Abstract
A rights-based approach in HIV service delivery for adults is increasingly taking root in sub-Saharan Africa in the context of greater availability of antiretroviral therapy. Yet there has been comparatively little progress in strengthening a rights-based approach to adolescent HIV services, which we learned during a qualitative study in 2010 among 111 adolescents living with HIV, 21 parents and 38 health providers in three districts in Zambia. Adolescents in the study expressed a range of information and support needs and wanted locally relevant interventions to meet those needs. They wanted greater access to HIV, sexual and reproductive health information, information on how to protect themselves, privacy and confidentiality in service sites, skills training so as to be able to earn money, and better control over disclosure of their HIV status to others. Both health workers and parents acknowledged that information and services needed to be improved to meet those needs far better. This paper provides examples of successful programmes in Zimbabwe, Uganda, Tanzania, Botswana and South Africa and calls for adolescent services to be linked to both paediatric and adult services, peer networks to be established to increase adolescents' ability to collectively voice their concerns and support each other, interventions supporting adolescents' control over self-disclosure, and lastly that adolescent health should become a training specialty in sub-Saharan Africa.
Résumé
L'approche basée sur les droits de la prestation de services en matière de VIH pour les adultes est en train de s'enraciner en Afrique subsaharienne, dans le contexte de la disponibilité accrue du traitement antirétroviral. Pourtant, il y a eu comparativement peu de progrès accomplis pour renforcer cette approche des services en matière de VIH pour adolescents. C'est qu'a révélé une étude qualitative menée en 2010 auprès de 113 adolescents vivant avec le VIH, 21 parents et 38 prestataires de santé dans trois districts en Zambie. Ces adolescents ont exprimé un éventail de besoins en information et soutien et souhaitaient des interventions pertinentes localement pour répondre à ces besoins. Ils voulaient avoir un accès élargi aux informations sur le VIH, la santé sexuelle et génésique, connaître les moyens de se protéger, bénéficier de confidentialité dans les sites de services, se former afin de pouvoir gagner de l'argent et mieux maîtriser la révélation de leur séropositivité aux autres. Les agents de santé et les parents ont reconnu que ces informations et services devaient être améliorés pour satisfaire bien mieux ces besoins. L'article donne des exemples de programmes réussis au Zimbabwe, en Ouganda, en République-Unie de Tanzanie, au Botswana et en Afrique du Sud et recommande de lier les services pour adolescents aux services pédiatriques et pour adultes, de créer des réseaux de pairs pour renforcer la capacité des adolescents à faire entendre collectivement leurs préoccupations et se soutenir mutuellement, de réaliser des interventions favorisant le contrôle des adolescents sur l'autorévélation et enfin de faire de la santé des adolescents une spécialité de la formation en Afrique subsaharienne.
Resumen
Cada vez más se está arraigando en Ãfrica subsahariana el enfoque en la prestación de servicios de VIH para adultos basado en los derechos, en el contexto de mayor disponibilidad de terapia antirretroviral. Sin embargo, se han visto relativamente pocos avances en fortalecer el enfoque basado en los derechos con relación a los servicios de VIH para adolescentes, lo cual averiguamos durante un estudio cualitativo realizado en 2010 entre 113 adolescentes que vivían con VIH, 21 padres y 38 profesionales de la salud de tres distritos de Zambia. Los adolescentes del estudio expresaron una variedad de necesidades de información y apoyo y querían intervenciones pertinentes para la localidad, que atendieran esas necesidades. Querían mayor acceso a información sobre VIH y salud sexual y reproductiva e información sobre cómo protegerse; privacidad y confidencialidad en las unidades de salud; capacitación en habilidades para poder ganar dinero; y mejor control de la revelación de su estado de VIH a otras personas. Tanto los trabajadores de la salud como los padres reconocieron que es necesario mejorar la información y los servicios para atender mucho mejor esas necesidades. En este artículo se exponen ejemplos de programas exitosos en Zimbabue, Uganda, Tanzania, Botsuana y Sudáfrica y se hace un llamado a vincular los servicios para adolescentes con los servicios para niños y adultos; a establecer redes de pares para aumentar la capacidad de los adolescentes para expresar sus inquietudes de manera colectiva y apoyarse unos a otros; a realizar intervenciones que apoyen el control de los adolescentes sobre la autorevelación; y, por último, a que la salud de la adolescencia sea una especialidad de formación en Ãfrica subsahariana.
