?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Introduction
Many workers in Alexandria are exposed to a variety of occupational and environmental allergens and/or irritants that predispose them to the development of bronchial asthma. The present study was conducted to determine the role of occupational exposure as a determinant of occurrence of bronchial asthma and to assess the possible role of total serum IgE; eosinophil count and GSTM1 and GSTT1 null polymorphism as risk factors for the development of bronchial asthma.
Methods
A case control study was conducted in which 100 workers with bronchial asthma were compared to 100 non asthmatic controls regarding their occupational characteristics, bronchodilator responsiveness, blood analysis for eosinophil count, total serum IgE, GSTM1 and GSTT1 genotypes.
Results
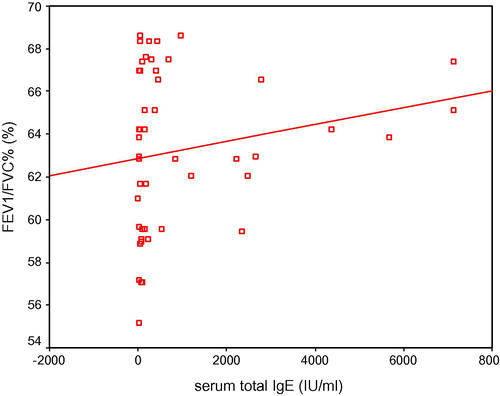
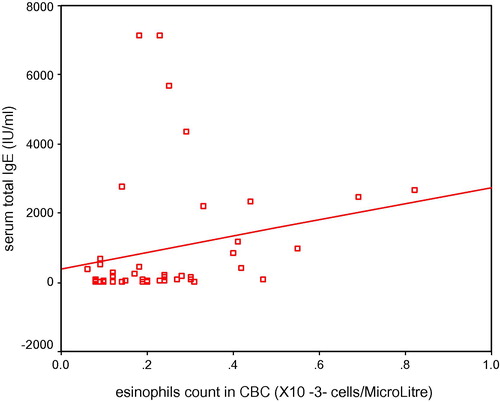
Exposure to irritants and allergens were significantly higher among workers with bronchial asthma compared to controls (86% vs. 64%, respectively, P = 0.00). Moreover, workers exposed to irritants were found to be 4 times at a higher risk of developing bronchial asthma, and those exposed to high molecular weight (HMW), and/or low molecular weight (LMW) were about three times at a higher risk of developing bronchial asthma. There was no significant difference detected between the cases of bronchial asthma and the controls regarding the frequency of the Null-genotype for either GSTT1 or GSTM1. However, the frequency of combined Null-genotype for both GSTT1 and GSTM1 was significantly higher in asthmatic workers than in controls. A significant positive correlation was found between total serum IgE level and pre-bronchodilator FEV1/FVC% (r = 0.29, and P = 0.03).
Conclusion
Occupational exposure to irritants and/or allergens is a significant risk factor for the occurrence of bronchial asthma among workers. On the other hand, eosinophil count and total serum IgE neither predicts the occurrence of bronchial asthma nor affects the severity and pattern of the disease among workers with bronchial asthma. Moreover, the present study concluded that GSTM1 and GSTT1 Null-genotypes are not likely to act as risk factors for the development of bronchial asthma. However, combined GSTT1 and GSTM1 Null-genotypes were considered as a potential risk factor for the development of bronchial asthma.
Abbreviations:
- ATS
- American thoracic society
- ETS
- environmental tobacco smoke
- FEV1
- forced expiratory volume at one second in liters (L)
- FEV1%
- forced expiratory volume at one second as percent of forced vital capacity
- FVC
- forced vital capacity in liters (L)
- HMW
- high molecular weight
- LMW
- low molecular weight
- MRC
- medical research council
- OA
- occupational asthma
- PPDs
- personal protective devices
- SABA
- short-acting β2 agonist
- ROS
- reactive oxygen species
1 Introduction
Bronchial asthma is a state of airflow limitation and/or bronchial hyper responsiveness (BHR) resulting from a persistent inflammatory process in response to a number of stimuli in a genetically susceptible individual. Simple definition of occupational asthma (OA) is asthma due to causes and conditions attributable to a particular working environment and not to stimuli encountered outside the workplace.Citation1
There is more emphasis on defining OA based on mechanism. Thus, allergic-type OA involves allergic/immunologic sensitization to a substance or material present in the worksite and excluding other occupational causes of variable air flow limitation not due to sensitization. For the allergic type of OA, a key clinical feature is that asthma develops after the passage of a latent period. Exposures that lead to allergic-type OA are called allergens which are either of high or low molecular weight substances. High molecular weight (HMW) allergens are substances of animal origin (such as animal hair, urine or saliva proteins, epidermal squamae, small insects, molds, dander, bacteria, protein dust, and mites) and vegetable origin (such as wood or wood products, cotton, flax, hemp, grain, flour, and latex). Low molecular weight allergens are substances of chemical origin, metals and pharmaceuticals.Citation2
Nonallergic OA (e.g., without latency) is also called irritant-type OA. This type of asthma is usually of sudden-onset and develops after high-level workplace irritant exposure; it develops abruptly without a significant latent period. The absence of a latent period is a critical clinical feature that an allergic mechanism, sensitization, is not operative.Citation3 Allergic-type OA and work-aggravated asthma occurs much more frequently than irritant-induced asthma. The prevalence of irritant-induced asthma is 6–22% of all work-related cases.Citation3,Citation4 Exposures that lead to irritant-type OA are inhaled irritants.Citation2
Workers most commonly reported to surveillance programs for OA include paint sprayers, bakers, nurses, animal handlers, welders, farmers, waiters, cleaners, laboratory and dental technicians, forestry workers, and workers in chemical, plastics, rubber, textile, and electrical industries.Citation5
Atopy is the most significant risk factor for asthma development, with approximately 85% of children who develop asthma and 40–50% of adults with new-onset asthma having an allergic response to aeroallergens.Citation6–Citation8 Atopy represents a complex gene-environment interaction in which environmental antigens interact with the immune system, producing atopic (IgE) responses.Citation9 Several studies reveal a link between IgE and asthma.Citation7,Citation10,Citation11 Some studies demonstrated that elevated pre-employment total serum IgE is a risk factor.Citation12
In the context of new candidate genes for asthma, the presence of airway inflammation is an important biochemical feature of asthma. There is evidence that a genetic predisposition may alter the capability of the airway to protect itself against inhaled toxic substances from the environment. Oxidative stress, with the formation of reactive oxygen species (ROS), is a key component of inflammation.Citation13,Citation14 Although host antioxidant defenses should detoxify ROS, individuals differ in their ability to deal with an oxidant burden, and such differences are in part genetically determined. Inability to detoxify ROS should perpetuate the inflammatory process, activate bronchoconstrictor mechanisms, and precipitate asthma symptoms.Citation14
