Abstract
Maternal mortality has been falling significantly in Cambodia since 2005 though it had been stagnant for at least 15 years before that. This paper analyzes the evolution of some major societal and health system factors based on recent national and international reports. The maternal mortality ratio fell from 472 per 100,000 live births in 2000–2005 to 206 in 2006–2010. Background factors have included peace and stability, economic growth and poverty reduction, improved primary education, especially for girls, improved roads, improved access to information on health and health services via TV, radio and cellphones, and increased ability to communicate with and within the health system. Specific health system improvements include a rapid increase in facility-based births and skilled birth attendance, notably investment in midwifery training and numbers of midwives providing antenatal care and deliveries within an expanding primary health care network, a monetary incentive for facility-based midwives for every live birth conducted, and an expanding system of health equity funds, making health care free of cost for poor people. Several major challenges remain, including post-partum care, family planning, prevention and treatment of breast and cervical cancer, and addressing sexual violence against women, which need the same priority attention as maternity care.
Résumé
La mortalité maternelle a sensiblement diminué au Cambodge depuis 2005, même si elle avait auparavant stagné pendant au moins 15 ans. L'article analyse l'évolution de facteurs majeurs dans la société et le système de santé, en se fondant sur de récents rapports nationaux et internationaux. Le taux de mortalité maternelle a reculé de 472 pour 100 000 naissances vivantes en 2000–2005 à 206 en 2006–2010. Les facteurs d'ordre général comprennent la paix et la stabilité, la croissance économique et la réduction de la pauvreté, le renforcement de l'enseignement primaire, en particulier pour les filles, l'amélioration des routes, l'accès élargi aux informations sur la santé et les services de santé avec la télévision, la radio et les téléphones portables, et une capacité accrue à communiquer avec et dans le système de santé. Les progrès propres au système de santé incluent une hausse rapide des naissances en institution et de l'assistance qualifiée à l'accouchement, avec des investissements dans la formation des sages-femmes et l'augmentation du nombre de sages-femmes assurant des soins prénatals et des accouchements dans un réseau en expansion de soins de santé primaires, des primes financières pour les sages-femmes dans les maternités pour chaque naissance vivante assistée, et un fonds élargi de financement de la santé garantissant la gratuité des soins pour les pauvres. Il reste à relever plusieurs défis majeurs, notamment les soins du postpartum, la planification familiale, la prévention et le traitement des cancers du sein et du col de l'utérus, et la lutte contre la violence sexuelle faite aux femmes, qui requièrent la même attention prioritaire que la maternité.
Resumen
La mortalidad materna en Camboya ha ido disminuyendo considerablemente desde 2005, aunque antes de eso permaneció estancada durante por lo menos 15 años. En este artículo se analiza la evolución en algunos factores importantes de la sociedad y del sistema de salud a raíz de recientes informes nacionales e internacionales. La razón de mortalidad materna bajó de 472 por cada 100,000 nacidos vivos entre 2000 y 2005, a 206 entre 2006 y 2010. Entre los factores antecedentes figuran paz y estabilidad, crecimiento económico y disminución de la pobreza, mejor enseñanza primaria, especialmente para las niñas, mejores carreteras, mejor acceso a información sobre la salud y servicios de salud por televisión, radio y teléfonos móviles y mayor capacidad para comunicarse con el sistema de salud y dentro de éste. Las mejoras específicas al sistema de salud son: un rápido aumento en el número de partos institucionales y con atención calificada, particularmente inversión en la capacitación de parteras y el número de éstas que ofrecen atención antenatal y durante el parto en una red de atención primaria en expansión, incentivo monetario para las parteras en las unidades de salud por cada bebé nacido vivo, y un sistema en expansión de fondos de equidad en salud, que ofrece servicios de salud sin costo alguno para las personas pobres. Aún falta encarar varios retos importantes –tales como atención posparto, planificación familiar, prevención y tratamiento del cáncer de mama y cáncer cervical, y abordaje de la violencia sexual contra las mujeres– a los cuales se les debe prestar la misma atención prioritaria que a la atención materna.
Twenty-five years after the launch of the Safe Motherhood Initiative, recent global estimates of maternal mortality ratios (MMR) are finally showing a decline in many countries.Citation1 To understand why, it is important to analyze the ingredients in individual success stories; this has been done to date for countries such as Bolivia, Egypt, Honduras, Hunan in China, Jamaica,Citation2 Malaysia and Sri Lanka,Citation3 Tamil Nadu in India,Citation4 and Nepal.Citation5 Now, systematic efforts to reduce maternal deaths finally appear to be bearing fruit in a measurable way and rapidly changing the centuries-long birthing tradition in Cambodia. In only ten years, a country with mainly home births has changed to having most births in government facilities.
