Abstract
Introduction
Essential hyperhidrosis is an idiopathic condition characterized by markedly excessive sweating especially in the hands.
Objective
This study was done to evaluate the functional results of radiofrequency thermocoagulation of T2 ganglion in 10 patients suffered from essential hyperhidrosis of both upper limbs.
Methods
This retrospective study was carried out on 10 patients suffered from essential hyperhidrosis of both upper limbs. The male to female ratio was 2 to 3 (4 males and 6 females) and their ages ranged from 16 to 28 years. Simultaneous palmar and plantar sweating was present in five patients (50%), simultaneous palmar and craniofacial hyperhidrosis in two patients (20%), and simultaneous palmar and axillary hyperhidrosis in one patient (10%), while palmar hyperhidrosis alone was found only in two patients (20%). All cases underwent surgery in the form of radiofrequency thermocoagulation (RFT) of T2 on both sides under local anesthesia and sedation using C-arm radiological guidance. Mean postoperative follow up examination period was 24 months.
Results
There was no operative mortality. Pneumothorax occurred on left side in one patient. Transient partial Horner's syndrome occurred on the right side in another patient. Postoperatively, 9 patients (90%) had clinical improvement of their palmar sweating. The last patient had partial improvement on right side and no improvement on the left side. The operation was repeated in one case with recurrence on the right side who improved. At the last follow up, excellent results were obtained in 90% of limbs, fair results in 5% of limbs, and poor results in 5% of limbs.
Conclusion
The results of this study indicate that second thoracic ganglionectomy and sympathectomy performed with the use of percutaneous RFT is a very effective treatment for palmar hyperhidrosis that provide excellent immediate and long-term results as well as a low complication rate.
1 Introduction
Essential hyperhidrosis is characterized by excessive eccrine sweating (watery and nonodorous) beyond that required for cooling and sufficiently heavy so as to be considered an impairment of good health.Citation1,Citation2 The excessive sweating most commonly involves the hands or a combination of the hands and feet. Axilla is not uncommonly involved as well. Facial sweating can occur as a relatively isolated phenomenon or as part of the palmar plus plantar presentation, and occasional patients experience excessive sweating over the trunk as well.Citation3 In 70% of patients, the onset of excessive sweating is noted in infancy, but 20% note the onset in adolescence.Citation4
The congenital variant has a slight female predominance. Perhaps 25% of patients may have one or more involved close relatives, warranting the designation of this as a familial variant. Those with a familial variant seem to be more likely to experience widespread excessive sweating and may be at higher risk of developing compensatory hyperhidrosis after surgery.Citation1,Citation5
Essential hyperhidrosis seems to be especially prevalent in Taiwan and Israel, where the familial variant seems to be more common than elsewhere, but the disorder is encountered worldwide.Citation6
The condition can present both an occupational and a social handicap to affected person. The diagnosis is easily made by history and examination of the patient.Citation7 Although mild cases can be treated with drying agents or anticholinergic drugs, severe cases are usually resistant to conservative treatment and the most effective permanent treatment is surgical sympathectomy.Citation8 Opinions differ regarding the extent of sympathectomy. Recent experience has demonstrated that complete sympathetic denervation of upper limbs can be achieved by removal of the second thoracic ganglion alone.Citation9,Citation10
The aim of this work was to evaluate the functional results of radiofrequency thermocoagulation of second thoracic ganglion in 10 patients suffered from essential hyperhidrosis of upper limbs and to compare these results with the results of the other authors reported in the literature.
2 Methods
This retrospective study was carried out on 10 patients suffered from essential hyperhidrosis of both upper limbs. This study was done in Alexandria hospitals over a period of 3 years starting from January 2006 to December 2008. The male to female ratio was 2 to 3 (4 males and 6 females) and their ages ranged from 16 to 28 years with mean age of 21 years.
Simultaneous palmar and plantar hyperhidrosis was present in 5 patients (50%), simultaneous palmar and craniofacial hyperhidrosis in 2 patients (20%), and simultaneous palmar and axillary hyperhidrosis in 1 patient (10%), while palmar hyperhidrosis alone was found only in 2 patients (20%) ().
Table 1 Extent of hyperhidrosis, extent of RFT and outcome of cases.
