Abstract
Background
A growing interest has become increasing in the role of physicians as effective resources for the promotion of good nutritional practices, however, the factors that impede their nutritional counseling and management practice (NC&M) are not clearly understood in Saudi Arabia.
Objectives
The objectives of the study were to investigate physicians’ practices concerning NC&M and to explore some determinants that predict such practices.
Results
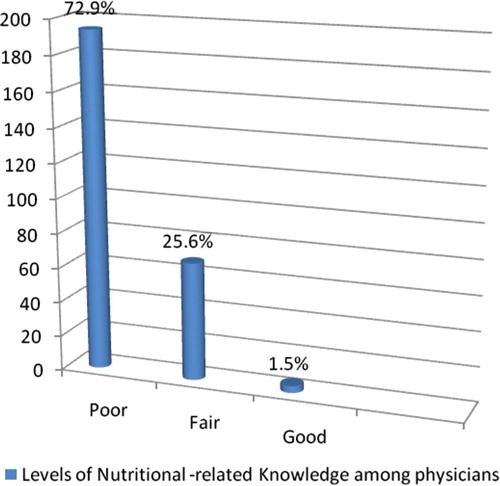
Data of 266 physicians working in big hospitals in Riyadh showed that only 7.9% of the respondents reported that they were practicing all aspects of NC&M; including nutritional assessment, therapy, and education. Those who practiced any one of these aspects ranged between 13.9–40.2%, meanwhile, 28% frankly reported that they did not practice NC&M. In the last year, the mean percentage of patients placed on nutrition therapy was 24.15 ± 27.78% and the mean percentage of clinic time dedicated to NC&M was 21.49 ± 20.54%. Most of the respondents (72.9%) had poor nutritional knowledge score. Overall, 19.2% previously attended CME in nutrition. Only 1.5% and 28.6% self-assessed themselves as “outstanding” and “good” in NC&M skills and the mean total self-efficacy in NC&M was moderate. The majority (77.8%) perceived NC&M as highly or moderately relevant to their specialties. Physicians attitude and perceived efficacy towards NC&M was moderately high as the mean scores were greater than their midpoint. Their perceived barriers of NC&M were considerably moderate; as the mean total score was found to be near the midpoint of that scale. Among the seven independent variables entered the binary logistic regression of physicians practice of NC&M, only the knowledge, attitude, and self-efficacy scores were significantly associated with their NC&M practice. These three predictors contributed by 23.5% of the variation of physician practice of NC&M.
Conclusions
Physicians knowledge, self-efficacy, attitudes and other factors should be stressed in any intervention warranted to improve their nutritional practices.
1 Introduction
Since 1950s the link between diet and chronic diseases such as obesity, cancer, cardiovascular diseases, diabetes, gall stones has been increasingly well recognized worldwide.Citation1 Over the past three decades Saudi Arabia has witnessed a remarkable lifestyle changes towards urbanization with accompanying nutrition transition of its population where customary and traditional food is being replaced by fast food high in fat, sugar and salt. This is happening along with sedentary lifestyle and reduced physical activity.Citation2 Consequently, the prevalence and costs of health conditions associated with excess weight continue to rise in alarming rates.Citation3 Therefore, efforts to treat and prevent these conditions have become increasingly important with a growing interest in the role of health service providers as resources for the promotion of good nutritional practices. Dietary and physical activity changes are needed not only to tackle poor and over nutrition but also to prevent and treat many of the chronic diseases that rise in epidemic proportions.Citation4–Citation6
Demonstrating the effectiveness of nutrition counseling is imperative, not only to promote successful patient outcomes but also to secure funding.Citation5 Physicians are considered as the most credible source of medical information as well the best in their ability to motivate patients to make healthy lifestyle decisions.Citation6 The credibility that physicians are typically accorded in many social settings suggests that nutrition advice delivered by practitioners may particularly persuasive. A study in Brazil demonstrated that trained health care providers were more likely to engage in nutrition counseling (P < 0.013) and to deliver more extensive advice (P < 0.02). They also used communication skills designed to improve rapport and ensure that clients understood the advice (P < 0.01).Citation7
However, nutritional practice in hospitals has low priority.Citation8 Previous surveys have shown that there is a disparity between physicians’ beliefs about the importance of diet and nutrition in health maintenance and disease prevention and the actual delivery of nutrition counseling.Citation9–Citation12 Warner et al.Citation13 reported that physicians are better able to identify obesity and its associated health risks, but some negative stereotypical attitudes persist. Jay et al.Citation14 found that more than 40% of physicians had a negative reaction towards obese patients, 56% felt qualified to treat obesity, and 46% felt successful in this realm. These negative attitudes affect current treatment practices and patient care. Doctors are reluctant to address weight management issues especially among those who are not extremely overweight.Citation15 Physicians may not be also adequate role models for promoting healthy eating and exercise adherence.Citation16
