Abstract
The majority of abortions in Colombia continue to take place outside the formal health system under a range of conditions, with the majority of women obtaining misoprostol from a thriving black market for the drug and self-administering the medication. We conducted a cost analysis to compare the costs to the health system of three approaches to the provision of abortion care in Colombia: post-abortion care for complications of unsafe abortions, and for legal abortions in a health facility, misoprostol-only medical abortion and vacuum aspiration abortion. Hospital billing records from three institutions, two large maternity hospitals and one specialist reproductive health clinic, were analysed for procedure and complication rates, and costs by diagnosis. The majority of visits (94%) were to the two hospitals for post-abortion care; the other 6% were for legal abortions. Only one minor complication was found among the women having legal abortions, a complication rate of less than 1%. Among the women presenting for post-abortion care, 5% had complications during their treatment, mainly from infection or haemorrhage. Legal abortions were associated not only with far fewer complications for women, but also lower costs for the health system than for post-abortion care. We calculated based on our findings that for every 1,000 women receiving post-abortion care instead of a legal abortion within the health system, 16 women experienced avoidable complications, and the health system spent US $48,000 managing them. Increasing women’s access to safe abortion care would not only reduce complications for women, but would also be a cost-saving strategy for the health system.
Résumé
La majorité des avortements en Colombie se déroulent encore hors du système de santé formel, dans différentes circonstances. La plupart des femmes obtiennent le misoprostol sur un marché noir florissant et s’auto-administrent la médication. Nous avons comparé les coûts pour le système de santé de trois approches de la prestation de soins en matière d’avortement en Colombie : soins post-avortement pour les complications des avortements à risque, et pour les avortements légaux dans un centre de santé, avortement médicamenteux uniquement avec le misoprostol et avortement par aspiration. Les dossiers de facturation des soins hospitaliers de trois institutions, deux grandes maternités et un dispensaire spécialisé en santé génésique, ont été analysés pour les procédures et taux de complications, et les coûts par diagnostic. La majorité des visites (94%) concernaient les deux hôpitaux pour des soins post-avortement ; les 6% restants se rapportaient à des avortements légaux. Seule une complication mineure a été observée parmi les femmes ayant subi un avortement légal, soit un taux de complication de moins de 1%. Parmi les femmes s’étant présentées pour des soins post-avortement, 5% avaient eu des complications pendant leur traitement, principalement dues à une infection ou une hémorragie. Les avortements légaux étaient associés avec un taux nettement inférieur de complications pour les femmes, mais aussi avec des coûts plus modiques pour le système de santé que les soins post-avortement. Sur la base de nos conclusions, nous avons calculé que sur 1000 femmes recevant des soins post-avortement au lieu d’un avortement légal au sein du système de santé, 16 présentaient des complications évitables et le système de santé dépensait $US 48 000 pour les prendre en charge. Élargir l’accès des femmes à des services d’avortement sûr réduirait les complications pour les femmes, mais serait aussi une stratégie de réduction des coûts pour le système de santé.
Resumen
La mayoría de los abortos en Colombia continúan ocurriendo fuera del sistema formal de salud bajo una variedad de condiciones, y la mayoría de las mujeres obtienen misoprostol de un floreciente mercado negro para el medicamento y se lo autoadministran. Realizamos un análisis de costos para comparar los costos del sistema de salud en tres estrategias para la prestación de servicios de aborto en Colombia: atención postaborto para las complicaciones de abortos inseguros; y para la interrupción legal del embarazo (ILE) en una unidad de salud, aborto con medicamentos inducido con misoprostol solo y aborto con aspiración por vacío. Se analizaron los registros hospitalarios de facturación de tres instituciones, dos maternidades importantes y una clínica especializada en salud reproductiva, con relación a los procedimientos y tasas de complicaciones, y costos por diagnóstico. La mayoría de las mujeres (el 94%) acudieron a los dos hospitales para recibir atención postaborto; el 6% fue para una ILE. Se encontró una sola complicación menor entre las mujeres que tuvieron una ILE, una tasa de complicaciones de menos del 1%. Entre las mujeres que acudieron en busca de atención postaborto, el 5% presentó complicaciones durante el tratamiento, principalmente infección o hemorragia. La ILE estaba asociada no solo con mucho menos complicaciones para las mujeres, sino también con menores costos para el sistema de salud, en comparación con la atención postaborto. Basándonos en nuestros hallazgos, calculamos que por cada 1000 mujeres que recibieron atención postaborto en vez de una ILE en el sistema de salud, 16 mujeres presentaron complicaciones evitables, y el sistema de salud gastó US $48,000 manejándolas. Ampliar el acceso de las mujeres a los servicios de aborto seguro no solo reduciría las complicaciones para las mujeres, sino que también sería una estrategia de reducción de costos para el sistema de salud.