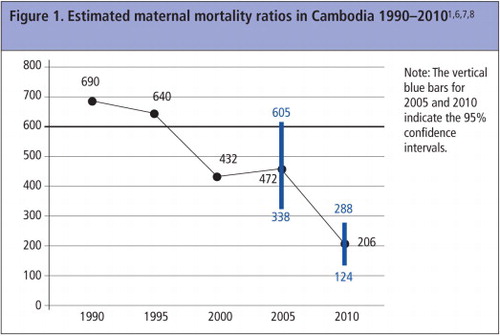
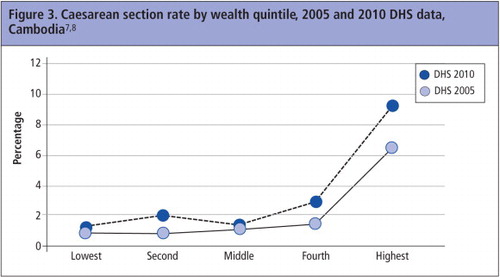
Vital registration of births and deaths is incomplete in Cambodia. National systems for detecting and notifying maternal deaths still only report at best 30% of estimated total deaths (Dr Lo Veasnakiry, Director, Department of Planning and Health Information, Ministry of Health, Personal communication, January 2012). National surveys, Demographic & Health Surveys (DHS) and censuses, as well as global estimates, have for the years 1990–2008 all indicated a MMR stagnant around 432 maternal deaths per 100,000 live births in the 2000 DHS for the six years preceding the survey and 472 in the 2005 DHS for the six years prior to that survey (95% CI 338–605).Citation6,7 During the last five to ten years, much effort has been made to improve maternal survival, however. The 2010 DHS showed a decline to 206 per 100,000 live births (95% CI 124–288), for the period 2004–2010.Citation8 (). Three other recent global estimates have reached a similar conclusion.Citation1,9,10 This reduction means it may be possible for Cambodia to achieve the MDG5 75% reduction target of 140/100,000 live births by 2015. Limited data exist on the main causes of maternal death, but according to an analysis of all maternal deaths reported by the national surveillance system in 2010, haemorrhage, particularly post-partum, was found to be the biggest single cause of death, followed by eclampsia (Prof Tung Rathavy, Director of National Reproductive Health Programme, Personal communication, January 2012) (). Further breakdown of data on other direct causes (21%) were not available.
This article reviews the factors behind the decline in the maternal mortality ratio in Cambodia, within and outside the health system, and discusses areas that require improvement.
Methods
The analysis builds on national reports, local studies and data from the national Health Management Information System,Citation11 Demographic & Health Surveys for 2000, 2005 and 2010,Citation6–8 and information from the National Reproductive Health Programme. A literature search gave very limited additional information as few original papers focusing on maternal health in Cambodia have been published.
Data from the public health system have for many years been collected by the Department of Planning and Health Information, Ministry of Health, and maternal health care data have also been collected by the National Reproductive Health Programme. Most of the data are available through published annual reports or, alternatively, presented at Joint Annual Performance Reviews. Since 2011, all routine information available at the Ministry of Health through the Health Management Information System (HMIS) is available to health staff at a website in Khmer and English, with annual statistics publicly available.Citation11 This website is continuously updated with monthly reports from all government health facilities and was accessed in January 2012 for some of the data presented here. Key unpublished information that was provided or corroborated by Prof Rathavy, Director of the National Reproductive Health Programme, is indicated as a personal communication.
Cambodia is a mainly Buddhist country and gained national independence from France in 1953. The population was 13 million in 2008.Citation12 The following major changes of the last decades outside and inside the health system, relevant to maternal health, have been documented.