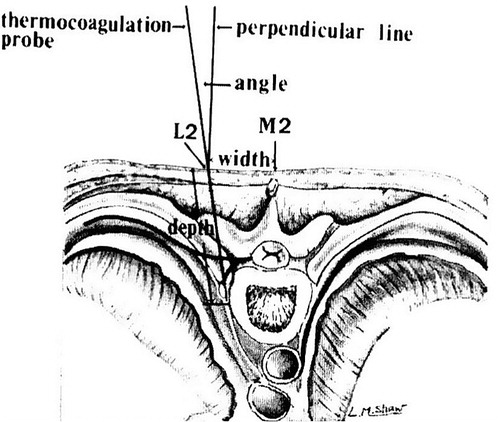
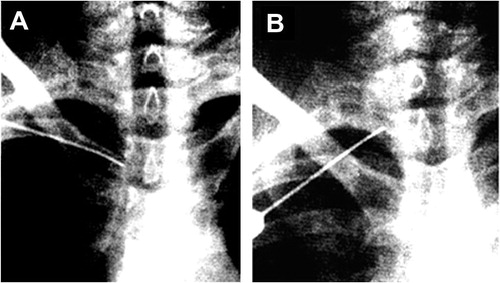
All cases underwent surgery in the form of radiofrequency thermocoagulation (RFT) of second thoracic ganglion on both sides under local anesthesia and sedation using C-arm radiological guidance. Only in 1 patient with hyperhidrosis of palm and axilla an additional RFT of T3 ganglion was done. The patient was positioned prone on the operating table. The site of needle puncture was 3 cm lateral from the midline of the base of the spinous process of the second thoracic vertebra. The needle was introduced through the second intercostal space. The angle of orientation was 101° from the horizontal plane and directed medially towards the midline. The depth of penetration was approximately from 6 to 6.5 cm (). Under C-arm radiological control we checked the optimal position of the needle relative to the second thoracic vertebra both in P–A and lateral views.( and ). On P–A view the needle was positioned first 2–5 mm adjacent to T2–T3 vertebral interspace, then repositioned 2–5 mm adjacent to the mid to rostral portion of the body of T2 beneath the head of the second rib. On lateral radiological view the tip of the needle was at the middle of the body of the second thoracic vertebra. The generator of radiofrequency used was RFG-3C from Radionics. Before lesion making, low voltage stimulation of 0, 1–0, 5 V at 50–75 Hz, for 1 min duration was done and the patient was observed for radicular pain or development of Horner’s syndrome. An increase in hand temperature during stimulation was a good sign that the electrode in a good position.
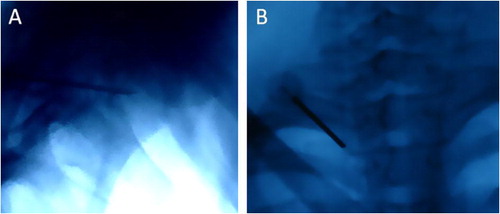
The straight temperature monitoring electrode (10 mm tip length) was used to perform an initial lesion at 80–90 °C for 180 s for each location, then the lesion was repeated at the same temperature and duration after withdrawal the electrode by 0.5 cm in each location. A flush and sweating was usually noted in the hand during stimulation due to cutaneous vasodilatation (). After the completion of RFT the hand was dry and flushed ().
Postoperative follow up examination period ranged from 1 to 3 years with a mean of 2 years.
3 Results
The operation was performed on both sides for all 10 patients on the same setting. 18 sides were operated for RFT of T2 ganglion while two sides in 1 patient with simultaneous palmar and axillary hyperhidrosis were operated for T2 and T3 ganglion.
3.1 Technical success
RFT was technically successful (completed) in all cases. If the patients could not localize or quantify the lesion during the procedure we could successfully complete the procedure on the basis of observation of palmar hyperemia in the affected side or by using radiological guidance.
3.2 Postoperative morbidity and mortality
There was no operative mortality. Pneumothorax occurred on left side in one patient Transient partial Horner’s syndrome occurred on the right side in another patient (loss of ciliospinal reflex and miosis). Compensatory hyperhidrosis occurred in on patient with preoperative hyperhidrosis in all his body that responded well to anticholinergic drugs.