Unsafe abortion has significant social, economic and personal costs.Citation1 It also contributes greatly to maternal mortality and morbidity rates, especially in countries with restrictive abortion laws.Citation2,3 There is clear evidence that restricting access to legal abortion is associated with increased rates of unsafe abortion and harm to women. In Latin America, where abortion is widely restricted, unsafe abortion is responsible for 12% of maternal deaths.Citation3 In Colombia unsafe abortion is estimated to be the fifth leading cause of maternal mortality.Citation4,5 In this paper, we discuss the consequences of restricted access to safe abortion and the associated costs for the health system in Colombia.
Prior to 2006, abortion was illegal for all indications in Colombia, and only post-abortion care (PAC) was available within the health system.Citation6 PAC in Colombia is a form of essential emergency obstetrical care to manage the complications of abortion, including incomplete abortion. Interventions used for PAC vary widely, depending on the health system. Traditionally, resource-intensive interventions, most commonly sharp curettage (D&C), have been used. Evidence supports the greater safety and efficacy of medical or aspiration methods for management of incomplete abortion, however, as compared with D&C. The World Health Organization recommends that either manual (MVA) or electric (EVA) vacuum aspiration be used instead of D&C, as D&C is associated with a higher rate of complications.Citation7 In Colombia, however, the majority of PAC is still provided using D&C under general anaesthesia.Citation9
As found in other countries, the criminalization of abortion in Colombia promotes a flourishing underground industry for abortion, where many women obtain misoprostol from the black market and self-administer the medication, or receive sub-standard care from unsafe providers.Citation6,8 In Colombia, prior to the 2006 change in the law, hospital admissions for PAC were estimated at 58,000 annually.Citation1,9
In May 2006, advocacy efforts contributed to the partial decriminalization of abortion in Colombia.Citation10 Abortion is no longer a criminal offence in three instances: if the pregnancy constitutes a threat to the woman’s health or life, if the fetus has anomalies incompatible with life, or if the pregnancy is the result of rape or incest.Citation8 A medical certificate confirming the applicability of one of these circumstances is required, and if rape is given as the indication, a legal certificate is necessary. No upper gestational age limit is specified in the law, and the signature of a specialist is not required.Citation11 In the months following the change in the law, the Colombian Ministry of Health and Social Protection endorsed technical norms for the provision of safe abortion, and misoprostol was approved for use in medical abortion.
While abortion law reform is a necessary pre-condition for improving safety and care for women, it is not enough to guarantee access to safe abortion. Information on how these changes in policy in Colombia have affected women’s access to safe abortion is limited. Initial reports indicate that challenges to accessing safe abortion in Colombia persist.Citation5,8 Lack of knowledge about the requirements for legally accessing abortion services, as well as the unwillingness of many physicians or institutions to provide services, have restricted women exercising their rights under the new law.Citation8,12 A study published in 2011, based on a survey of health providers and national level data, estimated that despite the law reform, 99% of abortions still occurred outside the health systemCitation9 and were more likely to be associated with both acute and long-term complications for women, creating costs for the health system.Citation1,7 A complication rate of 56–65% was found with abortions that were self-induced or provided by a traditional midwife.Citation9 It was also estimated that only a third of women experiencing complications from unsafe abortion accessed the health system for treatment.Citation9 This contrasts sharply with the 0.3—1.8% minor complication rate seen in countries with unrestricted access to safe abortion.Citation7,13
Barriers to obtaining a safe abortion exist at several levels in Colombia. Abortion remains highly stigmatized, and the process for obtaining a legal abortion is cumbersome,Citation8 and few facilities are equipped or willing to offer abortion services. Currently, only 11% of facilities eligible to offer abortion services in Colombia do so. They cite lack of equipment and infrastructure, as well as the absence of trained personnel as reasons for not providing safe abortion.Citation9 The majority of legal abortions currently occur in specialized private reproductive health clinics. Although technical guidance for abortion care has been issued, it is not known whether or how it has influenced practice outside the specialized reproductive health facilities. D&C is still commonly used for both legal abortion and PAC, which is thought to be due partially to lack of access to MVA equipment and training,Citation9 and the additional barrier of the cost of obtaining them.