The HIV epidemic in sub-Saharan Africa is maturing, and with it, the profile of adolescents and other young people living with HIV is evolving.Citation1 In Zambia the number of adolescents living with HIV is on the rise owing to greater availability of antiretroviral therapy, which is enabling vertically infected children to survive into adolescence.Citation2 Adolescents – most of whom are sexually activeCitation3 – account for almost half of new HIV infections in Zambia.Citation4,5 At the end of 2009, there were 80,000 young people aged 10–19 living with HIV in Zambia.Citation6
Thus, adolescents may increasingly be determining the trajectory of the HIV epidemic in southern Africa.Citation7–9 The epidemiological significance of adolescents as a group living with HIV has gained attention in terms of their potential to influence whether the Millennium Development Goals related to HIV and health are achieved or not.Citation8 This distinction has fostered awareness that their needs are different from those of both paediatric and adult populations living with HIV.Citation10–12
In Zambia, as in other sub-Saharan African countries, data on adolescents aged 10–19 living with HIV are often reported within 0–14, 15–19 or 15–24 age groups, making it difficult to accurately determine the extent of their access to HIV services.Citation4,13 Although the current Zambian National AIDS Strategic Framework for 2011–2015 prioritises HIV prevention among young people,Citation14 it lacks specific provisions relating to the care of adolescents and other young people already living with HIV.Citation15 This is particularly relevant in light of recent studies showing that a constellation of factors at the individual and community level is preventing the protection and fulfilment of sexual and reproductive health and rights of all adolescents in Zambia, regardless of their HIV status.Citation3,16,17 At the same time, adolescents living with HIV in Zambia regularly encounter additional social and emotional difficulties due to HIV-related stigma and additional family responsibilities,Citation18 and across southern Africa, they also tend to have poorer treatment outcomes compared to adults.Citation19,20 These facts demand greater attention.
Strengthening health systems to respond to sexual and reproductive health and other social protection needs of adolescents living with HIV is an indispensable strategy towards mitigating the impact of HIV on adolescent health.Citation21,22 In addition, tailoring health services to the needs of adolescents living with HIV is an opportunity to deliver age-appropriate interventions while advancing their right to health.Citation12,21 The UN Convention on the Rights of the Child requires the rights of all children to be respected, protected and fulfilled.Citation23,24 In the context of young people affected by HIV, these rights include the right to health and health services.Citation24,25
A rights-based paradigm led a far greater number of adults living with HIV to demand and eventually access antiretroviral therapy by the late 1990s,Citation26 despite disbelief at the time that this was feasible. Access to treatment was achieved largely through multifaceted advocacy initiatives aimed at mitigating structural barriers to treatment in Brazil and other countries, and finally in southern Africa.Citation26,27 A similar trajectory does not appear to have gained momentum in regard to adolescent services, even while global advocacy for early infant diagnosis contributed to the scale-up of paediatric treatment.Citation28 Consequently, although meeting the needs of all age groups is critical in the continuum of care for people living with HIV,Citation29 the recognition of the special needs of adolescents living with HIV has lagged behind.Citation11,30
Adolescents have often been wrongly perceived as young adults or big children,Citation31,32 which has resulted in their being provided with services designed for adult or paediatric populations.Citation33,34 We may say that there is an underlying gap in health systems' ability to deliver age-appropriate interventions for adolescents generally, not only for those living with HIV,Citation35,36 a problem that has become more evident as increasing numbers of young people both require and demand services.Citation7
In addition to unresponsive health systems, the social and legal environment in sub-Saharan Africa has traditionally curtailed the ability of adolescents to demand and access health services more generally,Citation35,36 as adolescents are often considered to be under the responsibility of adults,Citation36 with limited control of information or decision-making on their HIV status.Citation31 In addition, their access to sexual and reproductive health information is often hindered by cultural norms.Citation31,36
The prospect of adolescents living with HIV expressing their needs and challenging cultural barriers creates an opportunity to overcome some of these challenges. Moreover, the engagement of adolescents living with HIV in articulating their HIV-related service needs could also strengthen their demands for relevant sexual and reproductive health interventions.Citation10,21
A central concept underpinning the ability of adolescents to gain some control and discretion over their own well-being is that of self- and collective efficacy – how much control and influence individuals have over their own circumstances. Adolescents have an evolving capacity to take action to fulfil their right to health.Citation37 Research from Zambia shows that adolescents understand the circumstances that expose them to HIV risk and are adopting safer sexual practices, for example.Citation38 In turn, the potential of adolescents to positively influence the course of the HIV epidemicCitation39 is reinforcing global advocacy to increase their access to HIV treatment, care and other services.Citation9
Yet in most cases, advocacy for these services appears to be driven not by adolescents themselves but by other actors, such as networks of people living with HIV (largely made up of adults), government agencies, and non-governmental and international organisations. In addition, while the concept of reproductive rights as a fundamental aspect of human rights has gained global acceptance,Citation40 current approaches to adolescent health in Zambia and other sub-Saharan African countries continue to focus on adolescents' sexual behaviours and outcomes, with limited emphasis on their sexual and reproductive rights and their capacity to actualise those rights.Citation16,38 In Zambia, despite progress made by the government in strengthening the provision of adolescent-friendly services,Citation41 weak health systems remain a limiting factor towards the fulfilment of adolescents' sexual and reproductive rights.Citation16,31,42
In this discussion paper, we explore how the evolving capacity of adolescents living with HIV is shaping their ability to express their needs and how the health services should respond. We provide quotes from focus group discussions and interviews with young people aged 10–19 and quotes from their parents and health care providers to support our arguments.