3.3 Outcome of cases
All the patients had immediate initial relief of sweating. Follow up of the patients was done at one month, three months, and thereafter each 6 months. The evaluation was done clinically. The patients were classified into 3 groups according to their results. Group1: excellent results: complete relief of sweating, Group 2: fair results: partial relief of sweating, Group 3: poor results: no improvement of sweating. Postoperatively, excellent results were obtained in 90% of sides, fair results in 5% of sides, and poor results in 5% of sides.
Before treatment, simultaneous palmar and plantar sweating was present in 5 patients (50%). After treatment, 20% of these patients had dramatic improvement in their plantar hyperhidrosis, 40% had decreased plantar hyperhidrosis, and another 40% of patients had no improvement or a slight increase in their plantar hyperhidrosis. The 2 patients with simultaneous palmar and facial had excellent results as regard both palmar and facial hyperhidrosis. The patient with simultaneous palmar and axillary hyperhidrosis had excellent improvement as regards both palmar and axillary hyperhidrosis after RFT of T2 and T3 ganglia ().
3.4 Recurrence
Recurrence occurred in 1 patient on the right side (5%) after 12 months. Another radiofrequency lesion of the T2 ganglion was done in this case with recurrence. This patient improved and had excellent results after the second RFT. Summary data and outcome of these 10 patients are listed in .
Table 2 Summary data of 10 patients with essential hyperhidrosis who underwent RFT of T2 ganglion.
4 Discussion
The sympathetic supply of the upper limb is derived from the upper thoracic segments of the spinal cord from T2 to T6. These fibers are distributed up the sympathetic trunk and mainly via the cervicothoracic (stellate) ganglion to the brachial plexus and arteries of the upper limb. They innervate all sweat glands, erector muscles of the hairs and the muscular walls of the blood vessels.Citation11
Thoracic sympathectomy has been found to be of value in the treatment of certain pain syndromes, vascular disorders, and hyperhidrosis affecting the upper extremities.Citation12 Hyperhidrosis of the upper extremity is one of the most common indications for thoracic sympathectomy.Citation13–Citation17 Hyperhidrosis can be a source of great embarrassment and considerable disability to the patient. It may involve the entire body, including the legs and head, but symptoms are most severe and of the greatest discomfort in the upper extremities .The patients have symptoms that often date from childhood or early adolescence. Such individuals repot reluctance to shake hands or touch other people, and often wear gloves to disguise their condition.Citation15 The diagnosis is readily confirmed by inspection of the extremities.Citation16 Before surgery is considered for hyperhidrosis, all non surgical options should be tried. Also it is important to rule out other disorders such as thyrotoxicosis, pheochromocytoma and carcinoid syndrome as causes of excessive sweating.Citation17 In this study, all patients had their symptoms dated since early adolescence. Also, in this study, the reasons for seeking treatment included job-related inconvenience (e.g., writing, painting, fine manual work) in 6 cases (60%), inconvenience in practical daily tasks (e.g., loose grip of objects) in two cases (20%) and psychological hindrance (e.g., sense of inferiority or embarrassment) in two cases (20%). Patients with hyperhidrosis had previously tried non surgical treatments, which turned out to be ineffective.
The use of transthoracic electrocoagulation for the treatment of essential hyperhidrosis was first described by Malone et al.Citation14 The aim of this operation is to denervate the sympathetic supply to the upper limb without interfering with the stellate ganglion which supplies the head and neck. Division of the afferent or efferent fibers of the stellate ganglion will lead to Horner's syndrome.Citation18 Recent clinical and laboratory findings indicate that T2 ganglionectomy is likely sufficient to treat palmar hyperhidrosis. If the hyperhidrosis includes the axilla, the T3 and possibly T4 ganglia should be thermocoagulated as well. Also the surgical intent was not to eliminate all sweating from their hands, because this tended to substitute undesirable excessive dryness and skin cracking for the excessive sweating.Citation9,Citation10
The radiofrequency lesion has been claimed to be the most effective and widely used method for localized therapeutic destruction of neural tissue. The basic principle for radiofrequency ablation of a sympathetic lesion involves accuracy and precision. Sensory electrical stimulation occasionally elicits either a vague sensation or pain at the target area. Motor stimulation usually serves as an indicator of sufficient distance from the ventral root. To maximize the probability of success, the radiofrequency electrode must be located as close to the sympathetic ganglion as possible.Citation19,Citation20
In 1984, a percutaneous, X-ray guided radiofrequency technique devised by WilkinsonCitation21 has proved to be quite effective and safe for upper thoracic sympathectomy. In his series, the operation was conducted according to an expected anatomical location of the upper thoracic ganglia lying in the retropleural space.