Among lung antioxidants, glutathione is a key element and considered a susceptibility factor for OA. In humans, glutathione S-transferases (GSTs) represent a large and diverse super family of enzymes which play an important role in the functioning of antioxidant defenses.Citation15 Accordingly, members of the glutathione-S-transferase (GST) supergene family are potential candidates for genetic studies for their linkage to asthma, as enzymes encoded by them are critical in the protection of cells from ROS because they can utilize as substrates a wide variety of products of oxidative stress.Citation16 The GSTM1 and GSTT1 are the code names for GSTmu and GSTtheta enzymes that belong to the glutathione S-transferase (GST) genes super family.Citation15 They have been known to abolish enzymes activity and increase susceptibility to oxidative stress. Polymorphic variants in the class glutathione-S-transferase locus GSTM1 and GSTT1 influence how an individual handles an inflammatory-derived ROS burden.Citation16 Data, from previous studies, showed that particular genotypes are associated with an increased susceptibility to and/or poor outcome in several inflammatory pathologies.Citation17
Few studies examined the hypothesis that polymorphism in the GSTM1, GSTT1, and GSTP1 loci is associated with asthma and related phenotypes. Studies have reported contradictory results regarding any association between GST gene polymorphism and asthma.Citation17–Citation23
Objective assessments of pulmonary function are necessary for the diagnosis of asthma because medical history and physical examination are not reliable means of excluding other diagnoses or of characterizing the status of lung impairment. Although physicians generally seem able to identify a lung abnormality as obstructive, they have a poor ability to assess the degree of airflow obstruction or to predict whether the obstruction is reversible.Citation6 Spirometry measurements – forced expiratory volume at one second (FEV1), forced vital capacity (FVC), FEV1/FVC – before and after the patient inhales a short-acting bronchodilator should be done to determine whether there is airflow obstruction, its severity, and whether it is reversible over the short term.Citation24,Citation25 A reduced ratio of FEV1, and FEV1/FVC relative to references or predicted values indicates airflow obstruction, whereas a proportionately reduced FVC with a normal or increased FEV1/FVC ratio suggests a restrictive pattern. The severity of airflow obstruction is evaluated by comparison of the patient’s results with reference values based on age, height, sex, and race.Citation26
Many workers in Alexandria are exposed to varieties of occupational and environmental allergens and/or irritants that predispose them to the development of bronchial asthma. In spite of the extent of occupational exposures and the fact that bronchial asthma and work-related asthma are nowadays often preventable by early detection of genetically predisposed individuals and cessation of exposure to the causative agent,Citation27 yet, little attention has been given to the problem; as the Egyptian national table for prescribed occupational diseases till now does not include occupational asthma, and consequently, pre-placement examination for bronchial asthma is till date not conducted. The present study was conducted to determine the role of occupational exposure as a determinant of occurrence of bronchial asthma and to assess the possible role of total serum IgE; eosinophil count and GSTM1 and GSTT1 null polymorphism as risk factors for the development of bronchial asthma. The specific objectives of the current study were: (1) describe the relationship between occupational exposures and occurrence of bronchial asthma; (2) study the pattern and severity of bronchial asthma among workers; (3) reveal the relationship between eosinophil count, total serum IgE antibodies and bronchial asthma; and (4) study of GSTT1 and GSTM1 genotypes among the workers with bronchial asthma and non asthmatic controls to determine the potential role of these genes Null-genotype as a risk factor in occurrence of bronchial asthma.
2 Methods
The case control approach was adopted for this study to estimate the odds ratio, and test the hypothesis that asthma is caused by certain etiological factors such as occupational, immunologic and genetic characteristics.
The study included 100 male workers with bronchial asthma and 100 control workers who attended the Health Insurance Clinics during 8 month field work period of the study from January throughout August 2009. The unit of observation was a worker suffering from bronchial asthma as well as his free matched (age group) worker.
A bronchial asthma patient was included in the study when he was (a) a male; (b) able to perform technically acceptable pulmonary function tests; (c) 40 years old or more; (d) suffering from recurrent episodes of chest wheezing, breathlessness, chest tightness and coughing particularly at night or in the early morning; (e) non-smokers or ex-smokers with less than 10 packs/year history; and (f) clinically stable with no respiratory exacerbations for six weeks prior to inclusion in the study and with no changes in chronic medication during this period. Respiratory exacerbations were defined as an increase in breathlessness, sputum volume or sputum purulence from the baseline requiring treatment with prednisone and/or antibiotics.
The participant was included in the control group when he was (a) a male; (b) able to perform technically acceptable pulmonary function tests; (c) 40 years old or older; (d) had to be a lifetime non-smoker or an ex-smoker with less than 10 packs/year history; (e) had no respiratory symptoms or disease and never reporting physician-diagnosed respiratory disease, dyspnea, morning cough or wheeze.