Study methodology
The study was conducted between April and December 2010; the main findings are reported elsewhere.Citation31 Part of the study aimed to document the psychosocial and sexual and reproductive health needs of adolescents living with HIV in Zambia, and identify gaps between those needs and currently available services for adolescents. The study was conducted in one rural (Kalomo) and two urban districts (Lusaka and Kitwe) in Zambia, where adolescents make up almost a quarter of the population of 10 million.Citation6 These districts were selected for variation in geographic location, contexts and interventions available. In all three districts, adolescents were accessing clinical HIV services from government HIV clinics and non-clinical support from community centres run by non-governmental organisations which served as our study recruitment sites.
Adolescents willing to participate were consecutively recruited while attending a clinic or centre. Parents and guardians signed consent forms for orally consenting adolescents aged 10–18, while adolescents aged 18–19 signed their own consent forms. All participating adolescents were aware of their HIV status and efforts were made to safeguard confidentiality consistent with recommendations on research among young people.Citation43,44 Inclusion of interviews with parents and health care providers allowed us to triangulate findings.Citation45 Ethical approval was granted by the Biomedical Research Ethics Committee of the University of Zambia.
Semi-structured interviews were conducted with adolescents living with HIV (58) and health care providers (14). The latter included doctors (5), nurses (4), counsellors (2), clinical officers (2) and administrative staff (1). Questions were tailored to younger adolescents (10–14 years), older adolescents (15–19 years) and key informants. The interviews, each lasting 30–40 minutes, were conducted in English or the local languages (Bemba, Lozi and Nyanja), and audio recorded, transcribed and translated into English.
Eight focus group discussions were subsequently held with 53 additional adolescents living with HIV, two with 21 parents (1 urban and 1 rural) and three with 24 health care providers (2 urban and 1 rural). The adolescent groups included two with girls aged 10–14 years, two with girls aged 15–19 years, two with boys and girls aged 10–14 years, and two with boys and girls aged 15–19 years. Moderated, semi-structured discussions using open-ended questions and follow-up probes were conducted, focusing on whether and how health services were meeting the needs of adolescents living with HIV. Discussions were conducted in English or local languages and lasted about 50–60 minutes, and were digitally recorded, transcribed and translated to English, and analysed using NVivo 7 (QSR International), with transcripts coded inductively to identify emerging themesCitation46 and the needs expressed by adolescents.
A sense of rights, entitlement and expectation
In the adolescent interview group, most (46) were living in urban areas, half were male and half female, and about 50% were in a sexual relationship at the time of the study. The sexually active adolescents tended to be older; six of them were married with children of their own. Twenty-eight of them planned to have children in the future. Only two of the sexually active adolescents had not disclosed their HIV status to their sexual partners, mainly for fear that it could end their relationships.
They seemed to embrace the concept of living positively and the rights of young people living with HIV to enjoy a fulfilling sexual life. A majority believed that people living with HIV should be allowed to marry and have children, if they so desired, for example.
“People living with HIV have feelings… [they] are human beings with normal lives, and marriage is a right to everyone, whether HIV positive or not.” (Interview, 19-year-old female, Lusaka)
“We have a right to having a family and have children.” (Focus group discussion, 17-year-old male, Kalomo)
“I do not think that being [HIV] positive should stop you from being in a relationship. Being HIV positive does not make a relationship different; it is just the same as those who are not positive.” (Interview, 17-year-old male, Lusaka)
“Everyone was looking at me in a funny way and whispering, ‘This is the one who is sick, she has AIDS.’ This was very painful for me because I thought that it was my right to disclose to people about my status. I felt that my rights were violated.” (Focus group discussion, 16-year-old female, Lusaka)
Expressing unmet needs
Many saw the health system as weak and not meeting their HIV, sexual and psychosocial needs, fulfilling their right to confidentiality or addressing them as a separate group.