Non-health system changes
General development
Stability and peace are fundamental for development. In 1975–79, Cambodia suffered a period of genocide, societal breakdown and vast infrastructural destruction under the Khmer Rouge, and in January 1979, was a land in ruins. Around two million people had perished. Societal reconstruction started at a very basic level in 1979, with efforts marred by severe poverty, continuing warfare in pockets of the country, and the fact that many Cambodians had spent years in refugee camps. Only in 1993 was the current regime accepted by the United Nations as the legitimate representative of the country, after elections had been held. The country has had peace since 1997, and development efforts by governmental and national and international development partners have become systematic.Citation13
Poverty reduction is ongoing. Cambodia is still a low-income country, with a gross domestic product of US$750 per capita. Economic growth was strong over the ten years prior to the global economic crisis of 2009, with annual growth at around 8%. For 2011, 6% economic growth has been predicted. Improved agricultural practices and exports, a growing manufacturing industry, tourism and construction are currently the main drivers of growth. While the poverty rate (per cent living on less than US$1.25/day) has declined from 47% in 1994 to 31% in 2007, it remains high,Citation14 and more common in rural than in urban areas, though significant improvements can be seen in rural areas too. The gap between the poorest and the wealthiest quintiles has been increasing in recent years, however.Citation13,14
Major roads have been hugely improved since 2000; all are now tarred and mainly passable year round. Country roads are still mainly dirt roads, but a vast programme of bridge building has greatly facilitated access to health care. In 2005, about 15% of the rural population lived more than 5km from a year-round accessible road, compared to 20% in 2002. In 2005, about 11% of the rural population needed to travel for more than 30 minutes by motorbike to reach the nearest year-round road.Citation15 The registration of new vehicles, motorbikes and cars, has increased significantly.Citation16 In 2010, 57% of families possessed a motorbike, compared to 38% in 2005.Citation6–8
Communications
Telecommunications were dominated by radio in the 1980s and 90s. In recent years, cellphone coverage has increased rapidly, and today most of the country has good phone coverage, with cellphones becoming ubiquitous throughout the country, rising from 8% of households in 2005 to 58% in 2010.Citation17
General access to an increasing number of communications media – radio, TV, DVD, phone – have helped to expose remote and rural populations as well as urban ones to more and better information on health-related topics and new ways of doing things. Health professionals such as doctors, midwives and nurses, the Ministry of Health, hospitals, health centres and preventive care, all of which were all unfamiliar, have become more familiar to people. Media have been used a lot to communicate health messages in the last 5–10 years; there is no longer a reliance only on one-to-one communication through staff at health centres, village health support groups and volunteers, or community-based contraceptive distributors. Moreover, health staff too have increased access to knowledge and information, thanks to new communications channels.Citation18
Education and political priorities
Education is expanding fast. During the Khmer Rouge years, practically all education was discontinued and the country lost most of its people with higher education due to massacres, starvation, disease and out-migration. Only 45 doctors were thought to have survived the Pol Pot regime in-country. Huge educational efforts starting in 1980 have gradually been paying off since the 1990s, with great improvements in literacy after 2001 and narrowing of the gender gap in primary education. For example, adult literacy among men over 15 years of age was 85% in 2008, and among women 71%, as compared to 79% and 57% in 1998, respectively.Citation12
National political priorities, to a large extent, are focused on reaching the MDGs. This is true both in the overall National Strategic Development Plan up to 2009, recently updated for 2009–2015, and in the current Health Sector Plan (2008–2015).Citation13 There have been special investments in maternal health in the health sector since 2007, and the First Lady, originally a nurse-midwife, in 2011 became a national champion for maternal health.
Fertility
Average age at marriage has risen by about one year from 1998 to 2008, to 23.3 for women and 25.6 for men.Citation12 Virginity among women is highly valued, and premarital sex among women is fairly uncommon. The proportion of teenagers who gave birth in 2007–2010 was small, only 5% of young women aged 15–19 years, while 10% of 18-year-olds gave birth. These figures do not appear to be rising.Citation8
Fertility has been falling in Cambodia since the post-Pol Pot baby boom in the 1980s. The 2010 DHS found a total fertility rate of 3.0, a decline of one child per woman from 2000, with a rate of 2.2 in urban areas and 3.3 in rural areas ().Citation8 With the size of newborn cohorts no longer increasing, Cambodia's population has been moving since year 2000 from a young to an intermediate age population.Citation12 The dependency ratio is also falling, and Cambodia is in the beginning of its demographic bonus period. This means that in the coming 40 years Cambodians aged 15–64 will be proportionately caring for fewer children and older people, leaving more room for national development and education.