Data on costs are useful in determining which services to implement when resources are scarce.Citation14,15 We hypothesized that the current costs to the health system of providing post-abortion care exceed the costs of offering safe abortions. In particular, the costs to the health system of offering medical abortion would provide substantial savings compared to offering only aspiration abortion. To test this hypothesis, this study compared the costs of four treatment approaches to the provision of abortion care: PAC, misoprostol-only medical abortion (MA), MVA and D&C.
Methods
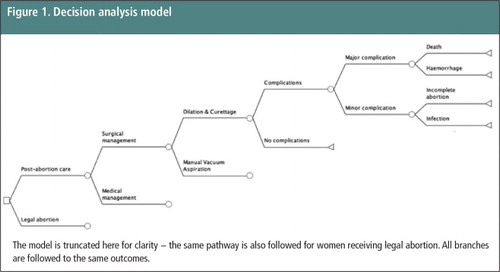
A decision analysis model was developed using TreeAge Software (Williamstown, MA, USA). Decision analysis is a tool that allows stepwise comparison of probabilities and outcomes of different options, such as the choice between medical or aspiration abortion methods. In this study, we built a model to facilitate comparison of different strategies for managing first trimester abortion (). We compared the costs and complications of all strategies currently used in Colombia: PAC, misoprostol-only MA, and MVA or D&C. Use of decision analysis allowed us to systematically examine each variable, and model results under a range of circumstances. This methodology also allows us to see how our results might be generalizable to other populations. Our primary outcome was the cost for each type of abortion care. Secondary outcomes included health complications. The perspective adopted was that of the health system. Because the data had all identifying information removed before it was made available to us, the WHO Ethical Review Committee and institutional review boards at all study sites declared the study exempt from ethical review.
The model was populated with data obtained from all abortion patients seen at three sites in Colombia during the calendar year 2012, selected because they were high volume institutions that offer legal abortions and PAC, and treat women with spontaneous abortions as well.Footnote* Costs and abortion outcome data were obtained from a convenience sample of one year of records at all three sites.
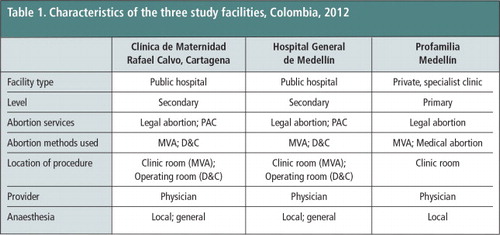
Two of the three sites were public maternity hospitals (Clínica de Maternidad Rafael Calvo, Cartagena; Hospital General de Medellín, Medellín). We specifically selected sites outside of Bogotá, to examine the experience of women outside the capital. All three institutions submitted descriptions of current protocols for management of legal abortion and PAC.
The two hospitals are large, secondary level facilities caring for more than 8,000 women a year, where women were generally seeking treatment for incomplete abortion. They presented to the emergency room, and the gynaecology ward was subsequently consulted. D&C and MVA were the methods used at both hospitals. Procedure selection depended on whether a trained provider was available and the time of day. A provider trained in MVA was only available on weekdays and during specific hours. An overnight admission was not compulsory at either site.
The third site was a specialist reproductive health clinic, Profamilia Medellín, which is a private, non-profit clinic, part of a national network, offering comprehensive reproductive health care for women and adolescents, including legal abortion using MVA or misoprostol. Services are packaged to include a consultation, examination including ultrasound, and assistance with obtaining legal abortion. Assistance to obtain a legal abortion included completing the necessary administrative forms to qualify for the different exemptions. Discounted rates are offered for adolescents. Table 1 summarizes the characteristics of the services offered at each site.
The model sequence begins with abortion, either initiated within the health system (legal abortion), or outside it (). The model is truncated for clarity – women presenting for legal abortion or post-abortion care can be managed with either a medical or surgical method = a medical or surgical method (MVA or D&C). The probability of complications is considered in both pathways of the model, and all branches are followed to the same outcomes.