Published studies delineated many substantial constrains that prevent physicians from providing dietary counseling. Physicians lack adequate time, knowledge, confidence (self-efficacy) and skills to provide effective nutritional counseling and management.Citation17 Also a variety of characteristics of health service management such as lack of training, lack of incentives, heavy demand relative to personnel, the separation of preventive and curative services – all may impede the provision of sustained nutrition intervention.Citation7
Despite the growing epidemic of obesity and overweight in Saudi Arabia, weight management is not adequately addressed and many of the above mentioned constrains can be observed to hinder adequate nutrition and exercise counseling and management. Al-NumairCitation18 assessed nutritional knowledge of 59 primary health care physicians and reported that the mean mark of correctly answered questions was 51.7 ± 14.35%. Moreover, there is a paucity of research tackling in depth physicians’ nutritional counseling and management practice, attitudes, knowledge and beliefs. Understanding these perceptions will help identify continuous medical education (CME) training needs of physicians. This will guide tailoring an effective CME program about nutritional counseling and management that could be integrated into routine medical care.
Therefore, this study aimed to investigate physicians’ practices concerning NC&M and to explore some determinants that predict such practices. Addressing such areas would help ensure strengthening the skills of physicians in providing quality counseling and therapeutic education for nutritional problems and weight maintenance with concomitant quality improvement across the health care delivery system in Saudi Arabia.
2 Methods
2.1 Study design and setting
A cross-sectional descriptive study was conducted in five big hospitals that represented different health institutions in Riyadh City, Saudi Arabia, during the period January through April 2010. Seven departments were randomly chosen from the prepared list of NC&M-related departments for each hospital (each hospital has its own classification for its departments). The chosen departments were providing care in different specialties including gastroenterology, cardiology, oncology, respiratory disorders, primary care, home care, diabetes center/clinic, obstetrics and gynecology and ophthalmology. Five hundred survey questionnaires were distributed to all physicians in those departments who were consented for their personal approval to participate in the study. Only those who agreed (307) were included in the study with response rate 61.4%. Forty one questionnaires were excluded due to incomplete answers, giving a final total of 266 valid responses. The study was approved by the research ethics committee at the author's institution.
2.2 Tool of the study
A self-administered structured questionnaire was developed. Its content validity was confirmed through an extensive literature review and experts specialized in clinical nutrition, public health and behavioral sciences. It included data about:
2.2.1 Personal data
This included data such as sex, years of experience, nationality, specialty.
2.2.2 CME data about NC&M
This included physicians’ previous training, perceived needs of further training in NC&M, and preferred sources to get information about NC&M.
2.2.3 Perceived relevancy to specialty, benefits and utility, barriers of NC&M
This was measured in terms of a statement entailing the perceived relevancy of NC&M to their work, eight statements revealing to what extent physicians believe in their role (within their specialty) in promoting healthy nutrition, the utility and efficacy of NC&M, in addition to seven statements assessing their perceived barriers toward NC&M. All statements are stated as five points Likert scale where each statement was scored from 1 to 5 with higher score for strong or higher perception.
2.2.4 NC&M practices and some related factors
Five questions were used to reveal their NC&M practice, time devoted in NC&M, percentage of patients placed on nutritional therapy, issues discussed during NC&M, and different NC&M practices done during the visit. Also physicians were asked to self-assess their proficiency skills in NC&M.