Changes within the health system
Main actors in reproductive health
The health system has evolved rapidly, and still faces challenges. In 1979, there was a huge lack of human resources in all sectors. Immediate efforts were initiated to train and deploy additional nurses, midwives and doctors, to rehabilitate infrastructure, and develop public health-oriented programmes in priority areas. Many development partners supported the government in these efforts. Training also took place in refugee camps, mainly on the Thai border, some of which remained functional into the 1990s. Gradually, this post-emergency effort transitioned into a regular health system strategy, including a human resources strategy, with the government in the lead, and with the support of a multitude of partner organizations.Citation13 The latter have included two large national NGOs, the Reproductive Health Association of Cambodia and Reproductive and Child Health Alliance, as well as UNICEF, UNFPA, WHO, and University Research Co, LLC.Citation19
Today, the health system is quite pluralistic, with a large, mainly unregulated private sector – formal and non-formal – and a fine-meshed network of public facilities. The private for-profit sector largely consists of public providers who are also seeing patients privatelyCitation20 and a quite small, purely private sector. The main exceptions are found in the non-profit sector: the large Kantha Bopha hospital – which provides free delivery services in the city of Siem Reap – and the 16 clinics of the Reproductive Health Association of Cambodia, which provide antenatal and post-natal care, but not delivery services. Their clinics, based in cities and towns, provide reproductive health care for approximately 500,000 patients per year, subsidized by donors, mainly USAID. Marie Stopes clinics provide family planning services and consultations for sexually transmitted infections, and Population Services International support quality improvement of reproductive health care in many private clinics. Pregnant women prefer the government system, the NGOs or the Kantha Bopha hospital for pregnancy care as well as family planning. This is not always the case for non-reproductive health-related conditions, where private care, qualified or unqualified, is often sought.Citation8
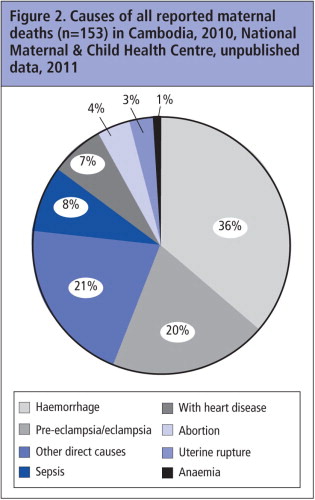
The public sector has 80 hospitals in three tiers – the highest two tiers of which can provide caesarean sections – and 1,008 health centres that each cover a population of 8–10,000 inhabitants. The national caesarean section rate was only 1% in 2005 and still low at 2% in 2010, reflecting how hospital care and referral are still under-utilised, in spite of increasing patient streams to hospitals.Citation11 shows some rise in all quintiles though greatest in the highest quintile.
As regards the overall effectiveness of the Cambodian public health sector, financing issues, budgeting, quality of care, pre-service training and human resources issues are examples of the remaining challenges that significantly influence maternity and family planning care. Another is the need to sufficiently remunerate government health workers, so as to lower the need to work outside government facilities and reduce absenteeism.Citation20
Maternity care
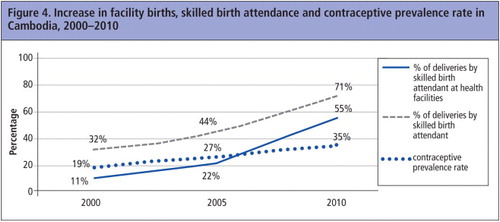
The birthing pattern has changed dramatically in the past decade. In 2000, the most common place to give birth was at home, and only 11% of births took place in government facilities. In 2010, 55% of women gave birth in facilities with a skilled birth attendant.Citation8 The percentage of births in public facilities has continued to rise, and in 2011 had risen to 61% of all estimated births. Of all births at public health facilities, 69% took place in health centres and 31% in hospitals. This rise is also significant at hospital level, and more women with complications are reaching hospital level.Citation11
In 2010, skilled birth attendance in a facility (public, private for-profit or non-profit) accounted for 55% of all births, and home deliveries with a midwife added 16%, for a total of 71% of all estimated deliveries with a skilled attendant.Citation8
Several health system factors have contributed to the rapid rise in facility-based births, including the availability of health centres staffed with midwives and providing antenatal care. Financial barriers have been reduced and availability of midwives has been increased through three financial interventions. Firstly, the growing availability of no-cost health care for poor people, through health equity funds, has made birthing care in public facilities much more widely available. Different systems of no-cost health care for families pre-identified as poor are thus today covering large parts of the country; currently 58 out of 77 operational districts are covered by health equity funds. The government and several major donors, in cooperation, reimburse the facilities for the services provided free to poor women and patients. Transport and food for caretakers who stay with the person who is hospitalized are also part of the health equity fund schemes.Citation21
Secondly, a few partner organizations provide vouchers for pregnant women, and these guarantee free maternity care for any woman attending a government health centre, while also giving financial remuneration to the facility if the facility provides a package of services (four antenatal visits, facility delivery and one post-partum visit). Thirdly, the government in 2007 launched an incentive scheme, the “live-birth incentive”, for health centres and hospitals; US$15 is given to the health centre and US$10 to the hospital for every live birth. These combined income streams make staff very motivated to provide good birthing care around the clock.Citation21,22 It is now common for a health centre midwife to give her cellphone number to a pregnant woman during antenatal care, asking her to call when labour starts, to make sure that the midwife can be at the health centre when the woman arrives. At the same time, the government has banned births by traditional birth attendants and strongly discourages midwives attending home births.