“I have tried to ask them for more information but they did not give me enough. What they told me was not very useful. I would love to have more access to information and life skills. I do not have enough information about family planning, which is my right.” (Interview, 17-year-old female, Lusaka)
“There should be more room so that as others are being privately attended to, those on the waiting line could be together and chatting about how to live positively and all, which could be a motivation.” (Focus group discussion, 16-year-old male, Kitwe)
“They should separate us from old people, and help us with what is needed for us children like SRH [sexual and reproductive health].” (Interview, 16-year-old male, Kalomo)
“The other challenge that our adolescents living with HIV are facing is stigma and discrimination. This vice must be fought so that our adolescents can be free to access services, because sometimes they refuse to go to the hospital for fear of being known. We must deal with this issue when we set up child-friendly services.” (Focus group discussion, parents, Kalomo)
“What I am taught at the clinic is really helpful, but I would really like to learn some more, especially about how I can protect myself. I feel disappointed at times.” (Interview, 14-year-old female, Lusaka)
“I would like to know more about how you can get pregnant and what you can use to protect yourself from getting pregnant.” (Interview, 16-year-old female, Kalomo)
“I want to know if I can have a boyfriend because every time I ask my mum she tells me not to. I would also love to learn about safe sex and safe motherhood.” (Focus group discussion, 14-year-old female, Lusaka)
“One thing that I would really like is being taught life skills because as it is, no one teaches us these things. I would like to learn how to cook, and also tailoring.” (Focus group discussion, 14-year-old female, Lusaka)
“Because I am blind I would really like to learn some skills so that I can sustain myself.” (Interview, 12-year-old male, Kalomo)
Acknowledgement of adolescent needs by health care providers and parents
There was an acknowledgement from both health care providers and parents that adolescents' access to appropriate HIV services was important, in spite of cultural and other barriers, but achieving it would take time.
“We don't have adolescent-friendly services because initially it was assumed that a child born with HIV, for example, was going to die in a few months, so even services were not designed for adolescents, meaning that their access to treatment is a challenging issue.” (Interview, health provider, Lusaka)
“There needs to be a full-time person trained specifically to deal with adolescents.” (Focus group discussion, health provider, Kalomo)
“One of the things we are looking at is having national guidelines that would support sexual reproductive health and rights for adolescents living with HIV.” (Focus group discussion, health provider, Lusaka)
“We feel and believe that it is a right of young people to access these services such as ...sexual and reproductive health, we are talking about issues of contraception, unsafe abortion and safe motherhood. We are talking about empowering them to make informed choices. Basically the services are evolving but that takes time.” (Interview, health provider, Lusaka)
“I think the primary thing is information...and then support groups and making this referral centre… The idea is to have a specialized secondary referral centre for adolescents and paediatrics with clinical, treatment and adherence problems.” (Interview, health provider, Lusaka)
“Most of our adolescents don't have access to information because of tradition – us parents don't like discussing such issues because sexuality is something sensitive... so my view is that we change the perspective of dealing with this as a taboo.” (Focus group discussion, parents, Lusaka)
“We as parents are also to some extent not fully aware of SRH [sexual and reproductive health] information that can help adolescents living with HIV grow up informed, but this is again a problem to do with the non-availability of children's clinics and youth-friendly corners” (Focus group discussion, parents, Kalomo)
Discussion
Acknowledging adolescents' evolving social and legal capacityCitation10,12 and involving them in designing health programmes could strengthen delivery of interventions tailored to their needs.Citation6 As early as 1989, the Convention on the Rights of the Child emphasised the importance of giving children a say in matters that affect them.Citation23 By 1994, the International Conference on Population and Development focused specifically on protecting and promoting adolescents' reproductive health rights.Citation47 More recently, Millennium Development Goal 3 and the Commission on Population and Development (45th session, 2012), have linked the strengthening of young people's sexual and reproductive health and rights to their access to services related to HIV and other sexually transmitted infections.Citation48 What exactly, then, is needed?