2.2.5 Physicians’ nutritional knowledge
This scale comprised 22 questions (five were multiple choice and 3 were true/false/don't know answers) that examined general and specific nutritional knowledge regarding healthy food, its constituents, food pyramid, glycemic index, caloric value, nutritional recommendations. For each question the correct answer was given a score of one and incorrect answer was given zero. Blank responses were coded as wrong responses. All scores were summed as a total knowledge score which ranged from 0 to 22. This score was leveled into three levels; Poor which is <50% correct answers (0–11), Fair which is 51%- <75% correct answers (11.1–16) and Good which is 75% or more correct answers (16.1–22).
2.2.6 Physicians’ attitudes towards NC&M
A scale of 16 items was designed as five points Likert scale (strongly agree, agree, neutral, disagree, strongly disagree) to ascertain physicians’ attitude toward nutritional counseling and management. For each item, the response was scored from 1 to 5 with higher score for more favorable attitude toward NC&M. A total score was summed and ranged from 16 to 80).
2.2.7 Physicians’ self-efficacy beliefs about NC&M
Self-efficacy means physician's confidence in his ability to participate in NC&M in common/difficult situations. The scale used was designed after literature review and it was adapted from a published self-efficacy scale.Citation19 It included 13 common/difficult situations to assess physicians’ confidence in their ability to participate in NC&M (e.g., Counseling patients in the benefits of dieting and weight management, Identifying barriers to compliance with dietary regime in a patient, Providing a patient with a detailed exercise prescription). Each item was rated on a 10-point Likert scale ranging from 0 (not at all confident) to 10 (very confident). The total scale score can range from 0 to 130, with higher scores indicating stronger perceived self-efficacy in NC&M.
2.3 Statistical analysis
Data was processed and analyzed by SPSS, version 17. Descriptive statistics was used to describe the studied variables. For testing internal consistency of for the scales Chronbach reliability test was used and it was 0.95 for self-efficacy scale, 0.72 for attitude scale and 0.63 for knowledge scale. Binary logistic regression was used to determine the independent predictors of physicians’ practice of NC&M which was the dependent variable in the regression. Practice of NC&M was assumed as (1) and non-practice of NC&M was the lower reference category (0). Seven independent continuous predictors were entered the regression which included the main psychosocial constructs of physicians practice; total knowledge score, total attitude score, total self-efficacy score, total barriers score, total benefits score, in addition to two main personal data; years of experience (which reflect age and experience), and hours of previous training in NC&M. The level of significance used was at P value <0.05.
3 Results
3.1 Respondents’ demographics
Male physicians represent 53.8% of the respondents. Only 126 participants (47.4%) were Saudis, while only 36 physicians were non-Arabic speakers (13.5%). The mean years of experience of the respondents was 9.09 ± 6.8 years (range, 1–31 years). Half of the sample was working in Military hospitals, 45.5% were working in Ministry of health hospitals (General and Specialist) and 11.1% were from a university hospital. More than half of the respondents (56%) pursued postgraduate studies (fellowship; 30.5%, and others; 25.5%). One hundred and twelve respondents (42.1%) ranked in higher positions (such as consultants).
3.2 NC&M practice, skills and training among physicians
shows that only 28.2% of the respondents did not practice NC&M. In the last year, the mean percentage of patients placed on nutrition therapy 24.15 ± 27.78 and the mean percentage of clinic time dedicated to NC&M was 21.49 ± 20.54. Among those who were practicing NC&M, instructions (whether individual, group or handouts) were the most frequently mentioned practice (40.2%, 14.7%, 11.3%, respectively), while other aspects of NC&M; assessment and therapeutic plan were followed by only 13.9% and 15.4% of them. About the sort of nutritional advice given to patients, general information about healthy eating (52.3%) and disease specific instructions (40.9%) were cited on top of the list. Only 22.2% mentioned “dealing with weight management issues”. Overall, 51 respondents (19.2%) attended previously CME in nutrition. Only 1.5% and 28.6% of the respondents self-assessed themselves as “outstanding” and “good” in NC&M skills. The most frequently cited preferred sources of nutrition information were textbooks and Web (46.2% and 39.5%).
Table 1 Physicians practice, skills and training of NC&M.