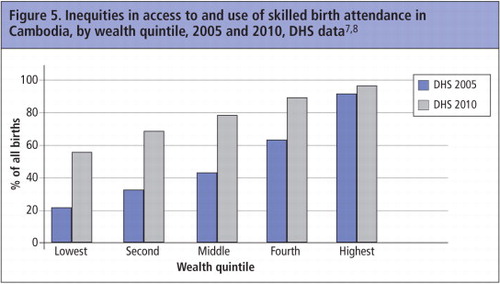
The rapid rise in facility births has changed the panorama of birthing care in Cambodia. It has become the norm for many communities to rely on health centres for antenatal and birthing care as well as post-partum and newborn care. With this change also came a change in traditional practices. A significant caseload of birthing women are now available for pre-service training of midwives. The increase in facility births has benefited women of all wealth quintiles, except the already privileged, for whom coverage was very high already ().
Antenatal care coverage has also increased greatly between 2000 and 2010. In 2000, 38% of all pregnant women had any antenatal care, in 2010, 89% had at least one antenatal care visit, and 59% of women had four or more antenatal care visits.Citation7–9
Strengthening midwifery
Pre-service training of primary and secondary midwives has been prioritized since 2000. Primary midwives have around one year of training only, acquired through a variety of programmes; secondary midwives have three years of direct-entry midwifery training. The Ministry of Health in its Joint Annual Performance Review for 2011 reported that 3,678 midwives are currently employed by the government, that all health centres have at least one primary midwife and that 51% of health centres have a secondary midwife (Prof Tung Rathavy, Director of National Reproductive Health Programme, Personal communication, March 2011). In-service training of midwives is also receiving much attention, and many partner organizations are involved in local efforts.
The regular coordination meetings for health centre midwives are worth mentioning. Health centres in Cambodia are supervised by provincial or operational district health authorities, but have until recently received little direct supervision or support from hospital staff. This shortfall is now being addressed by quarterly, full-day meetings for health centre midwives, key hospital staff and province and district health authorities to create dialogue on recent complicated or referral cases, and give focused training in key areas of obstetric and newborn care. Where they take place, they appear to improve quality of maternity care and family planning services, and the quality and frequency of obstetric referrals. A recent review in 11 USAID-supported provinces (out of 24 provinces) showed that all operational districts in these 11 provinces held such meetings regularly for updates, training and communication (J Liljestrand, unpublished data).
Emergency obstetric and newborn care, and referrals
In 2008, an assessment of emergency obstetric and newborn care revealed that while 25 of the country's hospitals provided comprehensive emergency obstetric and newborn care, out of the 37 needed to fulfill international targets, only 19 out of the 106–110 facilities needed to meet targets for basic emergency obstetric and newborn care actually provided it.Citation23 The same assessment estimated that 73% of the population could reach an emergency obstetric facility within one hour, and that 82% lived within 50 km of one. It was also estimated that 88% of the population could reach a health centre within one hour, and 97% within two hours, while about 96% of the population were estimated to live within 50 km of a health centre.Citation23 The assessment was followed up by a detailed plan for improvement and upgrading of emergency obstetric and newborn care, to be completed in 2015. The plan addresses infrastructural needs as well as human resources, equipment, drugs and referral systems.