In 1988, Chuang et al.Citation22 reported a stereotactic procedure for percutaneous RFT of upper thoracic ganglion in 10 cases with palmar hyperhidrosis. In their results they reported the real anatomical relationship between the second thoracic sympathetic ganglia and the tip of thermocoagulation probe that was revealed in cadaver studies and was adopted for thermocoagulation in a living human body. According to their study, the average size of the T2 ganglion in Chinese people is 9.8 mm in length, 7.4 in width, and 2.8 mm in thickness. They used a thermal probe with a 10-mm tip, that was applied to the T2 orT3 ganglion for 6 min at 85–90 °C in 10 patients with palmar hyperhidrosis that resulted in total neuronal death within the thoracic ganglia. They concluded that their technique should result in a better outcome compared to other methods, also it may be used to treat Buerger's disease, Raynaud's disease vasospasmic/sympathetic pain of the upper extremities.
According to the anatomical study of WilkinsonCitation23 in 1988, the T2 ganglion is situated roughly in the middle of the vertebrae rostro-caudally and 1/3 dorso-ventrally. Others have indicated that approximately 90% of the T2 or T3 sympathetic trunks are located on the head of the corresponding rib.Citation24 Another study found that the second thoracic ganglion is usually located (in 92.5% of patients) in the second intercostal space at the level of the intervertebral disc, between the second and the third thoracic vertebrae.Citation25
Although a variation of 1–1.5 cm of exact anatomical position is not of great importance during a surgical sympathectomy, it is critical during radiofrequency electrode placement. Therefore, multiple radiofrequency lesions were done.Citation26 In this study three dimensional system of coordinates described by Chuang et al. was applied, also a thermal probe with a 10-mm tip, that was applied to the T2 orT3 ganglion for 9–12 min at 85–90 °C on each side of 10 patients with palmar hyperhidrosis. In this study an average of three lesions for 9 min duration were done on each side of the 10 patients.
Before anesthesia, during the introduction of the needle, patients were asked to take a light breath and to tell the doctor if they felt like coughing. The needle was elevated immediately when signs of pneumothorax (i.e., coughing, sensation of a need to cough) were suspected or were reported by the patient. In this study this occurred in 1 patient who developed Pneumothorax on the left side postoperatively.
During the procedure, palm skin temperature measurement was used to demonstrate sympathetic denervation. Other previous studies reported that the T2 sympathetic ganglion determines palm skin temperature in patients with essential palmar hyperhidrosis.Citation9,Citation10
After the procedure, patients are out of bed and fully active and can be discharged on the same operative day.
Chuang et al.Citation27 reported final success rate of 99.9% in their series of 1742 (1688 palmar + 54 facial) hyperhidrotic patients with the use of this technique of ganglionectomy and sympathectomy. The facial innervation ascending from the T2 ganglion may be responsible for the effectiveness of T2 lesioning in patients with facial hyperhidrosis. In their study during a long-term follow-up assessment ranging from 1 to 8 years, recurrence had developed in 268 sides, and retreatment was successful in all of these sides. This result was similar to the final success rate that Rex et al.Citation28 reported in 1152 cases. The final cure rate using this percutaneous technique is higher than that described in reports in which other methods were used. The postoperative complication rates of 0.2% for pneumothorax and 0.15% for partial Horner's syndrome are very low. In this study the final success rate was 99, 5% and postoperative complication rate 5% for pneumothorax and 5% of partial Horner's syndrome. All of these patients returned to normal within 6 months. Also, open surgical removal of T2 and T3 ganglia produced many postoperative complications, such as pneumothorax, Horner's syndrome, intercostal artery bleeding, gustatory sweating, and paravertebral muscular atrophy.Citation27,Citation28
Chuang et al.Citation27 reported that most patients with palmar hyperhidrosis also have sole hyperhidrosis which is problematic. After the use of the same technique for the control of palmar and craniofacial hyperhidrosis, however, they found that 24% of plantar hyperhidrosis improved dramatically, 68% of plantar hyperhidrosis improved partially, and only 8% plantar hyperhidrosis did not improve or became worse. Thus, they reported a dramatic or partial improvement was achieved in 92% of patients. This result is similar to the success rate of Lin et al.Citation29 but still higher than the 23.3–44% rate of improvement reported in other studies.Citation30–Citation32
In this study, before treatment, simultaneous palmar and plantar sweating was present in five patients 50% of patients. After treatment, 20% of these patients had dramatic improvement in plantar hyperhidrosis, 40% had decreased plantar hyperhidrosis, and anther 40% of patients had no improvement or a slight increase in their plantar hyperhidrosis.