3.3 PHC physicians’ knowledge, attitudes and perceptions about NC&M
delineates that most of the respondents (72.9%) have poor total knowledge score about nutrition, 25.6% have fair knowledge level and only 1.5% have good knowledge level. The mean total knowledge score was 8.76 + 3.36 with the actual range (0–22) and the estimated range (0.5–17.8).
As shown in , the mean score of physicians’ perceived relevancy of NC&M to their specialties (3.07) was moderately high as the range of the score was 1–4. Those who reported high perceived relevancy was (41%). Generally the physicians’ attitude towards NC&M was moderately high. This is clear from values of the lower limit of total attitude score’ range (35) and its mean (53.38 ± 7.34) where both were greater than the midpoint of that score (32.5). For different attitudinal statements, the mean scores of 11 out of 16 statements were above 3.35 (midpoint = 3, estimated range 1–5). However, the mean score of self-estimated physicians’ perceived proficiency in NM &C (2.03) was less than the midpoint of the scale (2.5); this indicates that they acknowledge that they are lacking the proficiency in NC&M. Again on the self-efficacy scale, the respondents’ self-efficacy in NC&M was moderate as their mean total self-efficacy score was 77.51 which was around the midpoint (65) of the actual range (0–130). Along the self-efficacy scale of (0–10), all statements scored from 5.44 to 6.79 indicating moderate self-efficacy about different NC&M skills.
Table 2 Physicians attitudes and perceptions regarding NC&M.
Concerning physicians’ perceptions of benefits of NC&M, indicates that the mean total perceived benefits score was high (32.49) which was a little bit near the maximum of the actual range of that score (8–40). On the other hand, their perceptions of the barriers that hinder the practice of NC&M were considerably moderate; as the mean total barriers score was found to be 25.61, which was slightly greater than midpoint (22.5) of the actual range (7-35). However, the most prominent barriers mentioned were lack of training, low priority given for nutrition management during physicians’ preparation in their undergraduate study and shortage of physician time.
3.4 Binary logistic regression of PHC physicians’ practice of NC&M with some independent variables
indicates that among the seven independent variables entered the regression, only three predictors were found to be significantly associated with physicians’ practice of NC&M. These were the total knowledge score, the total attitude score, and the total self-efficacy score. Physicians with higher knowledge, attitude, and self-efficacy total scores were more prone to practice NC&M. If there is one unit increase in each of the knowledge, attitude and self-efficacy scores, we expect about 16%, 21% and 4% increase in the NC&M practice (odd ratio was 1.158, 1.205 and 1.036 with 95% CI of 1.033–1.297, 1.014–1.431 and 1.011–1.061, respectively). These three predictors contributed by 23.5% of physician practice of NC&M (Cox & Snell's R square = 0.235).
Table 3 Binary logistic regression of the NC&M practice among physicians with some independent variables.
4 Discussion
Despite the potential for counseling to improve dietary practices, a broad review of literature suggests that the practice of NC&M among physicians is inadequate.Citation20–Citation22 The current study reveals similar findings where only 7.9% of the respondents reported that they were practicing all aspects of NC&M including nutritional assessment, therapy, and individual/group education. Some (13.9–40.2%) reported their practice to any one of the previously mentioned aspects, meanwhile, 28% frankly reported that they did not practice NC&M, and even 12% never gave any nutritional advice to their patients. The previously reported estimates of the percentage of patient consultations that include nutrition or weight counseling range from 14% to 50%.Citation20–Citation24
Although the low prevalence of such counseling among physicians, it is clearly obvious in this study that most of them had favorable attitude to NC&M as The total attitude score was 53.38 and the scale's midpoint 32.5. Also, most of the respondents were aware of the relevancy of NC&M to their specialties (78.2%) and believed in the importance of nutrition in preventing and treating common diseases in Saudi Arabia (Mean = 32.49, range 8–40). This is in consistence to Kushner study (1995) who reported that nearly three quarters of respondents feel dietary counseling is important and is the responsibility of physicians.Citation9 Kolasa and RickettCitation25 mentioned that the gap remains between the proportion of patients who physicians believe would benefit from nutrition counseling and those who receive it from their primary care physician or are referred to dietitians and other healthcare professionals. HelmanCitation26 concluded that the extent of nutrition counseling by GPs is considerably less than might be expected from the strength of their statements about the importance of nutrition and long-term health.