An abortion, whether spontaneous or induced, and whether provided in safe or unsafe conditions, can be complete or incomplete and complicated or uncomplicated. As shown in Table 1, the Profamilia clinic used either MVA or misoprostol-only medical abortion for legal abortions. For PAC, the two large hospitals used MVA or D&C, both for management of incomplete abortion and more serious complications. We defined PAC as any care provided (medical, aspiration or surgical) for women presenting with an abortion initiated outside of the health system. We considered an abortion as complicated if it was incomplete and required an intervention, or associated with any of the following: repeat surgery, uterine perforation, infection, referral to another site, haemorrhage, or death. We considered only immediate complications in our model.
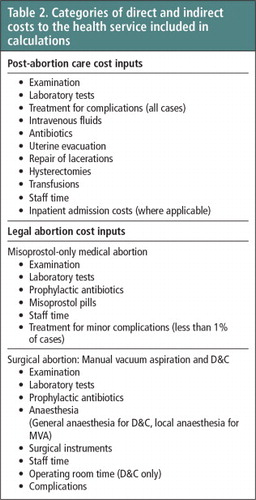
Probabilities were obtained for procedure type (legal abortion or PAC and management strategies: surgical or medical) and complications from our database of hospital visits. Hospital costs for each procedure type were determined from hospital diagnosis codes and billing records for fiscal year 2012. To include estimates of both direct costs of medical care, and indirect costs, costs were calculated from total charges. Total charges by procedure type were obtained from billing records, and costs estimated by using the cost-to-charge ratio. Types of costs considered are listed in Table 2 . Mean costs were sorted by procedure code, and stratified by whether the case was with or without complication. Only the costs from a single episode of direct medical care were considered; no future costs were projected. Out-of-pocket payments by women were not included.
Sensitivity analysis is a statistical tool used to analyse how varying one or more parameter can alter model results. Univariate and multivariate sensitivity analyses were performed to test model assumptions and determine robustness of results. Univariate sensitivity analysis was performed on all inputs. We varied each input from 50% to 200% of base estimates to identify if any threshold values existed. This allowed us to analyse how changes in our model inputs or assumptions might alter study results. For example, medical costs are known to vary widely. As our base estimate for the cost of each procedure, we used the mean cost calculated from our database. For each variable, we ranged the cost from half of our base estimate to twice the value of our base estimate, and looked to see if the model results changed. This allowed us to see what the results would be when our base estimates varied, and increased the generalizability of our findings.
Findings
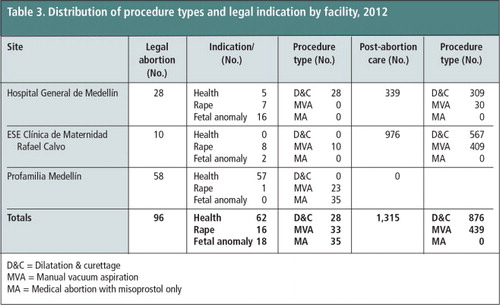
Facility records
A total of 1,411 women sought abortion care at all three sites in 2012. The great majority, 94%, were for PAC (Table 3). Each site provided a small number of legal abortions (range 10–58 cases) out of the 1,411 cases. The type of procedure used varied considerably by site. At the Profamilia clinic, only medical abortion and MVA were provided. Of women requesting a legal abortion at the Profamilia clinic, 37% had a medical abortion and the remainder an MVA. No PAC cases were seen, and D&C was not utilized. At the two hospitals, both MVA and D&C were used for legal abortion and PAC. Among women requesting legal abortion at the hospitals, 74% had a D&C and the remainder MVA. With respect to PAC at the hospitals, 67% of women had a D&C, and the remainder MVA. Management with misoprostol for either legal abortion or PAC was not observed at either of the two hospitals.
D&C = Dilatation & curettage
MVA = Manual vacuum aspiration
MA = Medical abortion with misoprostol only
The great majority of the women seeking care across the three facilities needed PAC and attended one of the two hospitals. Only 6% of the visits were for legal abortion (96 out of 1,411; p<.05). Complication rates were overall low, and consistent with the literature.Citation16 One minor complication was present among women having legal abortions, for a complication rate of less than 1%. Among the 1,315 women presenting for PAC, 76 of the cases (5%) were complicated, requiring additional surgical or medical management, mainly due to infection or haemorrhage (data not shown, p<.05).
