Abstract
Introduction
Cerebral venous occlusion (CVO) means intraluminal obstruction by cerebral venous thrombosis (CVT) or external compression. The differential diagnosis is broad including stroke, brain capillary telangiectasia, contusion, hypertensive hemorrhage, metastases and venous vascular malformations. MRI in conjunction with MRV is considered the modality of choice in diagnosis of CVO.
Objective
To assess the role of magnetic resonance venography in the evaluation of cerebral veins and sinuses occlusion.
Methods
The study was conducted on 15 patients with cerebral venous occlusion and subjected to MRI and MRV.
Results
The study included 13 patients with cerebral venous occlusion due to thrombosis and two patients with occlusion by tumors (meningioma).
Conclusion
MRI in conjunction with MRV is considered an accurate, safe, non-invasive, non-ionizing diagnostic modality in assessing CVO. It can assess parenchymal lesions and detect intraluminal small thrombi and its extension.
Keywords:
1 Introduction
Cerebral venous thrombosis or occlusion by extrinsic compression that subsequently progresses to complete occlusion is an elusive diagnosis because of its non-specific presentation and its numerous predisposing causes.Citation1 Cerebral (dural) venous sinus thrombosis is an uncommon condition but become more common than previously thought, its clinical presentation is varied and often dramatic and may occur with headache and cranial nerve palsies.Citation2 It often affects young-to-middle-aged patients, and more commonly women. It is an uncommon cause of cerebral infarction relative to arterial disease but is an important consideration because of its potential morbidity.Citation3
The most common causes and risk factors associated with CVT are due to: genetic prothrombotic conditions: antithrombin deficiency, protein C and protein S deficiency. Acquired prothrombotic states: nephrotic syndrome, pregnancy, and puerperium.Citation4 Infections: otitis, mastoiditis, sinusitis and meningitis. Collagen-vascular diseases: systemic lupus erythematosus, sarcoidosis and Behçet syndrome.Citation5 Hematologic conditions: polycythemia, leukemia, anemia and sickle cell disease. Drugs: oral contraceptives and tamoxifen.Citation6 Mechanical causes: trauma and neurosurgical procedures and miscellaneous causes: dehydration and cancer.Citation7
The imaging characteristics of MRI include: (1) Imaging of the brain parenchyma that appears in the form of non-specific lesions, such as intracerebral hemorrhages or infarcts, edema, isolated or associated with infarcts or hemorrhages, and it can even be normal in up to 30% of patients. (2) Imaging of the cerebral venous system (veins and sinuses thrombus) by direct visualization of a thrombus within the vessel.Citation8 MRV features include non-visualization of the vessel (i.e. no flow), flow defect and presence of collaterals at the site of occlusion.Citation9
2 Methods
Twelve of the 15 patients with known or suspected CVO were subjected to high field MRI of the brain (1.5 T) by using closed MRI unit (Philips and GE) and three patients by using a low field magnet (0.2 T) MRI unit by using open MRI unit (Hitachi) medical system.
The following protocols were applied: axial T1WI, T2WI and flair sequences, sagittal T1WI sequence, coronal T2WI sequence and MRV for all patients using three dimensional-phase contrast technique (3D-PC).
The following parameters were utilized for closed MRI (1.5 T):
Slice thickness: 6 mm, interslice gap: 0.6 mm, field of view: 230 mm2, rectangular field of view (RFOV): 80%, number of signals averaged (NSA): 2, for T1W sequences: repetition time (TR) = 600 ms; echo time (TE) = 15 ms, for T2W sequences: TR = 5000 ms; TE = 120 ms, for FLAIR: TR = 6000 ms; TE = 120 ms.
The MRV phase contrast parameters were: TR = 500 ms, TE = 50 ms, FOV = 230 mm2 and velocity = 15 cm/s.
The following parameters were utilized for open MRI unit (0.2 T):
Slice thickness: 6 mm, interslice gap: 0.6 mm, field of view: 230 mm2, rectangular field of view (RFOV): 100%, number of signals averaged (NSA): 3, T1W sequences: repetition time (TR) = 400 ms; echo time (TE) = 17 ms, T2W sequences: TR = 4000 ms; TE = 120 ms and FLAIR: TR = 9000 ms; TE = 140 ms.
The MRV phase contrast parameters were: TR = 40 ms, TE = 12 ms, FOV = 240 mm2 and velocity = 6 cm/s.