Workers with bronchial asthma and controls were subjected to the following data collection tools:
| (a) | Interviewing schedule: Workers were interviewed in Alexandria Health Insurance Outpatient Clinics by a special interviewing schedule that was designed to obtain data about personal characteristics, family, medical and occupational histories; it was based on the British Medical Research Council Questionnaire (BMRC)Citation28 and the allergy questionnaireCitation29 with minor modifications to some questions to be adjusted to the Egyptian workers (can be obtained from the authors upon request). | ||||
| (b) | Anthropometric measurements: Including weight and height.Citation30 | ||||
| (c) | Spirometry: All workers included in the study underwent spirometry at the Industrial Medicine Unit affiliated to the Department of Community Medicine in the Alexandria Faculty of Medicine. The equipment used was Spirometer ST-95 version 1.1A manufactured by Fukuda Sangyo Co., Ltd. Japan in 1998. It is a computerized spirometer which can produce both volume-time and flow-volume curves. The used spirometer and the performance of the maneuver met recommendations of the American Thoracic Society (ATS) and the European Society of Clinical Respiratory Physiology.Citation31,Citation32 Maneuver of forced expiration was explained for the participant by the investigator. The test procedure was explained to each participant. The participant performed the test while seated. He was asked to take 3 deep breaths, then, to fill his chest with air till he reaches total lung capacity (TLC), then he was asked to breathe out as fast and explosive as possible till he reached his residual volume (RV). Each participant performed at least 3 test maneuvers. If the performance was unsatisfactory, the participant was asked to repeat it again. Maximum number of maneuvers was 7 times, the best 3 traces were selected provided that there was good reproducibility between the best 3 trials, i.e., the variability between them was less than 5% for the FVC and FEV1 indices and 10% for the PEF index. The highest of the three trials for each index “best test” was recorded as the final value.Citation31 For analysis, the best FEV1 and forced vital capacity (FVC) were chosen regardless of the curve. The ‘best test’ curve was selected from the largest sum of FEV1 and FVC. All other lung function parameters selected for analysis were taken from the ‘best test’ curve. Pre and post-bronchodilator lung function testing: among workers with bronchial asthma, bronchodilator treatment was withdrawn prior to pulmonary function testing according to standard practice (immediate release theophylline: 24 h, long-acting β2 agonist: 12 h, short-acting β2 agonist: 6 h and short acting anticholinergic: 8 h). The investigator conducted maximal in-and expiratory flow volume curves with the participants before (‘pre’) and 20 min after (‘post’) administration of 2 puffs (400 μg) salbutamol. The medication was given via a metered dose inhaler with a large volume spacer (Volumatic, GlaxoSmithKline).Citation33 Bronchodilator responsiveness (BDR) was calculated according to the following criteria: (1) post-bronchodilator FEV1 ⩾ 80% predicted and FEV1/FVC ratio ⩾ 70%; (2) FEV1 change from initial (=post FEV1 − pre FEV1/pre FEV1 × 100) ⩾ 12%; (3) FEV1 absolute change (=post FEV1 − pre FEV1) ⩾ 200 mL; and (4) FEV1 change from predicted (=post FEV1 − pre FEV1/predicted FEV1 × 100) ⩾ 9%. The severity of bronchial asthma was determined according to the guidelines of the National Heart, Lung, and Blood Institute in 2007.Citation34 This classification was based on the following components: (a) symptoms, such as nighttime awakening, need for short-acting β2 agonist (SABA) for quick relief of symptoms and work days missed; (b) activity levels which means the ability to engage in normal daily activities or in desired activities and (c) lung function, measured by spirometry: FEV1, FVC and FEV1/FVC; the severity of airflow obstruction is classified into mild, moderate and severe obstruction when the FEV1 is ⩾80%, 60% to <80% and <60% of predicted values, respectively.Citation34 | ||||
| (d) | Immunological investigations: Three milliliters of peripheral blood was collected, from participants who gave full agreement, in an EDTA-containing vacutainer and the following immunological investigations were done: (1) eosinophil count; eosinophilia was considered when the eosinophil count was >0.8 × 103 cells/μLCitation35; and (2) total serum IgE level using BN ProSpec of Dade Behring Marburg GmbH.Citation36 In adults, total serum IgE values of <100 IU/mL are considered normal values.Citation37 | ||||
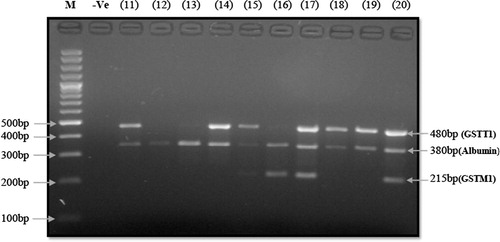
| (e) | GSTM1 and GSTT1 genotyping: The genomic DNA for genotyping was isolated from 1 mL of peripheral blood collected in an EDTA containing vacutainer using alcohol precipitation DNA extraction method (Wizard genomic DNA extraction Kit, Promega).Citation38 The GSTM1 and GSTT1 Null-genotypes were detected using a multiplex polymerase chain reaction (PCR) method.Citation39 Briefly, 100 ng of DNA were amplified in a 50-μL multiplex reaction mixture containing 10 pmol of each of the following primers: | ||||
| • | GSTM1 primers: GSTM1-F:TTCCTCACTGGTCCTCACATCTC GSTM1-R: TCACCGGATCATGGCCAGCA | ||||
| • | GSTT1 primers: GSTT1-F: GAACTCCCTGAAAAGCTAAAGC GSTT1-R: GTTGGGCTCAAATATACGGTGG. | ||||
The ALBUMIN gene was also amplified as an internal control with 5 pmol of each of its primers (Alb-F: GCCCTCTGCTAACAAGTCCTAC and Alb-R: GCCCTAAAAAGAAAATCGCCAATC). The PCR reaction contained 3.5 mM MgCl2, 200 μM dNTPs, 5 μL 10X PCR buffer, and 2U TaqDNA polymerase. Inclusion of negative control in all PCR reactions was included to ensure exclusion of any contaminations.
The PCR protocol included an initial melting temperature of 94 °C for 5 min followed by 35 cycles of denaturation at 94 °C for 40 s, annealing at 60 °C for 40 s and extension at 72 °C for 1 min. A final 7-min extension step at 72 °C terminated the process. The PCR products were analyzed on 2% agarose gels. A fragment of 215 bp indicated the presence of GSTM1; a fragment of 480 bp indicated the presence of GSTT1; and a fragment of 380 bp indicated positive internal control of albumin gene amplification. The subjects were classified as either (+) for each genotype when a PCR product is produced or (−) when they showed a Null-genotype for each of GSTM1 and GSTT1, provided that there is a PCR product for the internal control (). In case the internal control did not work, the sample was repeated.
Figure 1 Captured gel image of Multiplex PCR genotyping assay for detection of GSTT1 and GSTM1 gene deletion using 2% agarose. The subjects were classified as either (+), when at least one specimen of the gene was detected, or (−) when they showed a null genotype. Examples; participant No.11 is GSTT1 (+) and GSTM1(−); participant No.12 is GSTT1(−) and GSTM1(−); and participant No.17 is GSTT1(−) and GSTM1(+).