Systems for emergency obstetric and newborn referrals are still weak. Public health authorities are working with local NGOs and villages to establish emergency referral schemes from home to health facilities (M Ahmadzai, MCH Specialist, UNICEF, and V Chivorn, Deputy Director, Reproductive Health Association of Cambodia, Personal communication, March 2012), including the contracting of local vehicle owners. Ambulance services from health centres to hospitals are gradually being improved. In 2010, 2.2 % of all health centre births had an emergency referral during delivery.Citation11
Family planning
While the contraceptive prevalence rate has been rising, from 19% using a modern method among married/cohabiting women in 2000 to 35% in 2010, family planning is still lagging behind national targets.Citation11 The national target set at the International Conference on Population and Development in 1994, 55% modern method use among married couples in 2015, will probably not be reached, nor will the MDG target for 2015 of 60% modern method use among married couples.Citation24 The contraceptive method mix consists primarily of condoms, pills and injectables, accounting for 83% of modern method use, while intrauterine devices, implants and surgical contraception make up only 17%.Citation8 While the national commitment to maternal health is strong, this is less so in the area of family planning, where pro-natalist sentiment is often encountered among decision-makers, and usually also a failure to connect maternal health and family planning.Citation25
Abortion
In Cambodia, abortion before 12 weeks of pregnancy is legal at the request of the woman, according to a law passed in 1997. Actual access to safe abortion in public facilities remained limited for a long time, however, being mainly available through private providers. Access has improved since 2005, thanks to increased training of doctors and midwives in the public and private sectors. The training has been carried out by the National Reproductive Health Programme and the NGO Options, in collaboration. More women now have access to safe abortion, more abortions and post-abortion care are safe, and more medical abortions are carried out.Citation26 The proportion of women with repeat abortion has fallen from 8% to 5% from 2005 to 2010, with the increase in contraceptive usage.Citation8 Medical abortion drugs were registered for abortion in 2010, and medical abortion is rapidly increasing.Citation26
Unsafe abortion remains a cause of maternal death, either because of unavailability of safe abortion, lack of knowledge of the legality of abortion among women and providers, or due to late decisions to seek abortion and the fact that government hospitals often do not provide later abortions. A significant drop in abortion-related deaths occurred between 2005 and 2009, however. In 2005, it was estimated that deaths due to unsafe abortion occurred in 10% of Cambodian hospitals and in 1% of health centres providing post-abortion care. In 2009, reports of deaths from unsafe abortion had dropped markedly, and only 1% of the nation's hospitals and 1% of health centres providing post-abortion care reported a death from complications of an unsafe abortion.Citation26
Maternal death reviews and maternal death reporting
The first efforts to audit maternal deaths systematically started in the 1990s, and these efforts were formalized into a national programme in 2004. Almost all known maternal deaths (20–30% of the total estimated maternal deaths) are now investigated through visits to the home of the deceased woman and the facilities that provided care. The information is analyzed at provincial level meetings, and conclusions and actions for improvement of the system are agreed, based on lessons learned. The extent and type of follow-up to implement action varies a lot, however, which we learned from work in five provinces between 2009 and 2012.
Two births happening in rapid succession, Ssar Sadam Health Centre, Siem Reap province, Cambodia, September 2010
Although it has been mandatory to report all maternal deaths to the Ministry of Health since 2009, based on the MMR of 206/100,000 and birth estimates in census data, only 20–30% of maternal deaths are still being reported.Citation27 A combination of community factors (death at home or during transport) and health system factors (facility failed to report a death as maternal) appear to be the main reasons.Citation28
Guidelines and training for maternal and newborn care
Standard treatment guidelines for obstetric care and policies for safe motherhood were developed and published in 2000.Citation29 A newer set of safe motherhood protocols for health centres were published in 2010, and corresponding hospital guidelines are in the pipeline at this writing, prepared by the National Reproductive Health Programme and major partners. All midwives and all doctors working with obstetric care are being trained in life-saving skills, and since 2010 this training is being carried out nationally through shorter training courses at local level, and by coaching and on-the-job training. Treatment of pre-eclampsia and eclampsia, post-partum haemorrhage and newborn asphyxia are being supported by coaching, job aids and monitoring. Importantly, both the management of eclampsia/pre-eclampsia and newborn asphyxia have recently been upgraded to evidence-based programmes based on international guidelines. Assisted deliveries with vacuum extraction and magnesium sulfate treatment for severe pre-eclampsia and eclampsia have both now been delegated also to midwives at health centres, if trained on these methods, making access to these life-saving interventions more available.Citation30
Uterine rupture and obstructed labour account for a minor proportion of maternal deaths in Cambodia today, and vesico-vaginal fistulae are also relatively rare. It thus appears that access to hospital care within a few hours of the advent of an obstetric emergency is fairly high, even though the quality of care may need further improvement.