The reasons for the existing disparity between physicians′ attitudes, beliefs about the importance of nutrition in health maintenance and disease prevention and the actual delivery of nutrition counseling and management is not clear. One reason has been proven to exert a strong impact on human behavior and also on physician's practice behavior is self-efficacy.Citation19 Those with greater degrees of self-efficacy are more likely to engage in the behavior and persist in the face of obstacles. When physicians lack the confidence in their ability to assess, counsel and manage nutritional issues, even when they believe in its importance, they might be more hesitant to do so.Citation27 Similar to the findings of Mihalynuk et al.,Citation27 our study shows that the total mean self-efficacy score of the physicians was quietly moderate (77.51 & range 0–130). Furthermore, physicians’ self-perceived proficiency was also moderate; as fewer than one third of the physicians self-assessed themselves as outstanding and good (1.5% &28.6%, respectively) in NC&M skills. Consistently, Vetter et al.Citation28 reported that less than one third of the participants were confident in their ability to assess the nutritional status of patients or to discuss general nutritional issues. This lack of confidence may have important consequences; according to a popular behavioral theory,Citation19 Physicians who perceive themselves to be highly efficacious expect favorable outcomes.Citation29 Skilled physicians can serve as efficacy builders to their patients by diagnosing peoples’ strengths and weaknesses and cultivating a patient's belief in their own capabilities. However, physicians fail to do so if they themselves do not feel competent at conducting basic nutrition assessments or offering dietary advice.Citation30,Citation31 Key physician factors found to be associated with low self-efficacy are lack of training, lack of knowledge, and perceived barriers.Citation9 These factors might affect physicians’ practices directly or indirectly through their self-efficacy.
A broad review of the literature suggests that the nutrition training of physicians and many medical students is inadequate; our data suggest that the majority of the respondents never received special training in NC&M (80.8%) and had poor nutrition knowledge (72.9%). This is also in keeping with a U.S. Public Health Service study noting that physicians are “woefully undertrained in nutrition”.Citation32 Also, Spener et al.Citation33 mentioned that the training received by medical students in their study did not adequately address the requisite skills for real patient encounters. Similar to our findings, the degree of nutrition knowledge has been found to be low among physicians in practice.Citation34 A 2002 survey of 290 medical students reported that some students were lacking in knowledge about NC&M knowledge.Citation35 Acquisition of knowledge and skills enable a person to meet personal standards of merit that tend to heighten beliefs of personal efficacy.Citation30 Physicians training should not only focus on nutritional facts and knowledge but also should stresses on understanding of methods to improve a patient's nutrition status (e.g. ordering appropriate diets, referring patients to nutrition experts, providing a self-management prescription, among others). Bandura documented that influential mentors must be diagnosticians of peoples’ potentials and must be knowledgeable about how to modify activities so that potentiality can be turned into actuality.Citation30
Lack of knowledge and training are perceived as barriers in the present study. Physicians noted many barriers to counselling their patients that agree with previous studies that reported lack of knowledge, lack of counseling training, low physician confidence, inadequate teaching materials in addition to a lack of time, inadequate reimbursement and patient non-compliance, as main barriers to diet counselling.Citation36–Citation38
Our results implied that knowledge, attitude and self-efficacy were the most important significant predictors of physicians’ practice of NC&M which came in accordance with previous researchers.Citation39,Citation40 Therefore, a multifaceted approach will be needed for training physicians to change their NC&M behavior. An effective training program should not only intend to increase their awareness and superficial knowledge of nutrition but also should involve discussion of in depth knowledge, development of attitudes, management skills and building a robust sense of self-efficacy to support the exercise of control in the face of difficulties that inevitably arise.Citation41
Our study has several noteworthy limitations. Our results may have limited generalizablility to other populations of physicians in KSA, as all respondents in our study were from big hospitals in Riyadh city and also the self-reported nature of the study carries the risk of disclosure bias, yet it represents the opinions of physicians from different specialties in big hospitals representing different health sectors all over the city. Because the selection of the sample was based on physician willingness and the response rate of less than 61.4% raises the possibility of a significant response bias among physicians responding to the survey. As we did not evaluate a sample of non-responders to examine differences between responders and those who did not respond, the possibility of non-response bias remains. Our results should be interpreted cautiously and may not apply to all community based physicians especially the primary care physicians were not included in the study. Test fatigue due to the length of the questionnaire may have led to lower overall scores. Despite these drawbacks, the principal strength of our study was that it was the first, to our knowledge, to investigate the predictors of physicians practice in NC&M in our country and it corroborated previous findings of significant deficits in knowledge, training, self-efficacy, with low scores in self-perceived proficiency and moderate scores of perceived barriers.
