors.Footnote* There are also plans to gradually reduce the number of third class beds to the national minimum required in private hospitals of 15–20%.Citation16
Continuing support for the poor?
The clientele shift is seen as necessary to increase the profit margin and enhance the development and sustainability of the facilities. The income of the health facilities is derived only in very small part from charitable donations, with patient fees as the main, regular source of income. As discussed earlier, profitability is an intrinsic element of Muhammadiyah health services, being essential not only to their functioning, but also to support the entire organization and its overall charitable activities.Citation11Citation18
Cross-subsidy is further being provided to less lucrative parts of services for the poor and needy. “Charity funds” are allocated for patients with demonstrated indigent status for whom fees would be reduced or payment allowed in installments. Given its social mission, Muhammadiyah cannot overlook the poor, even as it increasingly perceives them as a financial risk. Facilities therefore try to limit liability by gradually reducing the customary quota set for poor patients, as well as seeking funding from the government through the social health insurance scheme, which, as one hospital representative in Solo explained:
“is advantageous for the hospital, reducing our financial exposure, and enabling us to fill the third class wards, thus increasing their profitability.”
“It is commonplace that for basic health care… the hospital may foot the bill.… But for a serious disease, this hospital like other hospitals (charitable, private and government) very often can do nothing except leave the patients to find their own way to overcome their problems.” Citation12
Trend towards more expensive, commercial and unnecessary treatment
Hospital fees are complex and determined not only by the type of ward and the level of comfort provided, but also by the clinical pathways taken and the drugs prescribed. There are concerns that Muhammadiyah health facilities, not unlike other private providers in Indonesia, may offer more lucrative medical procedures, even at times unnecessary ones, in their search for greater profit. Some of the visited health facilities were collaborating with large private employers to provide health care to their employees, and selling them overly complex medical check-ups and laboratory analysis packages. Others provide special services that cater for “modern” demands such as skin and beauty enhancements, especially for women, but increasingly also for men.
For maternal health care, obstetric ultrasound and caesarean section delivery are being promoted more. It is increasingly common in Muhammadiyah and other private services in Indonesia to use ultrasound screening not only for early detection of multiple pregnancy and better gestational age assessment, as recommended by the World Health Organization (WHO),Citation20 but also to provide a visual record of the growth, formation of sexual identity and movements of the fetus.Footnote† Frequent scans have not been shown to have hazardous effects, but they are poorly justified on clinical grounds as they do not enhance perinatal outcomes.Citation20 Women health's organizations ask whether women are making an informed choice,Footnote** a concern raised also in other countries with a high frequency of scans, such as Syria, Viet Nam and China.Citation20–22
In a parallel trend, caesarean section is increasingly recommended in Muhammadiyah facilities as in the rest of the country and the region. A recent audit of Indonesia and three other Southeast Asian countries found that overall caesarean rates were 27%, whereas complications requiring caesarean section are estimated by WHO at 5–15% of deliveries.Citation23 The audit noted that women were generally not fully informed about the increased risk of maternal morbidity in developing countries following elective caesarean section without medical indications. To reduce these risks, as a Lancet study of nine Asian countries suggests, caesarean section should be performed only for medical indications.Citation24 Still, financial considerations are driving these deliveries up because of higher profit margins from the intervention itself, the drugs provided and the longer stay of mother and baby after delivery. The higher fee for an obstetrician (instead of a midwife) also contributes.
Another provider-induced practice has affected Muhammadiyah's delivery of contraceptive services. Direct observation in the visited facilities showed that hormonal injections are being favoured, with little examination or monitoring of prospective users and irrespective of possible side effects. Other possibly more suitable and less costly methods are generally not offered. Muhammadiyah is thus contributing to the disproportionate increase in hormonal injections in overall contraceptive use in Indonesia caused by the ongoing privatization of family planning services and private providers' preference for one- and three-monthly injections as “an ideal way to lock in a flow of payments”.Citation25
Reflections
This case study challenges the assumption that a major, socially-oriented, private sector charitable organization can still focus on ensuring pro-poor services in a context of multiple pressures from increasing privatization. We have seen a shift from MCH-focused primary health care facilities to curative-oriented general hospitals and a move toward more expensive facilities and medical interventions attractive to a more affluent patient population. In turn this is reducing the access of less advantaged groups to health care services, and particularly MCH and contraceptive services. This is at a time when the Indonesian government is also still struggling to improve the quality, accessibility and affordability of public health services and is failing to enhance MCH care and meet MDG5 by reducing maternal mortality and unwanted pregnancies.Citation26
The observed shifts in types of facility, services and patients, and the tendency to promote unnecessary or more expensive services, would need to be confirmed through a more systematic investigation in a context of what is happening with public as well as other private providers. However, we know that other faith-based providers also seem to have commercialized their services, as a recent USAID report on the private health sector in Indonesia concluded that Catholic hospital services are generating operating surpluses, are more expensive than Muhammadiyah's hospital services, and do not tend to attract the poor or near-poor.Citation7
It may therefore be assumed that in spite of the burgeoning private sector, the poor are probably seeing their access to health care reduced, making them more dependent on public facilities. In turn, the public sector, with its extensive network of primary health care, MCH care and family planning services and the lowest hospital tariffs, may have to expand as a provider for the most disadvantaged groups in Indonesia. If so, investments will be needed to strengthen these services and the whole public health system, even if the task is daunting. This challenges the widespread view that the government needs only to focus on the provision of less lucrative, but badly needed, public goods such as epidemiological surveillance and immunization. It also questions the popular assumption that “actual provision of health care [by the government] is of secondary importance, except in areas where there are market failures, i.e. the private sector is unable or unwilling to provide certain services”.Citation7 In a sense, it could be argued that Muhammadiyah's diminishing interest in providing primary health care, MCH and family planning services for the poor does signal a “market failure” that should then be addressed by the government. Given that resources are limited, it also becomes questionable whether the public sector should continue to support the socially-oriented private sector, or de facto subsidize it through social health insurance and other government programmes.