It is well established that compensatory hyperhidrosis often occurs after thoracic sympathectomy.Citation33 The extent of compensatory hyperhidrosis in the present study was not assed, however, because this was not the original purpose for the study, and an adequate analysis would have required additional planning and follow-up that would have exceeded the scope of this study. The pathologic form of compensatory hyperhidrosis (excessive sweating over the trunk, inguinal area, or face severe and persistent enough even at rest or in a cool environment) is considered a significant complication. It seems to develop in patients with the familial type of the disease or with wide spread areas of heavy sweating before surgery.Citation34 In this study one case (10%) developed compensatory hyperhidrosis, but the pathological form did not occurred.
Although the number of cases in which this procedure has been used was small, the procedure offers such a major advance over presently available alternative open surgical techniques that presentation seems warranted. This technique is effective, safe, has fewer side effects, and is certainly easier with less cost effective than presently available surgical alternative. This is especially true for patients who require bilateral sympathectomy. Patients no longer need to be hospitalized and to undergo a major surgical intervention under general anesthesia to achieve satisfactory thoracic sympathectomy The ability to achieve sympathectomy without the need for general anesthesia and major surgical intervention is especially important for patients with hyperhidrosis, whose disease is not considered life-endangering, and for patients who are candidates for sympathectomy because of cardiac problems but who may be poor surgical risks.Citation22,Citation35 Because of few complications and a high success rate, it should be considered an attractive first-line alternative in the management of severe hyperhidrosis.Citation27,Citation36
5 Conclusion
The results of this study indicate that second thoracic ganglionectomy and sympathectomy performed with the use of percutaneous RFT is a very effective treatment for palmar and craniofacial hyperhidrosis that provide excellent immediate and long-term results as well as a low complication rate. The technique is safe, has fewer side effects, and is certainly easier with less cost effect than other surgical alternative. The technique is also effective as a retreatment for recurrences.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine
References
- P.S.MaloneA.E.P.CameronJ.A.RennieThe surgical treatment of upper limb hyperhidrosisBr J Dermatol11519868184
- P.J.GoluekeW.V.GarrettJ.E.ThomosonDorsal sympathectomy for hyperhidrosis: the posterior paravertebral approachSurgery1031988568572
- Z.CohenI.LeviI.PinskThoracoscopic upper thoracic sympathectomy for primary palmar hyperhidrosis: the combined pediatric, adolescents and adult experienceEur J Surg Suppl580199858
- A.D.FoxL.HandsJ.CollinThe results of thoracoscopic sympathetic trunk transection for palmar hyperhidrosis and sympathetic ganglionectomy for axillary hyperhidrosisEur J Vasc Endovasc Surg171999343346
- A.N.GrahamW.A.OwensJ.A.McGuiganAssessment of outcome after thoracoscopic sympathectomy for hyperhidrosis in a specialized unitJ R Coll Surg Edinb411996160163
- M.C.KaoLaser endoscopic sympathectomy for palmar hyperhidrosisLasers Surg Med121992308312
- C.J.ShihM.T.LinThermoregulatory sweating in palmar hyperhidrosis before and after upper thoracic sympathectomyJ Neurosurg5019798894
- R.W. Hardy, J.W. Bay, Surgery of the sympathetic nervous system. I: H.H. Schmidek, W.H. Sweet (Eds.), Operative neurosurgical techniques, Vol New York, Grune et Stratton, 1988, pp. 1271–1280.