In conclusion the study recommends launching innovative and effective methods for enhancing physician training about nutrition, starting from medical school. Further research should be undertaken to explore other factors influencing NC&M, and to replicate the study on physicians with primary health care.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 30 November 2011
References
- WHO. What are the health consequences of being overweight? Cited in 2011, may. Available from: <http://www.who.int/features/qa/49/en/index.html>.
- A.Al-NuaimE.A.BamgboyeK.Al-RubeaanY.Al-MazrouOverweight and obesity in Saudi Arabian adult population, role of sociodemographic variablesJ Commun Health2231997211223
- A.I.Al-OthaimeenAl-NozhaA.K.OsmanObesity: an emerging problem in Saudi Arabia. Analysis of data from the National Nutrition SurveyEast Med Health J1322007441448
- A.M.BelalNutrition-related chronic diseases Epidemic in UAE: can we stand to STOP it?Sudanese J Public Health442009383392
- S.L.CookR.NasserB.L.ComfortD.K.LarsenEffect of nutrition counselling on client perceptions and eating behaviourCan J Diet Pract Res6742006171177
- S.AbramsonJ.SteinM.SchaufeleE.FratesS.RoganPersonal exercise habits and counseling practices of primary care physicians: a national surveyClin J Sport Med10120004048
- G.H.PeltoI.SantosH.G.AlvesC.VictoraJ.MartinesJ.P.HabichNutrition counseling training changes physician behavior and improves caregiver knowledge acquisitionJ Nutr1342004357362
- M.MoweI.BosaeusH.H.RasmussenJ.KondrupM.UnossonØ.IrtunNutritional routines and attitudes among doctors and nurses in Scandinavia: a questionnaire based surveyClin Nutr2532006524532
- R.F.KushnerBarriers to providing nutrition counseling by physicians: a survey of primary care practitionersPrev Med2461995543545
- J.F.ThuanA.AvignonObesity management: attitudes and practices of French general practitioners in a region of FranceInt J Obes299200511001106
- J.M.FerranteA.K.PiaseckiP.A.Ohman-StricklandB.F.CrabtreeFamily physicians’ practices and attitudes regarding care of extremely obese patientsObesity179200917101716
- M.Van GerwenC.FrancS.RosmanM.Le VaillantN.Pelletier-FleuryPrimary care physicians’ knowledge, attitudes, beliefs and practices regarding childhood obesity: a systematic reviewObes Rev1022009227236
- C.H.WarnerC.M.WarnerJ.MorgansteinG.N.AppenzellerJ.RachalT.GriegerMilitary family physician attitudes toward treating obesityMil Med173102008978984
- M.JayA.KaletT.ArkM.McMackenM.J.MessitoR.RichterS.SchlairS.ShermanS.ZabarC.GillespiePhysicians’ attitudes about obesity and their associations with competency and specialty: a cross-sectional studyBMC Health Serv Res92009106
- G.D.FosterT.A.WaddenA.P.MarkrisD.DavidsonR.S.SandersonD.B.AllisonPrimary care physician’ attitudes about obesity and its treatmentObesity Res1110200311681177
- L.Q.RogersB.GutinM.C.HumphriesC.R.LemmonJ.L.WallerT.BaranowskiR.SaundersEvaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived successTeach Learn Med1832006215221
- S.BowermanM.BellmanP.SaltsmanD.GarveyK.PimstoneS.SkootskyH.J.WangR.ElashoffD.HeberImplementation of a Primary care physician network obesity management programObesity Res92001S321S325
- K.S.Al-NumairNutritional knowledge of primary care physicians in Saudi ArabiaPakistan J Nutr362004344347