First, adding adolescent services, linked to both paediatric and adult services, could be a mechanism for entrenching a rights-based paradigm for adolescent health. Sawyer et alCitation10 argue that the nature of adolescent-friendly services should be informed by adolescents themselves, and we agree. In a Zimbabwean model described by Erukar et al,Citation49 when adolescents were asked to identify characteristics that would, in their view, make services youth-friendly, they rated confidentiality, short waiting time, low cost and friendly staff as the most important characteristics. The least important characteristics included youth-only services, suggesting that adolescents do not necessarily prefer stand-alone youth services, which may be contrary to expectations.Citation49
Defining these characteristics, which could differ depending on the context and the social circumstances of adolescents, should precede implementation of adolescent HIV services. For instance, some adolescents in our study had children of their own; a situation which calls for seamless transition and close linkages between paediatric, adolescent and adult services as well as better integration of sexual and reproductive health with HIV services for older adolescents living with HIV.Citation50 Evidence from other countries shows that physical co-location and the provision of a package of interventions that includes dual protection and a contraceptive method mix within adolescent HIV services could facilitate integration.Citation34,50
Similarly, HIV services need to address livelihood needs of adolescents living with HIV. While vocational and life skills training is commonplace in HIV programmes for adults, this is rare in adolescent services, but could be important for adolescents who, as in our study, were primary carers to their children. In a rare programme in Zimbabwe, adolescents affected by HIV were included within a community-based savings and life skills programme, which apart from empowering them economically, also improved their self-efficacy and self-esteem.Citation51
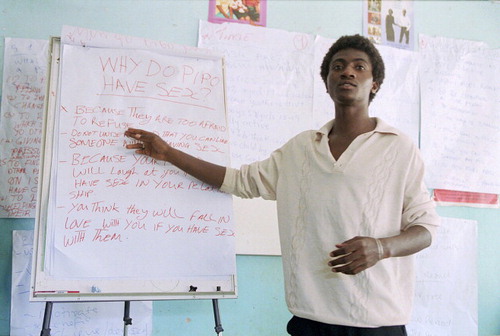
Second, adolescents living with HIV should be supported to establish peer networks of their own, similar to those for adults, as part of adolescent HIV programming. This would increase their ability to collectively voice their concerns and preferences in regard to services, as well as their ability to support each other and overcome stigma. In Uganda, HIV programmes have started engaging peer groups of adolescents to counsel each other, reinforce ART adherence, and sensitize their communities about HIV by sharing their experiences of living with HIV.Citation52 This facilitation of adolescents' collective efficacy needs to be a central pillar of HIV services. Evidence from a recent randomized trial in Tanzania shows that when supported to understand social ecology, citizenship, HIV and broader community health issues, as well as how to make needs assessments and take collective action, adolescents can collectively educate and mobilize their own communities. They can also successfully engage governmental and non-governmental organizations to provide a wide range of services for themselves and their communities.Citation37 HIV programmes should therefore create platforms and opportunities that enable dialogue between young people, their communities and their governments, as they have successfully done for adults living with HIV.Citation53,54 Conversely, policy makers ought to seek and listen to the voices of adolescents living with HIV when formulating policies related to HIV and young people in order to ensure that national policies emphasize HIV prevention among youth, as well as providing appropriate services to those already living with HIV.
Third, there is the issue of disclosure of HIV status, which has been shown to be an important problem for HIV positive adolescents. Adolescents and their families need to have greater control over how and when to disclose their status to others, which requires disclosure skills. Although experience on how to achieve this is limited, evidence from South Africa shows that family-centred approaches that improve disclosure skills of parents living with HIV could be an important methodology to adopt for adolescents.Citation55 Interventions supporting adolescents' self-disclosure should take into account their evolving capacity, self-efficacy and sexual and family relationships.Citation56,57
Achievement of sexual and reproductive health of adolescents living with HIV requires HIV programmes to engage adolescents and their communities in tackling HIV stigma and other cultural barriers preventing adolescents from enjoying a healthy sexual life. In our study, adolescents living with HIV were determined to have healthy sexual relationships, but were often challenged by cultural traditions that prevented them from discussing their sexual relationships with their parents. Strengthening parents' and adolescents' communicative ability regarding sex and relationships could facilitate and positively influence adolescents' sexual behaviour.Citation58,59 Improving comfort with communication about sex, sexuality and relationship may require parents-focused programming to enable them to improve communication with their HIV-infected adolescents, as has been done successfully in Uganda.Citation60
Fourth, there is a need to ensure that health providers are specifically trained on adolescent health. Unlike in most western countries, adolescent health is not a training specialty in sub-Saharan Africa.Citation61 However, competency-based training of health providers on adolescent health has been shown to be effective in Botswana.Citation62 In Uganda, the Ministry of Health has successfully improved adolescent counselling skills of HIV counsellors through a similar competency-based training programme. The hallmark of this initiative, which was implemented in partnership with non-governmental organizations, was the meaningful involvement of primary beneficiaries in identifying their counselling needs, which informed the development of a prototype curriculum and strengthened the ability of service providers to handle adolescent issues.Citation63 In Zimbabwe, training of health providers involved adolescents themselves, who explained their experiences of living with HIV and their psychosocial needs.Citation64
In summary, our findings suggest that health services in Zambia could be transformed to become more adolescent-friendly through a number of approaches, including 1) using participatory approaches to define adolescent services; 2) identifying health care providers who could assume responsibility for care of adolescents and their transition from paediatric to adult services; 3) strengthening health providers' competencies to provide adolescent-friendly services; 4) responding to individual circumstances as well as the wider social context of adolescents living with HIV i.e. in relation to social, economic, stigma and other cultural barriers, and 5) empowering adolescents living with HIV to advocate for themselves and become leading agents of change.