The need for continuing improvement
The data show that the maternal mortality ratio is falling in Cambodia, and all the factors described in this paper are likely to have contributed to this, even if their relative importance cannot be ascertained. It is to be expected that the quality of maternity care may be lagging, given such rapid expansion in use of services. Giving birth in a health care facility will not automatically lead to better maternity care if the attending staff are not sufficiently skilled. A health centre that previously used to see 5–10 deliveries per month and is now seeing 35 deliveries may lack sufficient floor space, beds, safe water, sewerage, instruments and commodities, on top of the need for increased staffing. Similar constraints due to expansion are seen in hospitals. Infection control may become an issue in facilities that become crowded as well. Efforts by all stakeholders at all levels are therefore critical, to ensure that the quality of care is steadily being improved.
Although attempts to improve emergency referrals for obstetric care are being implemented all over the country, these have been mostly uncoordinated, and limited in scope and impact. Systematic referrals of non-emergency, outpatient cases requiring assessment at higher levels, notably from antenatal care, have also not been well developed. New effort is currently being put into both these areas.
The provision of family planning has improved only slowly (), leaving many pregnancies unwanted, often among grand multiparous women.Citation8 There is also a need for more innovative approaches to the treatment of post-partum haemorrhage. The majority of deliveries take place at health centres, which are often 1–3 hours from hospitals that can perform major surgery. With post-partum haemorrhage the major cause of death, appropriate measures for health centre midwives to prevent and treat severe bleeding are essential for improved maternal survival. Oxytocin is generally available from health centres up, and active management of third stage of labour is improving rapidly. Currently, the only “second-line treatment” available at health centre level is aorta compression (no balloon tamponade or anti-shock garment). Lastly, vital registration of births and deaths in Cambodia is only slowly improving, while as regards maternal death audits, the National Reproductive Health Programme is currently revising the strategy.
Post-partum and post-natal care are still lagging far behind, but progress can be expected in the next five years if a concerted effort is made. Of concern is that newborn mortality has not fallen significantly during the last five years. Focused efforts are needed to make normal birthing care better, and also care of low birthweight and sick newborns. Lessons from successful experiences increasing coverage of antenatal care and delivery services should be applied to post-partum and post-natal care for mothers and newborns, particularly in the first days, first week and month post-delivery.
Compared to many other countries, access to public health facilities is relatively good in Cambodia. A structural issue of major importance is the effectiveness of the health sector overall. Out-of-pocket payments account for a large share of health sector financing. Donors make significant contributions to the health system, but user fees, both formal and informal, are still often significant.Citation31 While discussion of these issues goes beyond the scope of this paper, they will certainly continue to influence maternal health care.
In spite of its poverty, Cambodia has made some major strides in maternal mortality reduction, mainly through increased health centre births assisted by trained midwives, a more liberal abortion law, a decline in fertility, and eliminating financial barriers to maternity care for poor women. Focused efforts on maternal survival are showing success when the key ingredients are in place, but they do not automatically transmit to other areas of sexual and reproductive health. Several major challenges remain, which represent a continuing challenge for Cambodia that the country is well-placed to take on in due course. They include post-partum care, family planning, prevention and treatment of breast and cervical cancer, and addressing sexual violence against women, which need the same priority attention as maternity care.
Acknowledgements
Professor Tung Rathavy, Director of the National Reproductive Health Programme, gave invaluable input to this manuscript, sincere thanks to her. The secondary analysis of DHS 2011 data by wealth quintiles ( and ) was done by Dr Hiromi Obara, WHO, Manila. This study was funded by the US Agency for International Development (USAID) under Better Health Services project, Cooperative Agreement No. 442-A-00-09-00007-00. The findings of this study are the sole responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
References
- World Health Organization. Trends in maternal mortality: 1990–2008. Estimates developed by WHO, UNICEF, UNFPA and the World Bank. 2010; Geneva: WHO.
- M Koblinsky. Reducing maternal mortality. Learning from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica and Zimbabwe. 2003; World Bank: Washington, DC.
- I Pathmanathan, J Liljestrand, JM Martins. Investing in maternal health. Learning from Malaysia and Sri Lanka. 2003; World Bank: Washington, DC.
- P Padmanaban, PS Raman, DV Mavalankar. Innovations and challenges in reducing maternal mortality in Tamil Nadu, India. Journal of Health, Population and Nutrition. 27(2): 2009; 202–219.