Model results
We then examined how probabilities for procedure type, costs and complications affected overall costs and analysed the overall costs for the health system using our economic model (). We applied our model’s findings to a hypothetical cohort of 1,000 women in Colombia. Legal abortions with both MVA and medical abortion were associated with fewer health complications for women than abortions requiring post-abortion care, and the legal abortions with both methods led to cost savings for all three facilities. For every 1,000 women receiving PAC instead of legal abortion, 16 women had unnecessary complications, at a cost of US$48,000.
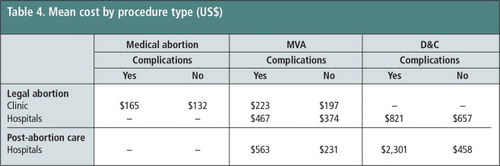
For legal abortion, both misoprostol and MVA were less costly than D&C, for both complicated and uncomplicated cases (Table 4). Costs of legal abortion varied by facility. The average cost of an uncomplicated MVA at the clinic was nearly half the cost of the same procedure at the two hospitals ($197 versus $374). The cost of an uncomplicated, clinic-based MVA was nearly a third of the cost of a hospital-based D&C ($197 versus $657). Complicated cases were even more expensive, regardless of procedure type, with implications for resources and quality of care.
For uncomplicated PAC, the average cost for an MVA was nearly half the cost of a D&C at the same type of facility ($231 versus $458). Management of complications with misoprostol for PAC cases was not observed. Complicated PAC cases were more expensive, regardless of procedure type. Abortions in the hospitals were more expensive than those in the clinic, across all types of care observed.
Thus, PAC was associated with increased costs as well as more complications. This remained true across ranging assumptions in sensitivity analysis. Sensitivity analysis demonstrated that legal abortion would need to cost more than $734 per case for PAC to be a cost-saving strategy. If we assume a 9% spontaneous abortion rate (based on population level estimates), and if the remainder of PAC cases currently observed were replaced with legal abortion (medical or MVA), the health system would save an additional $163,000 dollars and prevent 16 complications per 1,000 abortions. We also evaluated how changing hospital practice to eliminate sharp curettage would affect health outcomes and costs. We ran the model replacing D&C with either medical abortion or MVA, and estimated outcomes for a population of 1,000 women. The health system could save an additional $177,000 (per 1,000 women) from baseline, by replacing D&C with MVA.
Discussion
This study demonstrates the harm for women of restricted access to abortion, and the higher costs to the health system as well. Partial legal reform alone in Colombia has not been adequate to guarantee women their right to safe legal abortion services. The great majority of women in our study (94%) were still seeking abortion care outside of the hospital system.
While both WHO-approved methods of legal abortion (aspiration and medical methods) are safe, and associated with a similarly low rate of complications, the cost-savings for the health system could be expanded by increasing existing medical abortion services and incorporating modern aspiration methods. Sharp curettage has not been approved by WHO for many years now, as it is on average twice the cost of either medical abortion or MVA, and is associated with higher rates of complications.Citation16 The health system could save additional funds and reduce complications by replacing D&C with medical abortion or MVA.
Limited service-level data exist on the provision of legal abortion and of PAC in restricted settings like Colombia. Our study provides an analysis of abortion care from three sites in the country in two cities in Colombia. Our sample size was small, with only 58 legal abortions included. We included data from only one specialized reproductive health clinic in our sample, Profamilia. This limits the generalizability of our findings. As with all decision models, outcomes are dependent on the accuracy and availability of model inputs. We performed sensitivity analysis around all variables to address this limitation. Our data are restricted to the experience of women within the health care system. We were unable to include information on the experience of women before accessing the health system, who presented requesting PAC. Despite these limitations, the findings are clear, significant, and consistent with findings in Mexico City following a change in their abortion law.Citation19
Our findings indicate that medical abortion is an under-utilized option for legal abortion services and is not used at all for PAC. Medical abortion is an option valued by many women, and is cost-effective for the health system to provide.Citation17,18 We were not able to study the provision of mifepristone with misoprostol for medical abortion, as mifepristone is unavailable in Colombia. This results in an underestimate of the cost-savings and efficacy of medical abortion when using both medications.
The continuing prevalence of the use of D&C for both post-abortion care and legal abortion care is worrying. It is uncertain exactly why it persists. Limited availability of MVA equipment and training certainly contributes, but we suspect that increased efforts to introduce MVA and medical abortion, improve training and raise awareness of the harms of D&C will all be needed to change this ingrained practice, which we believe is urgent.