Acknowledgements
We are thankful to the young people, research assistants and adults who participated; Fabian Cataldo, who participated in designing the study protocol; the research advisory group, including the Southern Africa AIDS Trust, among others; and our study funders, the Swedish International Development Cooperation Agency, through the Africa Regional Programme of the International HIV/AIDS Alliance, and the UK Department for International Development, through the Evidence for Action Research Consortium.
References
- R Ferrand, S Lowe, B Whande. Survey of children accessing HIV services in a high prevalence setting: time for adolescents to count?. Bulletin of World Health Organization. 88(6): 2010; 428–434.
- United Nations Children's Fund. Children and AIDS: Fifth Stocktaking Report, 2010. 2010; UNICEF: New York.
- S Siziya, AS Muula, LN Kazembe. Harmful lifestyles' clustering among sexually active in-school adolescents in Zambia. BMC Pediatrics. 8(6): 2008
- Ministry of Health [Zambia] Central Statistical Office [Zambia] and ORC Macro. Zambia HIV/AIDS Service Provision Assessment Survey 2005. 2006; Ministry of Health, Central Statistical Office and ORC Macro: Calverton, MD.
- S Agha, R Van Rossem. Impact of a school-based peer sexual health intervention on normative beliefs, risk perceptions, and sexual behavior of Zambian adolescents. Journal of Adolescent Health. 34(5): 2004; 441–452.
- United Nations Children's Fund. The State of the World's Children 2011. 2011; UNICEF: New York.
- RA Ferrand, EL Corbett, R Wood. AIDS among older children and adolescents in Southern Africa: projecting the time course and magnitude of the epidemic. AIDS. 23(15): 2009; 2039–2046.
- Joint United Nations Programme on HIV/AIDS. We can empower young people to protect themselves from HIV. 2010; UNAIDS: Geneva.
- UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2010. 2010; UNAIDS: Geneva.
- SM Sawyer, RA Afifi, LH Bearinger. Adolescence: a foundation for future health. Lancet. 379(9826): 2012; 1630–1640.
- World Health Organization. Antiretroviral Therapy of HIV Infection in Infants and Children in Resource-limited Settings: Towards Universal Access. 2006; WHO: Geneva.
- WHO. Adolescent Friendly Health Services: An Agenda for Change. 2002; WHO: Geneva.
- M Mahy, JM Garcia-Calleja, KA Marsh. Trends in HIV prevalence among young people in generalised epidemics: implications for monitoring the HIV epidemic. Sexually Transmitted Infections. 88(Suppl.2): 2012; 65–75.
- National AIDS Council [Zambia]. National AIDS Strategic Framework 2011–2015. 2010; National AIDS Council [Zambia]: Lusaka.
- S Kalibala, D Mulenga. Situation Assessment of the HIV Response Among Young People in Zambia. 2011; UNAIDS: Geneva.
- RJ Magnani, AM Karim, LA Weiss. Reproductive health risk and protective factors among youth in Lusaka, Zambia. Journal of Adolescent Health. 30(1): 2002; 76–86.
- L Warenius, KO Pettersson, E Nissen. Vulnerability and sexual and reproductive health among Zambian secondary school students. Culture, Health & Sexuality. 9(5): 2007; 533–544.
- A Menon, C Glazebrook, N Campain. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. Journal of Acquired Immune Deficiency Syndromes. 46(3): 2007; 349–354.
- JB Nachega, M Hislop, H Nguyen. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. Journal of Acquired Immune Deficiency Syndromes. 51(1): 2009; 65–71.
- MD Nglazi, K Kranzer, P Holele. Treatment outcomes in HIV-infected adolescents attending a community-based antiretroviral therapy clinic in South Africa. BMC Infectious Diseases. 12: 2012; 21.