2.1 Statistical method
Statistical analysis was done using numbers and percentages for descriptive purposes.
3 Results
This study included 15 patients with age range from 40 days to 84 years old as mentioned in () and mean age of 33.50 years. Ten patients (66.7%) were females and five patients (33.3%) were males. The most common and earliest clinical presentation in this study was headache followed by convulsion, disturbed consciousness, coma, weakness of one limb, blurring of vision and papilledema. Among the predisposing factors for CVO were post partum complications (four patients – 26.7%), followed by dehydration and post surgery complications, (both included three patients – 20%); however, there was no obvious predisposing factor in five patients (33.3%). The most common cause of cerebral venous occlusion in this study was venous thrombosis, was detected in 13 patients (86.7%) followed by compression from outside by tumor (meningioma) (), that was detected in two patients (13.3%) (). MRI features in our study were observed in the form of parenchymal changes and abnormal signals in thrombosed veins and sinuses in both T1 and T2, in addition to blooming of them. Parenchymal changes in our study were due to thrombosis in 12 patients and tumor in two patients. There was one patient of thrombosed cases reported no parenchymal changes (). These changes were seen in the form of non-hemorrhagic infarction in six patients (40%), hemorrhagic infarction in four patients (26.7%) and edema in seven patients (46.7%) (). The commonest MRI findings were replacement of the signal void of sinuses or veins by abnormal signal intensity. It showed three patterns, the first was hyper intense in both T1 and T2 in six patients (46.2%) (i.e. late subacute stage) (A–C). In two patients (15.4%), it was hyper intense in T1 and iso to hypo intense in T2 (i.e. early subacute stage) (A and C) while in four patients (26.7%), it was hypo intense in both T1 and T2 (i.e. chronic stage) (A and B). Finally, there was one patient with equivocal signal in both T1 and T2 () but was diagnosed by MRV. The main MRV findings in our study were non-visualization of occluded veins or sinuses due to absent signal, flow defect and presence of collaterals that may form in the dura that surrounds the occluded sinus. These collaterals were noted in three patients in this study (23.1%) (C). MRV successfully diagnosed all cases. The most common non-visualized sinus in this study was SSS that was noted in 86.7%, followed by transverse sinus 73.3%, sigmoid sinus 40% and straight sinus 33.3%. More than one occluded sinus could be found in some patients. Both cortical and deep veins could not be visualized in 33.3% and torcular herophili was included in 13.3% (E and F).
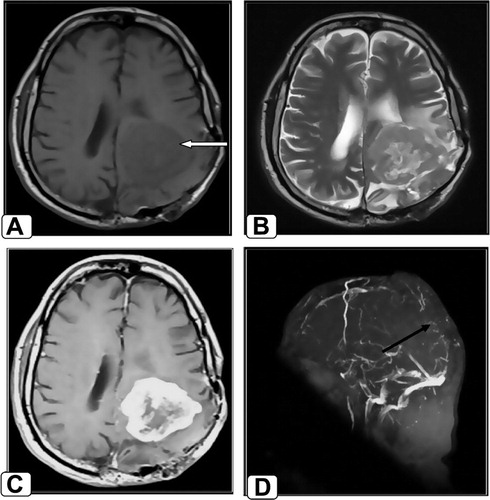
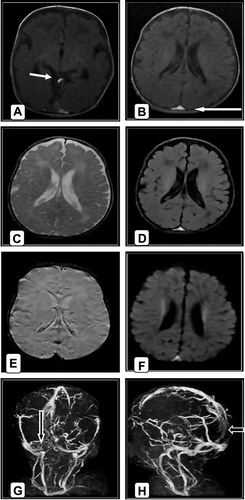
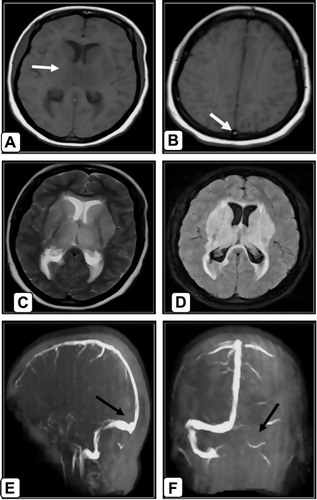
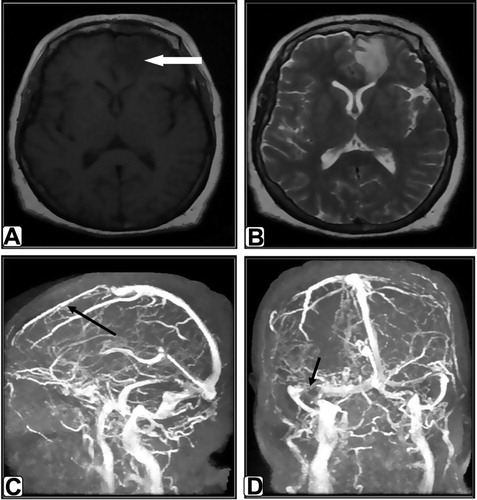
Table 1 Distribution of patients according to age and sex.