Increasing access to medical abortion for women would improve health outcomes and reduce costs for the health system. Registration of mifepristone in Colombia, to allow combined medical abortion, a more effective regimen, would further improve both health and cost outcomes. Legal reform was a positive step towards securing access to safe abortion for women in Colombia, but it has not yet benefited the great majority of women. Efforts to remove remaining barriers to safe abortion services must be strengthened.
Acknowledgements
We acknowledge the technical and financial support from HRP (UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction). We would like to acknowledge contributions made by Alison Edelman, Leandro Chavez, Laura Margarita Bello-Alvarez, Joaquin Guillermo Gomez-Davila, Juan Guillermo Londoño, Bernardo Agudelo and Andres Macias to protocol development and data collection.
Notes
* A small proportion of women presenting will have had spontaneous abortions. We included them in our analysis because women presenting for miscarriage management are also affected by hospitals using outdated procedures for abortion care (especially D&C) and the health system bears the costs, as do women presenting for PAC. Although we did not make the distinction between spontaneous and self-induced abortion rates in the database, the rate of spontaneous abortion was explored with sensitivity analysis.
References
- S Singh. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. Lancet. 368(9550): 2006; 1887–1892.
- DL Billings, J Benson. Postabortion care in Latin America: policy and service recommendations from a decade of operations research. Health Policy and Planning. 20(3): 2005; 158–166.
- World Health Organization. Unsafe Abortion: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2008. 6th ed, 2008; WHO: Geneva.
- L Cuevas. Análisis de la información de la vigilancia rutinaria. Informe Quincenal Epidemiológico Nacional. 21(5): 2007; 65–76.
- HB Johnston, MF Gallo, J Benson. Reducing the costs to health systems of unsafe abortion: a comparison of four strategies. Journal of Family Planning and Reproductive Health Care. 33(4): 2007; 250–257.
- AC González Vélez. [Current situation with abortion in Colombia: between illegality and reality]. Cadernos de Saude Publica. 21(2): 2005; 624–628. [In Spanish].
- World Health Organization. Safe Abortion: Technical and Policy Guidance for Health Systems. 2012; WHO: Geneva.
- ED Amado, MC Calderon Garcia, KR Cristancho. Obstacles and challenges following the partial decriminalisation of abortion in Colombia. Reproductive Health Matters. 18(36): 2010; 118–126.
- ESS Prada, L Remez, C Villarreal. Unintended pregnancy and induced abortion in Colombia: causes and consequences. 2011; New York City: Guttmacher Institute.
- M Ceaser. Court ends Colombia’s abortion ban. Lancet. 367(9523): 2006; 1645–1646.
- Women’s Link Worldwide. Lo que hay que saber sobre el aborto legal en Colombia (2006–2013). 2013; Bogota.
- AC González Vélez. “The health exception”: a means of expanding access to legal abortion. Reproductive Health Matters. 20(40): 2012; 22–29.
- TA Weitz, D Taylor, S Desai. Safety of aspiration abortion performed by nurse practitioners, certified nurse midwives, and physician assistants under a California legal waiver. American Journal of Public Health. 103(3): 2013; 454–461.
- D Hu, SM Bertozzi, E Gakidou. The costs, benefits, and cost-effectiveness of interventions to reduce maternal morbidity and mortality in Mexico. PLoS One. 2(8): 2007; e750.
- D Hu, D Grossman, C Levin. Cost-effectiveness analysis of alternative first-trimester pregnancy termination strategies in Mexico City. British Journal of Obstetrics and Gynaecology. 116(6): 2009; 768–779.
- L Say, R Kulier, M Gulmezoglu. Medical versus surgical methods for first trimester termination of pregnancy. Cochrane Database System Review. 1: 2005. CD003037.
- MI Rodriguez, A Seuc, N Kapp. Acceptability of misoprostol-only medical termination of pregnancy compared with vacuum aspiration: an international, multicentre trial. British Journal or Obstetrics and Gynaecology. 119(7): 2012; 817–823.
- MM Lafaurie, D Grossman, E Troncoso. Women’s perspectives on medical abortion in Mexico, Colombia, Ecuador and Peru: a qualitative study. Reproductive Health Matters. 13(26): 2005; 75–83.
- C Levin, D Grossman, K Berdichevsky. Exploring the costs and economic consequences of unsafe abortion in Mexico City before legalisation. Reproductive Health Matters. 17(33): 2009; 120–132.