2.1 Statistical analysis
The collected data were coded and typed onto computer files using. SPSS/Pc + software program version 18.0.Citation40 Descriptive statistics including frequency, percentages, arithmetic mean (
), and standard deviation (SD) were used to describe workers with bronchial asthma and controls. The study also used analytic measures such as student t-test, χ2 test, and non-parametric tests. Correlations between spirometry, eosinophil count, and total serum IgE using non-parametric Spearman’s correlation were also included in the present study. The level of significance selected for this study was the 0.05 level.
2.2 Ethical clearance
The overall study objectives and procedures were explained and consents were obtained from all participants in the study. All collected data were dealt with great confidentially. The study was approved by Alexandria Faculty of Medicine Research Ethics Committee.
3 Results
3.1 Population personal characteristics
There was no significant difference between workers with bronchial asthma and controls regarding their mean age, height, weight, BMI, marital status, and smoking habit. On the other hand, there was a significant difference between workers with bronchial asthma and controls regarding their education, where workers in the control group continued their education to the secondary and/or the university level (X2 = 13.08 and P = 0.01) ().
Table 1 Personal and occupational characteristics of workers with bronchial asthma and controls.
3.2 Occupational exposure characteristics
There was no significant difference between workers with bronchial asthma and controls regarding the duration of employment, daily working hours, working status and the use of personal protective equipment at work (). About one third of workers with bronchial asthma (28%) were affiliated to textile industry followed by 18% were involved in general public services and 16% worked in chemical industry.
The study demonstrated the distribution of workers with bronchial asthma and controls according to their exposure status and the nature of exposure. The study showed that 86% of workers with bronchial asthma were exposed compared to 64% of controls; the difference was statistically significant where OR was 3.46 (1.64–7.38), X2 = 12.90, and P = 0.00. Regarding the nature of exposure among workers with bronchial asthma and controls, significantly increased ORs were found for exposure to irritants (OR = 4.35); HMW allergens (OR = 3.27); LMW (OR = 3.04); and mixed environments (OR = 3.43). The differences were statistically significant where X2 = 10.25 (P = 0.001); X2 = 5.59 (P = 0.018); X2 = 6.94 (P = 0.008); and X2 = 8.0 (P = 0.005), respectively ().
Table 2 Distribution of workers with bronchial asthma and controls according to exposure.
3.3 Study of bronchodilator response
In the present study, the mean values and the mean percent predicted values of pre-bronchodilator FEV1, FVC, and FEV1/FVC% were significantly lower in workers with bronchial asthma compared to controls.
Regarding the post-bronchodilator lung function indices in the current study, the mean value and the mean percent predicted value of post-bronchodilator FEV1 were significantly lower in workers with bronchial asthma (2.44 ± 0.19 L, and 75.15 ± 6.80%, respectively) compared to controls (4.12 ± 0.18 L, and 89.66 ± 4.75%, respectively) (P = 0.00). The mean absolute change of FEV1, the mean% change of FEV1 from the initial and the mean% change of FEV1 from the predicted were significantly higher in workers with bronchial asthma (0.42 ± 0.18L, 20.64 ± 9.02%, and 12.77 ± 5.31%, respectively) compared to controls (0.05 ± 0.14 L, 2.32 ± 1.11%, and 2.03 ± 0.93%, respectively) (P = 0.00) ().
Table 3 Mean values and mean percent predicted values of post-bronchodilator (Post-BD) FEV1, FVC and FEV1/FVC in workers with bronchial asthma and controls.
The mean value of post-bronchodilator FVC was significantly lower in workers with bronchial asthma (3.58 ± 0.19 L) compared to controls (4.95 ± 0.15 L) (t = −56.10 and P = 0.00). The mean absolute change of FVC, the mean % change of FVC from the initial, and the mean% change of FVC from the predicted were significantly higher in workers with bronchial asthma (0.37 ± 0.12 L, 11.58 ± 4.53%, and 9.37 ± 3.10%, respectively) compared to controls (−0.80 ± 0.26 L, 1.82 ± 1.27%, and 2.03 ± 0.81%, respectively) (P = 0.00) ().
The mean value of post-bronchodilator FEV1/FVC% was significantly lower in workers with bronchial asthma (68.12 ± 5.86) compared to controls (83.49 ± 3.37) (t = −22.69 and P = 0.00). The %mean change of FEV1/FVC from the initial, and the mean change of FEV1/FVC% from the predicted were significantly higher in workers with bronchial asthma (4.66 ± 6.43 and 5.30 ± 7.33, respectively) compared to controls (1.98 ± 1.23 and 2.21 ± 1.39, respectively) (P = 0.00) ().
The current study classified workers with bronchial asthma according to the severity of asthma; 58% of workers with bronchial asthma in the present study had moderate persistent bronchial asthma, 18% had mild persistent bronchial asthma, 16% had intermittent bronchial asthma and 8% had severe persistent asthma.
3.4 Eosinophil count and total serum IgE in workers with bronchial asthma
There was no significant difference between workers with bronchial asthma and controls regarding eosinophil count and total serum IgE level ().
Table 4 Eosinophil count and total serum IgE level among workers with bronchial asthma and controls.
Regarding the bronchial asthma severity categories, about 97% of workers with moderate to severe persistent asthma had normal eosinophil count compared to 3.03% who had high eosinophil count. According to the total serum IgE level, 54.54% of workers with moderate to severe persistent asthma had high level of total serum IgE compared to 45.45% who had normal level; these differences were statistically insignificant ().
Table 5 Eosinophil count and total serum IgE level in different bronchial asthma severity categories in workers with bronchial asthma.
3.5 GSTM1 and GSTT1 null polymorphism and bronchial asthma
On studying the genotype profile in a subsample of workers with bronchial asthma and controls, the presence of GSTM1 Null-genotype was compared in both sample groups. The difference in the frequency of GSTM1 Null-genotype between workers with bronchial asthma and controls was insignificant (58% and 52%, respectively, P = 0.54) (). The difference remained insignificant after stratification of the groups by exposure, which was performed to exclude the interaction effect ( and ).
Table 6 Association between genotype profile and bronchial asthma phenotype.
Table 7a Association between GSTM1 genotype profile and bronchial asthma phenotype among exposed workers with bronchial asthma and exposed controls.
Table 7b Association between GSTM1 genotype profile and bronchial asthma phenotype among non-exposed workers with bronchial asthma and non-exposed controls.