Muhammadiyah does not seem to consider providing better quality (and choices) to those who can pay moreCitation16 as being in contradiction with its social and religious values. From a public policy perspective, however, all groups in society have a right to quality of care, irrespective of their socio-economic class. Development and enforcement of clinical pathways and standards is needed to enhance quality of services and stop the provision of unnecessary and more expensive services and drugs for commercial purposes, including in MCH and family planning provision.
Public perception of the private sector is that it offers better quality than the public sector, gauged on convenience and comfort. Research shows, however, that there is no difference in quality of clinical care — as the same providers practice in both sectors,Citation2Citation8 with multiple practice being a common feature in Indonesia, including at Muhammadiyah. Moreover, the government's oversight of the private sector is minimal in spite of the many unaccountable providers. As the World Bank also recommends,Citation7 improved stewardship by the government is required to regulate the private sector and ensure access to services and quality of care, and to avoid negative consequences for the population, especially the poor.
Finally, public education by independent sources to support informed choices seems urgent in an increasingly competitive health care market. With regard to reproductive health, women accessing maternity and contraceptive services need to know what are and are not essential services, that they should have a choice of contraceptive methods, and be warned that increasingly complex and expensive techniques do not necessarily imply better quality nor are always in their best interests.
If the trends illustrated here are common to other charitable and socially-oriented private providers, serious thinking will need to be devoted to the future of primary care, preventive care and health promotion, including comprehensive reproductive health care. The chronic neglect of these core elements of primary health care in Indonesia may worsen as privatization of the health sector proceeds and profit considerations become more pressing with increased competition.
Acknowledgements
This study was commissioned by the World Bank Jakarta office in 2007 with support from the Dutch government. We gratefully acknowledge useful comments from Claudia Rokx and Puti Marzuki, both from that office. The views expressed here are those of the authors only and do not reflect those of the World Bank or other organizations the authors are or have been associated with.
Notes
* This was later raised to 69% in 2010.Citation6
† Muhammadiyah and Aisyiyah each have their own identity. However, for brevity, only the name of the umbrella organization is used and reference to Aisyiyah is made only when there is a clear distinction.
** For confidentiality reasons, specific informants will not be identified by name and position mentioned only when attribution adds to the argument.
* Most importantly Muhammadiyah's 100th Anniversary Congress and Aisyiyah's 46th Anniversary International Seminar in July 2010.
† Other documents give much higher estimates, probably because they include health hamlet units, not included in the directory, as the main official source of detailed information on individual facilities.
* Muhammadiyah and Asyiyah participate in the Gerakan Sayang Hidup (Pro-Life Movement), an interfaith movement to oppose abortion, although individual health professionals may hold different views.
† Interview with Aisyiyah central-level representatives in Jakarta.
** The main project in this direction was conducted in the mid-2000s to strengthen Muhammadiyah's primary health care facilities in nine provinces, with funding from Pathfinder International (Personal communication, Toha Muhaimin, public health expert, Muhammadiyah member and project facilitator).
* Interview with Natsir Nugroho, Chair, Health and Social Welfare Committee.
† Interviews with Muhammadiyah central-level representatives in Yogyakarta and Jakarta.
** Interviews with Muhammadiyah providers and users in Java and Sumatra, as well as field observations.
* Interview with Natsir Nugroho, Chair, Health and Social Welfare Committee.
* Interestingly, religious preference is being mentioned only as an additional factor in the choice of Muhammadiyah services, with only a small portion of users defining themselves as Muhammadiyah members.
† Interviews with Muhammadiyah and other public and private hospital personnel in Jakarta.