- D.S.O’ RiordainM.MaherD.J.WaldronLimiting the anatomic extent of upper thoracic sympathectomy for primary palmar hyperhidrosisSurg Gynecol Obstet1761993151154
- D.A.HerzJ.E.LoomanR.D.FordSecond thoracic sympathetic ganglionectomy in sympathectically maintained painJ Pain Symptom Mgt81993483491
- A.MastersJ.A.RennieEndoscopic transthoracic sympathectomy for idiopathic upper limb hyperhidrosisClin Auton Res21992349352
- F.E.WealeUpper thoracic sympathectomy by transthoracic electrocoagulationBr J Surg6719807172
- J.ByrneT.N.WalshW.P.HedermanEndoscopic transthoracic electrocautery of the sympathetic chain for palmar and axillary hyperhidrosisBr J Surg77199010461049
- P.S.MaloneJ.P.DuignanW.P.HedermanTransthoracic electrocoagulation (T.T.E.C.)–a new and simple approach to upper limb sympathectomyIr Med J7519822021
- D.ChuP.K.ShiC.M.WuTransthoracic endoscopic sympathectomy for treatment of hyperhidrosis palmarisKaohsiung J Med Sci131997162168
- A.BassS.InovrotzlavskiR.AdarUpper dorsal sympathectomy for palmar hyperhidrosisIsr J Med Sci191983112115
- A.J.MaresZ.SteinerZ.CohenTransaxillary upper thoracic sympathectomy for primary palmar hyperhidrosis in children and adolescentsJ Pediatr Surg291994382386
- A.GordonK.ZechmeisterJ.CollinThe role of sympathectomy in current surgical practiceEur J Vasc Surg81994129137
- D.J.HehirM.P.BradyLong-term results of limited thoracic sympathectomy for palmar hyperhidrosisJ Pediatr Surg281993909911
- J.W.BayD.F.DohnSurgical sympathectomyR.H.WilkinsS.S.RengacharyNeurosurgeryvol 21985McGraw-HillNew York19121917
- H.A.WilkinsonPercutaneous radiofrequency upper thoracic sympathectomy: a new techniqueNeurosurgery151984811814
- K.S.ChuangN.H.LiouJ.C.LiuNew stereotactic technique for percutaneous thermocoagulation upper thoracic ganglionectomy in cases of palmar hyperhidrosisNeurosurgery221988600604
- H.A.WilkinsonR.W.HardyNew stereotactic technique for percutaneous thermocoagulation upper thoracic ganglionectomy in cases of palmar hyperhidrosisNeurosurgery221988603604
- J.L.YarzebskiH.A.WilkinsonT2 and T3 sympathetic ganglia in the adult human: a cadaver and clinical–radiologic study and its clinical applicationNeurosurgery211987339342
- S.RengacharyT2 and T3 sympathetic ganglia in the adult human: A cadaver and clinical-radiographic study and its clinical applicationNeurosurgery211987342
- M.HashmonaiD.KopelmanO.KeinUpper thoracic sympathectomy for primary palmar hyperhidrosis: long-term follow-upBr J Surg791992268271
- K.S.ChuangJ.C.LiuLong-term Assessment of Percutaneous Stereotactic Thermocoagulation of Upper Thoracic Ganglionectomy and Sympathectomy for Palmar and Craniofacial Hyperhidrosis in 1742 CasesNeurosurgery5142002963970
- L.O.RexC.DrottG.ClaesThe Boras experience of endoscopic thoracic sympathicotomy for palmar, axillary, facial hyperhidrosis and facial blushingEur J Surg Suppl58019982326
- C.L.LinC.P.YenS.L.HowngThe long-term results of upper dorsal sympathetic ganglionectomy and endoscopic thoracic sympathectomy for palmar hyperhidrosisSurg Today291999209213
- F.GjerrisH.P.OlesenPalmar hyperhidrosis: long-term results following high thoracic sympathectomyActa Neurol Scand511975167172
- R.AdarSurgical treatment of palmar hyperhidrosis before thoracoscopy: experience with 475 patientsEur J Surg Suppl5721994911
- C.J.ShihY.C.WangThoracic sympathectomy for palmar hyperhidrosis: report of 457 casesSurg Neurol101978291296
- R.AdarCompensatory sweating after upper dorsal sympathectomyJ Neurosurg511979424425
- H.A.WilkinsonPercutaneous radiofrequency upper thoracic sympathectomyNeurosurgery381996715725
- K.K.TanSympathectomy for wet dripping palmsSingapore Med J321991119120
- A.LucasY.RollandN.JourneauxComputed tomography guided thoracic sympatholysis for palmar hyperhidrosisJ Cardiovasc Surg (Torino)391998387389