Moreover, the frequency of GSTT1 Null-genotype was compared in both sample groups; a frequency of 24% was found in asthmatic workers and 10% in controls and the difference was of a border line significance (P = 0.06) (). Stratification of the groups by exposure was done to exclude the interaction effect; the difference remained non-significant ( and ).
Table 8a Association between GSTT1 genotype profile and bronchial asthma phenotype among exposed workers with bronchial asthma and exposed controls.
Table 8b Association between GSTM1 genotype profile and bronchial asthma phenotype among non-exposed workers with bronchial asthma and non-exposed controls.
However, the study examined the association between combined GSTM1/T1 Null-genotype and asthma phenotype and showed that 20% of workers with bronchial asthma had a combined GSTM1/T1 Null-genotype compared to only 6% of the controls; this difference was found to be statistically significant (OR 3.92, 95% CI: 0.9–19.4 and P = 0.037) ().
Table 9 Association between combined GSTM1/T1 Null-genotype and bronchial asthma phenotype.
3.6 Correlation between eosinophil count, total serum IgE and bronchodilator responsiveness in workers with bronchial asthma
A significant positive correlation was found between total serum IgE level and pre-bronchodilator FEV1/FVC% (r = 0.29 and P = 0.03). Moreover, A significant positive correlation was found between total serum IgE level and eosinophil count (r = 0.38 and P = 0.00) ( and ). On the other hand, there was no significant correlation between eosinophil count, total serum IgE level and pre-bronchodilator FEV1 or FVC, their absolute change, the mean% change from the initial and the mean% change from the predicted values.
3.7 Association between GSTM1 and GSTT1 Null-genotype and bronchodilator responsiveness in workers with bronchial asthma
The association between GSTM1 Null-genotype and bronchodilator responsiveness was studied in workers with bronchial asthma. A total of 50 asthmatic patients were classified according to their GSTM1 genotyping into two groups; the first group consisted of 29 workers with bronchial asthma (58%) with GSTM1 Null-genotype and the second group consisted of 21 workers with bronchial asthma with GSTM1 WT-genotype (42%). There was no significant difference between the two groups regarding pre-bronchodilator FEV1, FVC, FEV1/FVC%, FEV1 absolute change, FEV1% change from the initial, FEV1% change from the predicted, FVC absolute change, FVC% change from the initial, FVC% change from the predicted, and FEV1/FVC% mean change ().
Table 10 Association between GSTM1 genotype and post-bronchodilator (Post-BD) change in lung function indices among workers with bronchial asthma.
Furthermore, the association between GSTT1 Null-genotype and bronchodilator responsiveness in workers with bronchial asthma was studied. A total of 50 asthmatic patients were classified according to their GSTT1 genotyping into two groups; the first group consisted of 11 workers with bronchial asthma (22%) with GSTT1 Null-genotype and the second group consisted of 39 workers with bronchial asthma with GSTT1 WT-genotype (78%). There was no significant difference between the two groups regarding pre-bronchodilator FEV1, FVC, FEV1/FVC%, their absolute and percent change from initial and predicted values ().
Table 11 Association between GSTT1 genotype and post-bronchodilator (Post-BD) change in lung function indices among workers with bronchial asthma.
4 Discussion
In the current study, exposure was found to be a significant risk factor in the development of bronchial asthma among workers. Regarding the nature of exposure among workers with bronchial asthma, significantly increased ORs were found for exposure to LMW, mixed environments, irritants, and HMW allergens. This finding was consistent with that of a study conducted by Kennedy et al.Citation41; the study reported significantly increased ORs for exposure to all low molecular weight agents combined (and in particular, to reactive chemicals and industrial cleaning agents); and Odds ratios greater than 2.0 were found for exposure to bioaerosols, metals, and to mixed environments.
In the present study, pre-bronchodilator FEV1, FVC and FEV1/FVC% were significantly lower in workers with bronchial asthma compared to controls. This finding was consistent with results reported by a study conducted by Richter et al.Citation33 where the mean percent predicted values of pre-bronchodilator FEV1, FVC and FEV1/FVC% among asthmatic patients were (59.29 ± 1.82%, 86.5 ± 2.74%, and 57.65 ± 1.16, respectively). Moreover, it was concomitant with the result of another study that was conducted to provide reference values for healthy adult population where the mean values of pre-bronchodilator FEV1, FVC and FEV1/FVC% among general adult population were (4.04 ± 0.56 L, 5.08 ± 0.75 L, and 80 ± 5%, respectively).Citation42
Post-bronchodilator FEV1, FVC and FEV1/FVC% were significantly lower in workers with bronchial asthma compared to controls in the present study. This finding was consistent with that of the study conducted by Richter et al.Citation33 in which, among bronchial asthmatic patient group in their study, the mean percent predicted values of post-bronchodilator FEV1 was 75 ± 2.1%, the mean absolute change of FEV1 was 0.445 ± 0.03 L), the mean% change of FEV1 from the initial was 27 ± 3, the mean% change of FEV1 from the predicted was 15 ± 2%, the mean absolute change of FVC was 0.375 ± 0.05 L, the mean % change of FVC from the initial was 13 ± 2% and the mean% change of FVC from the predicted was 11 ± 2%. The finding of the present study was also consistent with the finding of the study conducted by Johannessen et al.Citation42 in which the mean value of post-bronchodilator FEV1 was 4.12 ± 0.55 L, the mean absolute change of FEV1 was 0.078 ± 0.12 L, the mean value of post-bronchodilator FVC was 5.06 ± 0.75 L, and the mean absolute change of FVC was −0.022 ± 0.13 L among healthy adult population.