Table 2 Distribution of patients according to the causes of cerebral venous occlusion (CVO).
Table 3 Distribution of patients according to MR appearance of parenchymal changes.
Table 4 Distribution of patients according to the MRI appearance of signal changes in dural sinuses and veins.
4 Discussion
The diagnosis of CVT is as difficult as its clinical manifestations are non-specific and may be subtle. Several factors combine to create an extremely elusive diagnosis of CVT: wide spectrum of clinical presentations, various predisposing factors, and the fact that it affects individuals of all age groups.Citation10 CVT may mimic various medical conditions as arterial stroke, tumor, encephalitis, abscess and idiopathic intracranial hypertension (pseudo tumor cerebri).Citation11 So it is a diagnosis of exclusion and imaging investigation. Although most different modalities as DSA, CT, CTV and others help in diagnosis of cerebral venous occlusion (CVO) but each one has specific side effects and some have normal findings.Citation12 Most of patients in this study were in the age groups of <1 year and 30–60 years. This agreed with similar literature reported that the most patients with this disease present in the neonates and young-to-middle-aged patients.Citation3 Other literature reported that it is most common in the third decade while it may occur in all age groups.Citation13 A Canadian study was done on children in 2001 reported that CVST occurs in 10% in the first year of life and this is a lower percentage in comparison with the percentage in our study that reported three patients (20%) in the first year of life.Citation7
Ten patients in the current study were females (66.7%) and five patients were males (33.3%). This agreed with Einhäupl et al.Citation13 that reported 75% of patients were females and had been suggested that the use of oral contraceptives in women is behind the disparity between the sexes. According to the complaints of patients presented with CVT or cerebral venous compression, the current study had shown that headache was the most frequent and often the earliest symptom noted in 10 patients (66.7%). This was in agreement with previous studies of Ameri and BousserCitation14 who reported that 75% of the 110 cases complaint of headache. The most common predisposing factor was puerperium and this is agreed with Nagaraj et al.Citation15 who had found that 200 out of 230 cases (86%) of CVT, seen over eight years, were puerperal in nature. The most common cause of cerebral venous occlusion in the current study was intraluminal thrombus, it occurred in 13 patients (86.7%) and this agreed with Bousser et al.,Citation16 who reported that all patients in his study of 110 cases had cerebral venous occlusion due to thrombosis.Citation16 Occlusion by external compression was seen in two patients (13.3%) and was caused by meningioma and this is different from Jeffrey et al.Citation17 who reported in his study that compression or invasion of cerebral sinuses from dural or calvarial metastases was the main cause in those patients with cerebral sinuses occlusion due to solid tumors. Edema was the most common parenchymal change found in the present study, seen in (46.7%) of cases but Simonds et al.Citation18 observed focal edema in 25% of cases, followed by non-hemorrhagic infarction in (40%) and hemorrhagic infarction found in (26.7%). Nagaraj et al.Citation15 found hemorrhagic infarction in (40.9%) and non-hemorrhagic infarction in (51.6%). Eight patients (61.5%) in our study presented with subacute thrombus. Four cases (26.7%) had chronic thrombus but one patient with equivocal signal. No cases of acute thrombus could be detected. According to some estimates, in 10–30% of cases of sinus thrombosis, the thrombus at initial presentation or imaging examination is in the acute stage of formation.Citation18–Citation20 Subacute-stage thrombus has been found in 55% of patients and this nearly agreed with our study.Citation21,Citation20 and chronic thrombosis was found in 15% of patients.Citation22,Citation20 In the current study, MRV was done in all 15 patients using phase contrast