- S.C.ThompsonL.SchwankovskyJ.PittsCounselling patients to make lifestyle changes: the role of physician self-efficacy, training and beliefs about causesFam Pract1019937075
- C.N.SciamannaJ.D.DePueM.G.GoldsteinNutrition counseling in the promoting cancer prevention in primary care studyPrev Med352002437446
- E.FrankE.H.WrightM.K.SerdulaL.K.ElonG.BaldwinUS women physicians’ personal and clinical nutrition-related practicesAm J Clin Nutr752002326332
- N.A.AnisR.E.LeeE.F.EllerbeckN.NazirA.GreinerJ.S.AhluwaliaDirect observation of physician counseling on dietary habits and exercise: patient, physician, and office correlatesPrev Med382004198202
- N.K.RussellD.L.RoterHealth promotion counseling of chronic-disease patients during primary care visitsAm J Public Health831993979982
- H.WechslerS.LevineR.K.IdelsonE.L.SchorE.CoakleyThe physician's role in health promotion revisited – a survey of primary care practitionersN Engl J Med3341996996998
- K.M.KolasaK.RickettBarriers to providing nutrition counseling cited by physicians: a survey of primary care practitionersNutr Clin Pract2552010502509
- A.HelmanNutrition and general practice: an Australian perspectiveAm J Clin Nutr656 Suppl19971939S1942S
- T.V.MihalynukC.S.ScottJ.CoombsSelf-reported nutrition proficiency is positively correlated with perceived quality of nutrition training of family physicians in Washington StateAm J Clin Nutr77200313301336
- M.L.VetterS.J.HerringM.SoodA.L.KaletWhat do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledgeJ Am Coll Nutr2722008287298
- K.K.YeagerR.S.DonehooC.A.MaceraJ.B.CroftG.W.HeathM.J.LaneHealth promotion practices among physiciansAm J Prev Med121996238241
- A.BanduraSelf-efficacy: the exercise of control1997W.H. Freeman and CompanyNew York
- Schulman JA, Rienzo BA. The importance of physicians’ nutrition literacy in the management of Diabetes mellitus. Cited in April 2011. Available in <http://www.med-ed-online.org/f0000022.htm>.
- M.FlynnC.SciamannaK.VigilanteInadequate physician knowledge of the effects of diet on blood lipids and lipoproteinsNutr J2200319
- E.H.SpencerE.FrankL.K.ElonV.S.HertzbergM.K.SerdulaD.A.GaluskaPredictors of nutrition counseling behaviors and attitudes in US medical studentsAm J Clin Nutr842006655662
- K.LazarusR.L.WeinsierJ.R.BokerNutrition knowledge and practices of physicians in a family practice residency program: the effect of an education program provided by a physician nutrition specialistAm J Clin Nutr581993319325
- K.Y.FosterN.S.DiehlD.ShawMedical students’ readiness to provide lifestyle counseling for overweight patientsEating Behav32002113
- S.C.AlexanderT.OstbyeK.I.PollakPhysicians’ beliefs about discussing obesity: results from focus groupsAm J Health Promot212007498500
- V.Forman-HoffmanA.LittleT.WahlsBarriers to obesity management: a pilot study of primary care cliniciansBMC Fam Pract7200635
- L.EpsteinJ.OgdenA qualitative study of GPs’ views of treating obesityBr J Gen Pract552005750754
- K.WynnJ.D.TrudeauK.TauntonNutrition in primary care: Current practices, attitudes, and barriersCan Fam Phys5632010e109e116
- J.HymandD.W.MaibachJ.A.FloraS.P.FortmannCholesterol treatment practices of primary care physiciansPublCe Heat Reports10741992441445
- S.KatzA.FeigenbaumS.PasternakS.VinkerAn interactive course to enhance self-efficacy of family practitioners to treat obesityBMC Med Educ520054