Eosinophil count and total serum IgE were studied among workers with bronchial asthma. There was no significant difference between workers with bronchial asthma and controls regarding eosinophil count and total serum IgE level in the current study. This result was in agreement with the results of some studies.Citation43,Citation44 On the other hand, it was inconsistent with the results of other studies which concluded that in the general population, the percentage of patients with asthma and airway responsiveness is greater among those with high IgE levels than among those with low IgE levels.Citation45–Citation47 Moreover, one group of authors reported that, among non-allergic subjects, asthma is more prevalent in those with elevated IgE levels than in those with normal IgE levels.Citation48 Previous studies have also suggested that elevated serum IgE levels are significantly associated with a higher frequency of symptoms in subjects with asthma.Citation49
In the current study, although there was a tendency for an increase in the level of total serum IgE as the severity of asthma increased, yet, the difference between the severity categories of bronchial asthma was statistically insignificant. Other studies involving adult patients with asthma in Europe, reported that total serum IgE was found to be a strong predictor of moderate-to-severe asthma.Citation50 In another study, higher total IgE levels were shown to be associated with the degree of asthma severity among younger subjects with difficult-to-treat or in those who were categorized as severe asthma.Citation51
The present study presented the findings regarding the homozygous deletions of the GSTM1 and GSTT1 genes. There was at trend of higher frequency of GSTT1 Null-genotype in asthmatic workers relative to controls, 24% and 10%, respectively, but the difference was of border line significance [OR was 0.35 (95% CI: 0.10–1.21) and (P = 0.06)]. This finding was consistent with that of the study conducted by Hanene et al.Citation52 aiming at assessing whether polymorphism of GST genes (GSTM1 and GSTT1) are associated with asthma; their study concluded that there was no significant difference between the group of bronchial asthma patients and controls regarding the presence of GSTT1 null polymorophism (37.5% and 29.5%, respectively, and P > 0.05).Citation52 Similar results were reported in other studies.Citation19,Citation20,Citation53,Citation54 However, some studies have suggested that individuals with the GSTT1∗0/∗0 (GSTT1 null) genotype are more susceptible to genotoxic damage and lung diseases than individuals with the GSTT1 gene.Citation55,Citation56
Furthermore, the GSTM1 null polymorphism was present in 58% of workers with bronchial asthma and in 52% of controls; the difference was statistically insignificant [OR was 0.78 (95% CI: 0.33–1.86) and (P = 0.54)]. This finding was consistent with that of a study conducted by Sandford et al.Citation57 On the other hand, it was inconsistent with the finding reported by Hanene et al.;Citation52 where the GSTM1 Null-genotype was significantly associated with an increased risk of asthma in which GSTM1 Null-genotype was present among 70.7% of the asthmatic patients and among 50.2% of the control group in their study (P = 0.02). Moreover, other studies have demonstrated a significant association between subjects lacking GSTM1 activity and the risk of developing bronchial asthma and/or other forms of lung disease.Citation17,Citation19,Citation53,Citation55,Citation58,Citation59
The difference in the results might be due to the difference in sample size or type of population and frequency of Null-genotype in Egyptians. For example, in the present study, the frequency of GSTM1 Null-genotype among controls was 52%; this finding was similar to the frequency previously reported by Hamdy et al.Citation60 and Saad et al.Citation61 (55.5% and 42.5%, respectively). Regarding the frequency of GSTT1 Null-genotype among controls, in the present study it was 10% which was close to that reported by Saad et al. (16%).Citation61 However, a slightly higher frequency was reported by Hamdy et al. (29.5%).Citation60
In 2007, a literature-based meta-analysis aiming at studying genetic polymorphism of GSTM1 and GSTT1 and bronchial asthma was published. The meta-analysis included 14 studies, involving a total of 2292 asthma patients and 5718 controls. The OR of the asthma risk associated with GSTM1 Null-genotype was 1.20 (95% CI: 1.08–1.35). The GSTT1 Null-genotype was not associated with asthma risk except after stratification of the groups by smoking; it was associated with asthma risk in non-smoker adults (OR = 2.06, 95% CI: 1.21–3.71).Citation62
The meta-analysis entailed further analysis combining the GSTT1 and GSTM1 genotypes. Subjects with Null-genotypes for both GSTM1 and GSTT1 were at a significant higher risk for developing asthma (OR = 2.15, 95% CI: 1.39–3.33) compared to subjects who had both active genesCitation62; this finding was consistent with the finding of the present study (OR 3.92, 95%CI: 0.9–19.4 and P = 0.037). The meta-analysis suggested that there is an additive effect for GSTT1 and GSTM1 genotypes,Citation62 which is in agreement with the results of the current study.
The results of the meta-analysis suggest that the GSTT1 and GSTM1 Null-genotypes may play an important role in asthma pathogenesis. It is possible that intermediate electrophilic metabolites, arising in the first phase of detoxification, are not metabolized by GST enzymes in asthmatic patients and are not excreted. These intermediate metabolites may damage cells and generate oxidative stress, and so contribute to the pathogenesis of asthma.Citation62
On the other hand, another recent meta-analysis conducted by Minelli et al. in 2009 and entailed meta-analyses of GSTM1 (n = 22 studies) and GSTT1 (n = 19) showed an increased asthma risk associated with the Null-genotype; however, the association disappeared when meta-analysis was restricted to the largest studies.Citation63
In the present study, a significant positive correlation was found between total serum IgE level and eosinophil count. Although this finding was consistent with that of another study,Citation64 it was inconsistent with the result of Razi et al.Citation44 who found no statistical difference between asthma patients with high and low total serum IgE levels in their peripheral blood eosinophil count (P = 0.72). Moreover, the current study found a significant positive correlation between total serum IgE level and pre-bronchodilator FEV1/FVC%. This result was inconsistent with that of a longitudinal study where a significant inverse association was found between total serum IgE levels and FEV1/FVC%; the authors suggested that higher IgE levels indicate the presence of a disease process that can involve inflammation or other mechanisms related to IgE production which can impair lung function over time.Citation65
On the other hand, the present study found no significant correlations between eosinophil count or total serum IgE and pre-bronchodilator FEV1, FVC, FEV1/FVC%, their absolute and percent change from initial and predicted values. This finding was consistent with that of the study conducted by Razi et al.Citation44 However, it was in contrast to findings reported by Endoh et al. who concluded that higher serum IgE levels are correlated with lower values of FEV1, which is related to airway tone, and possibly act via cholinergic mechanisms.Citation66 Moreover, other authors have reported that, among patients with asthma, mean FEV1 is significantly lower in those with high IgE levels than in those with low IgE levels.Citation67
In conclusion, the present study demonstrated that occupational exposure is a significant risk factor for the occurrence of bronchial asthma among workers. Moreover, it concluded that eosinophil count as well as total serum IgE neither predicts the occurrence of bronchial asthma nor affects the severity and pattern of the disease among workers with bronchial asthma. Though there was a trend of higher frequency of GSTT1 Null-genotype in asthmatic workers relative to controls, the difference was of border line significance; however, combined GSTT1 and GSTM1 Null-genotypes was considered as a potential risk factor for the development of bronchial asthma.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine
Available online 23 June 2011
References
- I.L.BernsteinM.Chan-Yeunget alDefinition and classification of asthmaI.L.BernsteinM.Chan-YeungJ.L.Maloet alAsthma in the workplace1993Marcel DekkerNew York14
- S.M.BrooksT.TruncaleJ.M.CluskeyOccupational and environmental asthmaN.Rom WilliamEnvironmental and occupational medicine 4th ed.2007Lippincott Williams & Wilkins419463
- S.M.BrooksY.HammadI.Richardset alThe spectrum of irritant-induced asthma: sudden and not-so-sudden onset and the role of allergyChest11319984249
- J.C.McDonaldH.L.KeynesS.K.MeredithReported incidence of occupational asthma in the United Kingdom, 1989–97Occup Environ Med572000823829
- A.KarjalainenK.KurppaR.Martikainenet alExploration of asthma risk by occupation extended analysis of an incidence study of the Finnish populationScand J Work Environ Health2820024957
- NHLBI. Guidelines for the diagnosis and management of asthma. Expert Panel Report 2. NIH Publication 97-4051. Bethesda, MD. National Heart, Lung, and Blood Institute; 1997.