- S Bakeera-Kitaka, N Nabukeera-Barungi, C Nostlinger. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care. 20(4): 2008; 426–433.
- LJ Koenig, SL Pals, S Chandwani. Sexual transmission risk behavior of adolescents with HIV acquired perinatally or through risky behaviors. Journal of Acquired Immune Deficiency Syndromes. 55(3): 2010; 380–390.
- AS McMillan, D Simkiss. The United Nations Convention on the Rights of the Child and HIV/AIDS. Journal of Tropical Pediatrics. 55(2): 2009; 71–72.
- S Gruskin, D Tarantola. Universal access to HIV prevention, treatment and care: assessing the inclusion of human rights in international and national strategic plans. AIDS. 22(Suppl 2): 2008; S123–S132.
- JR Ayres, V Paiva, I Franca Jr. Vulnerability, human rights, and comprehensive health care needs of young people living with HIV/AIDS. American Journal of Public Health. 96(6): 2006; 1001–1006.
- A Berkman, J Garcia, M Munoz-Laboy. A critical analysis of the Brazilian response to HIV/AIDS: lessons learned for controlling and mitigating the epidemic in developing countries. American Journal of Public Health. 95(7): 2005; 1162–1172.
- M Chopra, N Ford. Scaling up health promotion interventions in the era of HIV/AIDS: challenges for a rights based approach. Health Promotion International. 20(4): 2005; 383–390Te.
- R Baryamutuma, F Baingana. Sexual, reproductive health needs and rights of young people with perinatally acquired HIV in Uganda. African Health Sciences. 11(2): 2011; 211–218.
- WHO UNAIDS. Key elements in HIV/AIDS care and support. 2000; WHO, UNAIDS: Geneva.
- WHO. Integrating sexual health interventions into reproductive health services: programme experience from developing countries. 2005; WHO: Geneva.
- I Hodgson, J Ross, C Haamujompa. Living as an adolescent with HIV in Zambia – lived experiences, sexual health and reproductive needs. AIDS Care. 24(10): 2012; 1204–1210.
- WHO. A qualitative review of psychosocial support interventions for young people with HIV. 2009; WHO: Geneva.
- S Gruskin, L Ferguson, J O'Malley. Ensuring sexual and reproductive health for people living with HIV: an overview of key human rights, policy and health systems issues. Reproductive Health Matters. 15(29 Suppl): 2007; 4–26.
- H Birungi, F Obare, JF Mugisha. Preventive service needs of young people perinatally infected with HIV in Uganda. AIDS Care. 21(6): 2009; 725–731.
- A Binagwaho, A Fuller, V Kerry. Adolescents and the right to health: eliminating age-related barriers to HIV/AIDS services in Rwanda. AIDS Care. 24(7): 2012; 936–942.
- GE Siu, S Bakeera-Kitaka, CE Kennedy. HIV serostatus disclosure and lived experiences of adolescents at the Transition Clinic of the Infectious Diseases Clinic in Kampala, Uganda: a qualitative study. AIDS Care. 24(5): 2012; 606–611.
- M Carlson, RT Brennan, F Earls. Enhancing adolescent self-efficacy and collective efficacy through public engagement around HIV/AIDS competence: a multilevel, cluster randomized-controlled trial. Social Science & Medicine. 75(6): 2012; 1078–1087.
- C Michelo, IF Sandoy, K Fylkesnes. Marked HIV prevalence declines in higher educated young people: evidence from population-based surveys (1995–2003) in Zambia. AIDS. 20(7): 2006; 1031–1038.
- N Kayeyi, K Fylkesnes, C Michelo. Decline in HIV prevalence among young women in Zambia: national-level estimates of trends mask geographical and socio-demographic differences. PLoS One. 7(4): 2012; e33652.
- LH Bearinger, RE Sieving, J Ferguson. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 369(9568): 2007; 1220–1231.
- Ministry of Health [Zambia]. Adolescent HIV Care and Treatment: A Training Curriculum for Multidisciplinary Health Care Teams. 2011; MOH [Zambia]: Lusaka.
- P Ferrinho, S Siziya, F Goma. The human resource for health situation in Zambia: deficit and maldistribution. Human Resources for Health. 9(1): 2011; 30.
- Save the Children. So you want to involve children in research?. 2004; Save the Children: Stockholm.
- World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. 2008; WMA: Ferney-Voltaire.
- R Bhopal. Concepts of Epidemiology: Integrating the Ideas, Theories, Principles and Methods of Epidemiology. 2nd ed. 2008; Oxford University Press: Oxford.