- DS Malla, K Ghiri, C Kharki. Achieving Millennium Development Goals 4 and 5 in Nepal. BJOG. 118(Suppl. 2): 2011; 60–68.
- National Institute of Statistics, Directorate General for Health (Cambodia), and ORC Macro. Cambodia Demographic & Health Survey 2000. 2001; National Institute of Statistics, Directorate General for Health, and ICF Macro: Phnom Penh, Calverton, MD.
- National Institute of Public Health, National Institute of Statistics (Cambodia) and ORC Macro. Cambodia Demographic & Health Survey 2005. 2006; National Institute of Public Health, National Institute of Statistics, and ORC Macro: Phnom Penh, Calverton, MD.
- National Institute of Statistics, Directorate General for Health, and ICF Macro. Cambodia Demographic & Health Survey 2010. 2011; National Institute of Statistics, Directorate General for Health, and ICF Macro: Phnom Penh, Calverton, MD.
- MC Hogan, KJ Foreman, M Naghavi. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 375(9726): 2010; 1609–1623.
- R Lozano, H Wang, KJ Foreman. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet. 378(9797): 2011; 1139–1165.
- Ministry of Health. MIS-Annual Health Statistics 2011. At: www.hiscambodia.org. 17 April 2012.
- National Institute of Statistics, Ministry of Planning. General Population Census of Cambodia 2008. 2009; NIS: Phnom Penh.
- Kingdom of Cambodia. UN Development Assistance Framework 2011–2015. Common Country Assessment 2009. 2010; UN in Cambodia.
- World Bank. Cambodia and the World Bank. Cambodia country overview. At: www.worldbank.org/en/country/cambodia. Accessed 12 January 2012.
- Map S. Infrastructure development in Cambodia. In: International infrastructure development in East Asia – towards balanced regional development and integration. In: Kumar N, editor. Eria Research Project Report 2007, No 2. Economic Research Institute for ASEAN and East Asia, Jakarta. At: www.eria.org/research. Accessed 12 January 2012.
- ASEAN Statistical Yearbook, 2008. 2009; ASEAN: Jakarta.
- International Communication Union. At: www.itu.int/ITU-D/ict/statistics. Accessed 28 March 2012.
- BBC World Service Trust. Cambodia Sentinel Survey 2008. Media consumption (radio, television and mobile phone) and HIV/AIDS information in the media. 2008; Ministry of Health: Phnom Penh.
- USAID. Cambodia Global Health Initiative Strategy. Washington DC. 9 September 2011. At: www.ghi.gov/documents/organization/175129.pdf. Accessed 23 April 2012.
- B Meesen, M Bigdeli, K Chheng. Composition of pluralistic health systems: how much can we learn from household surveys? An exploration in Cambodia. Health Policy and Planning. 26: 2011; 130–144.
- T Jordanwood, M Van der Pelt, C Grundmann. Health equity funds implemented by URC and supported by USAID. H Jalililan, V Sen. Improving Health Sector Performance. Institutions, motivations and incentives. The Cambodia Dialogue. 2011; ISEAS Publishing: Singapore, 387–418.
- P Ir, D Horemans, N Souk. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural health districts in Cambodia. BMC Pregnancy and Childbirth. 10: 2010; 1.
- National Emergency Obstetric and Newborn Care Assessment in Cambodia. 2009; National Institute of Public Health: Phnom Penh.
- Royal Government of Cambodia. Achieving Cambodia's Millennium Development Goals. 2010 update. 2010; Ministry of Planning: Phnom Penh.
- Chivorn V, Sokrin K, Ouk Vong V, et al. Family planning in Cambodia – is it a public health priority? (Submitted)
- T Fetters, S Barnett, T Chourn. Abortion in Cambodia 2005 and 2010. 2011; Ipas: Chapel Hill, NC.
- Ministry of Health. Fast Track Initiative for reducing maternal and newborn mortality 2010–2015. Phnom Penh: MoH.
- Mak S, Krasovec K, Men RC, et al. Maternal death reporting in a Cambodian operational district. (In manuscript)
- Ministry of Health. Safe Motherhood Clinical Management Protocols. 2000; Referral Hospital. (Khmer) MoH.
- Ministry of Health. National Reproductive Health Programme. Safe Motherhood Clinical management protocols: Health Centres. 2010; MoH: Phnom Penh.
- V Tangcharoensathien, W Patcharanarumol, P Ir. Health-financing reforms in southeast Asia: challenges in achieving universal coverage. Lancet. 377(9768): 2011; 863–873.