- Committee on the Health Effects of Indoor Allergens, Institute of Medicine. Mechanisms of immune response. In: Pope A, Patterson H, Burge H, editors. Indoor allergens: assessing and controlling adverse health effects. Washington, DC: National Academy Press; 1993. p. 131–51.
- Blumenthal MN. Principles of genetics. In Middleton E, Reed C, Ellis EF, Adkinson NF, Yunginer JW, editors. Allergy, principles and practice. 5th ed. Mosby; 1998. p. 28–39.
- D.B.PedenDevelopment of atopy and asthma: Candidate environmental influences and important periods of exposureEnviron Health Perspect10832000475482
- M.HalonenD.SternL.M.Taussiget alThe predictive relationship between serum IgE levels at birth and subsequent incidences of lower respiratory illnesses and eczema in infantsAm Rev Resp Dis1461992866870
- D.L.SherillR.SteinM.Halonenet alTotal serum IgE and its association with asthma symptoms and allergic sensitization among childrenJ Allergy Clin Immunol10419992836
- A.RenstromP.MalmbergK.Larssonet alAllergic sensitization is associated with increased bronchial responsiveness: a prospective study of allergy to laboratory animalsEur Respir J8199515141519
- S.T.WeissIssues in phenotype assessmentS.B.LiggettD.A.MeyersThe genetics of asthma1996Marcel DekkerNew York401419
- P.J.BarnesReactive oxygen species and airway inflammationFree Rad Biol Med91990235243
- I.RahmanS.K.BiswasA.KodeOxidant and antioxidant balance in the airways and airway diseasesEur J Pharmacol5332006222239
- J.D.HayesR.C.StrangePotential contribution of the glutathione S-transferase supergene family to resistance to oxidative stressFree Rad Res Commun221995193207
- L.TamerM.C.AlikgluN.A.AtesGlutathione-Stransferase gene polymorphism (GSTT1, GSTM1, GSTP1) as increased risk factors for asthmaRespirology942004493498
- A.AnthonyB.AndereaH.Michaelet alPolymorphism at the Glutathione S-transferase GSTP1 locus a new marker for bronchial hyperresponsiveness and asthmaAm J Respir Crit Care Med161200014371442
- W.D.CarrollW.LenneyP.W.JonesEffects of glutathione S-transferase M1, T1 and P1 on lung function in asthmatic familiesClin Exp Allergy359200511551161
- L.I.HollaA.StejskalovaA.VaskuPolymorphism of the GSTM1 and GSTT1 genes in patients with allergic diseases in the Czech populationAllergy6122006265267
- P.PiirilaH.WikmanR.Luukkonenet alGlutathione S-transferase genotypes and allergic responses to diisocyanate exposurePharmaco-genetics112001437445
- F.D.GillilandY.F.LiL.Dubeauet alEffects of glutathione S-transferase M1, maternal smoking during pregnancy, and environmental tobacco smoke on asthma and wheezing in childrenAm J Respir Crit Care Med1662002457463
- M.KabeschC.HoeflerD.Carret alGlutathione S transferase deficiency and passive smoking increase childhood asthmaThorax592004569573
- M.R.ByeD.KersteinE.BarshThe importance of spirometry in the assessment of childhood asthmaAm J Dis Child14681992977978
- J.T.LiE.J.O’ConnellClinical evaluation of asthmaAnn Allergy Asthma Immunol7611996113
- American Thoracic SocietyStandardization of spirometry, 1994 updateAm J Respir Crit Care Med1523199511071136
- T.A.SkovstedV.SchlunssenI.SchaumburgOnly few workers exposed to wood dust are detected with specific IgE against pine woodAllergy582003772779
- Medical Research Council working party reportDefinition and classification of chronic bronchitisLancet11965775779
- B.H.BoothDiagnosis of immediate hypersensitivityR.PattersonAllergic diseases: diagnosis and management 2nd ed.1980JB Lippincott Co.Philadelphia7699
- R.BomfordS.MasonM.Swash Hutchison’s clinical methods 1985The Macmillan Publishing Company Inc.London
- American Thoracic SocietyStandardization of spirometryAm J Respir Crit Care Med152199411071136
- P.H.QuanjerG.J.TammelingJ.E.Coteset alSymbols, abbreviations and nits. Working party standardization of lung function tests, European Community for Steel and CoalEur Respir J Suppl16851993100
- D.C.RichterJ.R.JoubertH.Nellet alDiagnostic value of post-bronchodilator pulmonary function testing to distinguish between stable, moderate to severe COPD and asthmaInt J COPD342008693699
- NHLBI. Guidelines for the diagnosis and management of asthma. Expert Panel Report 3. NIH Publication 97-4051. Gregory Morosco, Ph.D., M.P.H. James Kiley, Ph.D. National Heart, Lung, and Blood Institute; 2007.