technique in the axial plane with coronal reconstruction. MRV successfully diagnosed occlusion in all 15 cases. It was diagnosed by absence of signal intensity with consequent non-visualization of occluded sinuses or veins in all patients, flow defect in one patient and presence of collaterals in three patients. The superior sagittal sinus was most commonly involved accounting for (86.7%) and this agreed with Ameri and BousserCitation14 who reported in their study of 110 cases that SSS accounts for (72%). We finally concluded that MRI and MRV are valuable imaging modalities for the diagnosis of CVO especially as the clinical presentation and CT findings are usually non-specific. Therefore, the radiologist in the emergency department should be familiar with the imaging findings of CVO or CVT, and if it is suspected on CT, MRI and phase contrast MRV should be recommended as they are safer, non-invasive, non-ionizing and highly accurate modalities. Also phase contrast MRV has the ability to differentiate thrombosed sinuses from normal variants and other pitfalls.Citation18,Citation23
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 14 December 2011
References
- M.G.BousserCerebral venous thrombosis: nothing, heparin or local thrombolysis?Stroke301999481483
- D.J.LanskaR.J.KryscioRisk factors for peripartum and postpartum stroke and intracranial venous thrombosisStroke31200012741282
- J.M.FerroM.G.LopesM.J.RosasLong-term prognosis of cerebral vein and dural sinus thrombosis. Results of the venoport studyCerebrovasc Dis132002272278
- J.M.FerroP.CanhaoJ.StamM.G.BousserF.BarinagarrementeriaPrognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT)Stroke352004664670
- G.DeVeberM.AndrewCerebral sino-venous thrombosis in childrenN Engl J Med3452001417423
- R.EnnaiferA.MoussaL.MouelhiCerebral venous sinus thrombosis as presenting feature of ulcerative colitisActa Gastroenterol Belg722009350353
- W.I.SchievinkM.M.MayaCerebral venous thrombosis in spontaneous intracranial hypotensionHeadache48200815111519
- M.G.BousserJ.M.FerroCerebral venous thrombosis: an updateLancet Neurol62007162170
- M.A.Van BuchemL.LiauwA.SplitMR angiography of the intracranial venous systemRadiology2142000678682
- B.A.KhealaniM.WasayM.SaadahCerebral venous thrombosis: a descriptive multicenter study of patients in Pakistan and Middle EastStroke39200827072711
- M.G.BousserCerebral venous thrombosis: diagnosis and managementEur J Neurol2472000252258
- V.A.DuddalwarMultislice CT angiography: a practical guide to CT angiography in vascular imaging and interventionBJR7720042738
- K.EinhäuplM.G.BousserS.F.de BruijnEFNS guideline on the treatment of cerebral venous and sinus thrombosisEur J Neurol62006553559
- A.AmeriM.G.BousserCerebral venous thrombosisNeurol Clin10199287111
- D.NagarajT.HaridasA.B.TalyM.VeerendrakumarD.K.SubbukrishnaPuerperal cerebral venous thrombosis: therapeutic benefit of low dose heparinNeurol India4719994346
- M.G.BousserH.J.M.BarnettCerebral venous thrombosisH.J.M.BarnettJ.P.MohrB.M.SteinF.M.YatsuStroke pathophysiology diagnosis and management2nd ed1992Churchill Livingstone Inc.New York, NY
- J.JeffryeyM.LisaD.M.RaiseerCerebral sinus thrombosis diagnosed by MRI and MRV venography in cancer patientsNeurology552000309
- G.R.SimondsC.L.TruwitAnatomy of the cerebral vasculatureNeuroimaging Clin N Am41994691706
- J.M.HinmanJ.M.ProvenzaleHypointense thrombus on T2-weighted MR imaging: a potential pitfall in the diagnosis of dural sinus thrombosisEur J Radiol412002147152
- M.BerguiG.BradacClinical picture of patients with cerebral venous thrombosis and patterns of dural sinus involvementCerebrovasc Dis162003211216
- P.J.MacchiR.I.GrossmanJ.M.GomoriH.I.GoldbergR.A.ZimmermanL.T.BilaniukHigh field MR imaging of cerebral venous thrombosisJ Comput Assist Tomogr1019861015
- P.FavroleJ.GuichardI.CrassardM.G.BousserH.ChabriatDiffusion-weighted imaging of intra-vascular clots in cerebral venous thrombosisStroke35200499103
- P.VillablancaF.J.RodriguezT.StockmanlMDCT angiography for detection and quantification of small intracranial arteries: comparison with conventional catheter angiographyAJR1882007593602