** Including Yayasan Kesehatan Perempuan (Women Health Foundation).
References
- E Azhary. Portret bisnis rumah sakit Indonesia. Economic Review. 218: 2009; 1–8.
- G Chee, M Borowitz, A Barraclough. Private Sector Health Care in Indonesia. 2009; USAID (Health Systems 20/20, PSP-One and Strengthening Pharmaceutical Systems Projects): Jakarta.
- Kementerian Negara Perencanaan Pembangunan Nasional/Badan Perencanaan Pembangunan Nasional (Bappenas). Pembangunan kesehatan dan gizi di Indonesia: overview dan arah ke depan. Background study RPJMN 2010–2014. 2009; Bappenas: Jakarta.
- T Bossert, S Kosen, B Harsono. Hospital autonomy in Indonesia. 1997; Harvard University School of Public Health: Boston.
- Media Data Riset. Private hospital business trend and government hospital condition in Indonesia. 2007; PT Media Data Riset: Jakarta.
- A Ismar. Indonesia opens wider to foreign investment in agriculture and health. At: <www.theaustralian.com.au/business/news/indonesia-opens-wider-to-foreign-investment-in-agriculture-and-health/story-e6frg90x-1225877763099>. Accessed 4 September 2010
- World Bank. Improving Indonesia health outcomes. 2008; World Bank: Jakarta.
- C Rokx, J Giles, E Satriawan. New insights into the provision of health services in Indonesia: A health workforce study. 2010; World Bank: Washington DC.
- C Rokx, G Schieber, P Harimurti. Health financing in Indonesia: A reform road map. 2009; World Bank: Washington DC.
- Sciortino R, Ridarineni N. Muhammadiyah health care provision; a case study. Report to the World Bank, Jakarta office, August 2008. (Unpublished paper).
- Jaaffar Johan. The Calming, Tolerant Voice of Muhammadiyah. New Straits Time. At: <www.nst.com.my/nst/articles/21muha/Article. 10 July 2010>. Accessed 4 October 2010
- Latief H. Health provision for the poor. Islamic aid and the rise of charitable clinics in Indonesia. 2010. (Unpublished paper).
- P van Doorn Harder. Women shaping Islam: Reading the Qur'an in Indonesia. 2006; University of Illinois Press: Urbana.
- M Fuad. Civil society in Indonesia: the potential and limits of Muhammadiyah. Sojourn: Journal of Social Issues in Southeast Asia. 17(2): 2002; 133–163.
- Pajaningsih D. Muhammadiyah dan amal usaha Muhammadiyah bidang kesehatan. 2005. (Unpublished paper).
- Majelis Kesehatan dan Kesejahteraan Masyarakat. Profil dan Direktori Rumah Sakit Muhammadiyah-Aisyiyah. 2005; MKKM: Jakarta.
- Pimpinan Pusat Muhammadiyah. Partisipasi Muhammadiyah dalam program percepatan dan peningkatan akses pelayanan medik spesialis di Indonesia. Kerjasama PP Muhammadiyah, Departemen Kesehatan, Departemen Pendidikan Nasional, Majelis Kesehatan dan Kesejahteraan Masyarakat, Majelis Dikti Litbang, Fakultas Kedokteran Muhammadiyah. Unpublished project proposal, 2007.
- Pimpinan Pusat Muhammadiyah & Majelis Kesehatan dan Kesejahteraan Masyarakat. Revitalisasi pelayanan berbasis akar rumput: Tanfiz rakernas MKKM 22–25 Juni 2006. 2006; PPM & MKKM: Jakarta.
- World Bank. Making services work for the poor in Indonesia: focusing on achieving results on the ground. 2006; World Bank: Washington DC.
- A Harris. Consequences of birth policies and practices in post-reform China. Reproductive Health Matters. 15(30): 2007; 114–124.
- H Bashour, R Hafez, A Abdulsalam. Syrian women's perceptions and experiences of ultrasound screening in pregnancy: implications for antenatal policy. Reproductive Health Matters. 13(25): 2005; 147–154.
- T Gammeltoft, HTT Nguyen. The commodification of obstetric ultrasound scanning in Hanoi, Viet Nam. Reproductive Health Matters. 15(29): 2007; 163–171.
- M Festin, M Laopaiboon, P Pattanittum. Caesarean section in four South East Asian countries: reasons for, rates, associated care practices and health outcomes. BMC Pregnancy and Childbirth. 9: 2009; 1–11.
- P Lumbiganon, M Laopaiboon, AM Gülmezoglu. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 375(9713): 2010; 490–499.
- T Hull, H Mosley. Revitalization of family planning in Indonesia. Draft consultancy report. 2008; BKKBN: Jakarta.
- Disparity among regions a challenge for meeting MDGs. Jakarta Post, 17 February 2010.