- J.GotlibMolecular classification and pathogenesis of eosinophilic disordersActa Haematol11412005725
- National Committee for Clinical Laboratory Standards. Evaluation of precision performance of clinical chemistry device; approved guideline. NCCLS document EP5-A (ISBN 1-56238-368-X). NCCLS, 940 West Valley Road, Suite 1400, Wayne, PA 19087-1898, USA; 1999.
- K.P.RingelF.DatiReference values for serum IgE in healthy non-atopic children and adultsClin Chem2819821556
- S.A.MillerD.D.DykesH.F.PoleskyA simple salting out procedure for extracting DNA from human nucleated cellsNucleic Acids Res16319881215
- C.P.DelomenieM.S.Longuemauxet alGlutathione S-transferase (GSTM1) Null-genotype and sulphonamide intolerance in acquired immunodefciency syndromePharmacogenetics761997519520
- M.J.Norusis SPSS 18.0 guide to data analysis 2008Prentice Hall
- S.M.KennedyN.L.MoualD.Choudatet alDevelopment of an asthma specific job exposure matrix and its application in the epidemiological study of genetics and environment in asthma (EGEA)Occup Environ Med572000635641
- A.JohannessenS.LehmannE.R.Omenaaset alPost-bronchodilator spirometry reference values in adults and implications for disease managementAm J Respir Crit Care Med173200613161325
- H.TangZ.FangY.Sunet alYKL-40 in asthmatic patients, and its correlations with exacerbation, eosinophils and immunoglobulin EEur Respir J352010757760
- E.RaziG.A.MoosaviTotal serum IgE levels and total eosinophil counts: relationship with treatment response in patients with acute asthmaJ Bras Pneumol36120102328
- S.J.SzeflerB.R.PhillipsF.D.Martinezet alCharacterization of within-subject responses to fluticasone and montelukast in childhood asthmaJ Allergy Clin Immunol11522005233242
- J.SunyerJ.M.AntóJ.Sabriàet alRelationship between serum IgE and airway responsiveness in adults with asthmaJ Allergy Clin Immunol9531995699706
- B.BurrowsF.D.MartinezM.Halonenet alAssociation of asthma with serum IgE levels and skin-test reactivity to allergensN Engl J Med32051989271277
- K.M.BeehM.KsollR.BuhlElevation of total serum immunoglobulin E is associated with asthma in nonallergic individualsEur Respir J1642000609614
- D.J.TollerudG.T.O’ConnorD.Sparrowet alAsthma, hay fever, and phlegm production associated with distinct patterns of allergy skin test reactivity, eosinophilia, and serum IgE levels. The normative aging studyAm Rev Respir Dis14441991776781
- R.De MarcoA.MarconD.Jarviset alPrognostic factors of asthma severity: a 9-year international prospective cohort studyJ Allergy Clin Immunol1176200612491256
- L.BorishB.ChippsY.Denizet alTotal serum IgE levels in a large cohort of patients with severe or difficult-to-treat asthmaAnn Allergy Asthma Immunol9532005247253
- C.HaneneL.JiheneA.Jamelet alAssociation of GST genes polymorphism with asthma in Tunisian childrenMediators of Inflamm2007200719564 [Hindawi Publishing Corporation]
- T.E.IvaschenkoO.G.SidelevaV.S.BaranovGlutathione-S-transferase μ and theta gene polymorphism as new risk factors of atopic bronchial asthmaJ Mol Med80120023943
- M.B.FreidinE.I.BraginaL.M.Ogorodovaet alPolymorphism of the theta1 and mu1 glutathione S-transferase genes (GSTT1, GSTM1) in patients with atopic bronchial asthma from the West Siberian regionMolekulyarnaya Biologiya3642002630634
- T.R.RebbeckMolecular epidemiology of the human glutathione S-transferase genotypes GSTM1 and GSTT1 in cancer susceptibilityCancer Epidemiol Biomarkers Prev691997733743
- M.StanullaM.SchrappeA.M.Brechlinet alPolymorphism within glutathione S-transferase genes (GSTM1, GSTT1, GSTP1) and risk of relapse in childhood B-cell precursor acute lymphoblastic leukemia: a case-control studyBlood954200012221228
- A.J.SandfordH.W.ChanG.W.K.Wonget alCandidate genetic polymorphism for asthma in Chinese schoolchildren from Hong KongInt J Tuberc Lung Dis852004519527
- S.BenhamouW.J.LeeA.K.Alexandrieet alMeta-and pooled analyses of the effects of glutathione S-transferase M1 polymorphism and smoking on lung cancer riskCarcinogenesis238200213431350
- C.Brasch-AndersenL.ChristiansenQ.Tanet alPossible gene dosage effect of glutathione-S-transferases on atopic asthma: using real-time PCR for quantification of GSTM1 and GSTT1 gene copy numbersHum Mutat2432004208214
- S.I.HamdyM.HiratsukaK.Naraharaet alGenotype and allele frequencies of TPMT, NAT2, GST, SULT1A1 and MDR-1 in the Egyptian populationBr J Clin Pharmacol5562003560569
- A.A.SaadH.S.KassemS.S.BessaStudy of genetic predisposition in Egyptian colorectal cancer patients: Role of phase II xenobiotic metabolizing genes polymorphismAlex Medicam J4842006586599
- M.SaadatM.Ansari-LariGenetic polymorphism of glutathione S-transferase T1, M1 and asthma, a meta-analysis of the literaturePak J Biol Sci1023200741834189
- C.MinelliR.GranellR.Newsonet alGlutathione-S-transferase genes and asthma phenotypes: a Human Genome Epidemiology (HuGE) systematic review and meta-analysis including unpublished dataInt J Epidemiol3922010539562
- M.KhadadahB.O.OnadekoC.I.Ezeamuzieet alThe association of skin test reactivity, total serum IgE levels, and peripheral blood eosinophilia with asthma in KuwaitJ Asthma3762000481488
- D.L.SherrillM.D.LebowitzM.Halonenet alLongitudinal evaluation of the association between pulmonary function and total serum IgEAm J Respir Crit Care Med1521199598102
- N.EndohM.IchinoseT.Takahashiet alRelationship between cholinergic airway tone and serum immunoglobulin E in human subjectsEur Respir J12119987174
- M.NaqviS.ChoudhryH.J.Tsaiet alAssociation between IgE levels and asthma severity among African American, Mexican, and Puerto Rican patients with asthmaJ Allergy Clin Immunol12012007137143