- D Silverman. Interpreting Qualitative Data: Methods for Analyzing Talk, Text and Interaction. 2nd ed. 2001; Sage Publications: London.
- UN Population Fund. International Conference on Population and Development Programme of Action 1994. www.unfpa.org/public/icpd/
- UN Commission on Population and Development. (45th session, 2012) Draft Resolution on Adolescents and Youth, E/CN.9/2012/8. www.un.org/esa/population/cpd/cpd_resolutions.html.
- AS Erulkar, CJ Onoka, A Phiri. What is youth-friendly? Adolescents' preferences for reproductive health services in Kenya and Zimbabwe. African Journal of Reproductive Health. 9(3): 2005; 51–58.
- H Birungi, F Obare, A van der Kwaak. Maternal health care utilization among HIV-positive female adolescents in Kenya. International Perspectives on Sexual and Reproductive Health. 37(3): 2011; 143–149.doi: 10.1363/3714311.
- Senefeld S, Miller C, Mgugu D, et al. Self-esteem, self-efficacy and hope among vulnerable adolescents affected by HIV participating in community-based savings and lending groups in rural Nyanga district, Zimbabwe. Presented at 19th International AIDS Conference, Washington, DC, 2012. Abstract No. WEAE0402.
- Mukasa Mbooga B, Kawuma E, Batamwita R, et al. Responding to the sexual and reproductive health needs of adolescents living with HIV and AIDS: the Mildmay Uganda experience. Paper presented at 19th International AIDS Conference, Washington, DC, 2012. Abstract No. MOPE668.
- I Hodgson, A Nakiyemba, J Seeley. Only connect — the role of PLHIV group networks in increasing the effectiveness of Ugandan HIV services. Aids Care: Psychological and Socio-Medical Aspects of AIDS/HIV. 24(11): 2012; 1368–1374.doi: 10.1080/09540121.2012.656568.
- R de Souza. Creating “communicative spaces”: a case of NGO community organizing for HIV/AIDS prevention. Health Communication. 24(8): 2009; 692–702.doi: 10.1080/10410230903264006.
- TJ Rochat, N Mkwanazi, R Bland. Maternal HIV disclosure to HIV-uninfected children in rural South Africa: a pilot study of a family-based intervention. BMC Public Health. 13(1): 2013; 147. doi: 10.1186/1471-2458-13-147.
- R Cook, BM Dickens. Recognizing adolescents' ‘evolving capacities’ to exercise choice in reproductive healthcare. International Journal of Gynecology & Obstetrics. 70(1): 2000; 13–21.
- LS Wiener, HB Battles. Untangling the web: a close look at diagnosis disclosure among HIV-infected adolescents. Journal of Adolescent Health. 38(3): 2006; 307–309.
- Benavides Torres RA, Villarruel A, Rew L, et al. Parents' and adolescents' influences on Mexican adolescents' intentions for sexual behaviors: a model building approach. Paper presented at 17th International AIDS Conference, 2008. Abstract No. WEPE0852.
- KS Miller, KD Maxwell, AM Fasula. Pre-risk HIV-prevention paradigm shift: the feasibility and acceptability of the Parents Matter! Program in HIV risk communities. Public Health Report. 125(Suppl.1): 2010; 38–46.
- Kisaakye VNK, Nyombi J, Nakalawa L. Designing interventions for parents/guardians of HIV perinatally infected adolescents in Uganda. Presented at 5th IAS Conference on HIV Pathogenesis and Treatment. Cape Town, 2005. Abstract No. WEPED200.
- C Stefan, PL van der Merwe. Treating adolescents in South Africa: time for adolescent medicine units?. South African Medical Journal. 98(3): 2008; 184–185. 187.
- ED Lowenthal, D Szalda, N Harari. Relationship of training to self-reported competency and care of adolescents in an African health care setting. Journal of Adolescent Health. 49(4): 2011; 431–433.
- Chimulwa TN, Nyombi JK, Birungi J. Evaluation of strengthening HIV counselor training (SCOT) project in Uganda: successes and lessons learnt. Paper presented at HIV Capacity Building Summit, Nairobi, 2011. www.hivcapacityforum.org/userfiles/Chimulwa%20T.pdf.
- Gamanya G. Improving the quality of care for adolescents living with HIV/AIDS by introducing psychosocial support services at Beatrice Road Infectious Disease Hospital Opportunistic Infections and Antiretroviral Therapy clinic in Harare, Zimbabwe. Paper presented at 18th International AIDS Conference, Vienna, 2010. Abstract No. TUPE0832.