Abstract
Background
Serum levels of gastrin-17 (S-G-17) and pepsinogen I (S-PGI) are biomarkers of gastric antral and corpus mucosa, respectively. We determined whether these tests, together with the assay of Helicobacter pylori antibodies, are a nonendoscopic tool for the diagnosis of atrophic gastritis.
Objectives
To study the relation between H. pylori infection and atrophic gastritis in the elderly through the estimation of gastrin 17 and pepsinogen I as novel noninvasive diagnostic biomarkers.
Material and methods
The present study included sixty individuals suffering from gastritis there were divided into two groups. Group (I): Thirty patients having H. pylori infection aged above 65 years. Group (II): Thirty patients without H. pylori infection aged above 65 years. All individuals were subjected to diagnostic upper-gastrointestinal endoscopy and specific gastric biomarkers (serum gastrin-17, serum pepsinogen I/II).
Results
Serum pepsinogen I, II, ratio and gastrin 17 decrease with increasing grade of atrophy of the antrum respectively. Serum pepsinogen I, II, gastrin 17 were significantly lower in mild, moderate, and severe gastritis compared to superficial gastritis patients.
Conclusion
The diagnosis of atrophic gastritis obtained with the blood test panel of G.17, SPG I/II and H. pylori antibodies is in good agreement with the endoscopic and biopsy finding. The panel is a tool for nonendoscopic diagnosis and screening of atrophic gastritis.
1 Introduction
Aging is a basic natural and biological process that goes on continuously in every individual and is responsible for changes affecting the organs by the passage of time. It starts with the onset of life and is terminated by death.Citation1
H. pylori infection increases with age. Its prevalence was found to approach 75% in patients above 65 years of age.Citation2–Citation4
A recent retrospective study has found that H. pylori infection is associated with the majority of cases of symptomatic gastritis in the elderly patients.Citation5
Recent studies have demonstrated a clear association between gastric colonization with H. pylori, gastritis and peptic ulcer disease.Citation6,Citation7 Other epidemiological studies have also shown an association between infections with H. pylori and gastric cancer, the evidence is so complete that the world health organization has recently categorized H. pylori as a category I carcinogen.Citation8–Citation12
Gastric atrophy characterized by the loss of antrum glands is considered a precursor of gastric adenocarcinoma since H. pylori increases the risk of gastric adenocarcinoma. It was been classified as a class I oncogenic factor,Citation13 despite the central role of atrophic gastritis as a major risk factor for gastric carcinoma. Its diagnosis and its grading and proper assessments are done poorly or not at all in clinical practice.Citation14
Because H. pylori infection is a necessary causative factor in the majority of cases of gastric cancer, eradication of the infection will very likely reduce the incidence of gastric cancer.Citation14
The assays of serum/plasma pepsinogen I, pepsinogen II and pepsinogen I/pepsinogen II ratio in addition to gastrin 17 are easy tools for assessment of the presence or absence of atrophic gastritis even in a clinical setting whereas endoscopy is not available.
1.1 The aim of this work
To study the relation between H. pylori infection and atrophic gastritis in the elderly through the estimation of serum (gastrin-17 and pepsinogen-I) as novel noninvasive diagnostic biomarkers.
2 Methods
The present study included 60 individuals suffering from gastritis divided into two groups.
Group (I): Thirty patients having H. pylori infection aged above 65 years.
Group (II): Thirty patients without H. pylori infection aged above 65 years.
All patients included in the study were recruited from Main University Hospital and Fever Hospital.
2.1 Exclusion criteria
Patients with any other disease causing gastric insult were excluded from the study as were patients with diabetes mellitus, autoimmune diseases, chronic systemic infection, liver disease, chronic renal diseases and neoplastic disorders and also patients receiving drugs known to affect the gastric mucosa.
After taking a written consent from all patients, they were subjected to:
2.2 Endoscopy and biopsy sampling
Diagnostic upper gastrointestinal endoscopy was performed in all patients, two biopsies were taken from antrum to detect H. pylori, one for rapid urease and the other one for histopathological examination.
The biopsy specimens were immediately placed in a fixative (10% buffered formalin). The formalin fixed specimens routinely processed and embedded in paraffin blocks were serially cut and mounted on glass slides. The slides were stained with the conventional H&E stain. The prepared section was carefully examined by the light microscope and scored semi-quantitatively according to the updated Sydney classification system.Citation15
2.3 Blood samples
The basal blood samples for the measurement of PGI, PGII, and gastrin 17 were obtained with the subjects in recumbent position, after an overnight fast, after venipuncture, serum and plasma sample were centrifuged and therefore kept at room temperature for 2 h. Before analysis samples were frozen at −20 °C for the latter assay of gastrin and pepsinogen.
Diagnosis of atrophic gastritis by the blood test panel in delineation of patients with different topographic types of atrophic gastritis took place; with the blood test panel an algorithm and a computer program (Gastrosuft, Bioint Plc) were used.
Three criteria for the best discrimination of gastritis of different types were obtained from previous studies.Citation15,Citation16
2.4 Laboratory tests
2.4.1 Gastropanel test
| (a) | Estimation of H. pylori IgG by ELISA with references negative <30, positive >30.Citation17 | ||||
| (b) | Estimation of pepsinogen I by ELISA with reference range of 30–105 μg/l.Citation17 | ||||
| (c) | Estimation of gastrin 17 by ELISA with a reference range of 1–10 mmol.Citation17 | ||||
| (d) | Estimation of serum pepsinogen II by ELISA with reference range of 4–9 ng/ml.Citation17 | ||||
| (e) | Estimation of pepsinogen I/II ratio by ELISA with reference range of 3–20. | ||||
2.5 Statistical methods
The Data were collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 17) software.
Arithmetic mean, standard deviation, for categorized parameters, chi-square test was used while for numerical data t-test was used to compare two groups while for more than two groups ANOVA test was used, least significant differences (LSD) was basically a t-test used only when the F-value is significant to detect the presence of significance between each of the two groups. The level of significance was 0.05.
3 Results
The mean age was 69.4 ± 5.04 years in H. pylori +ve group and 70.1 ± 3.69 years in H. pylori −ve group. There was no significant difference between both groups (P is significant if <0.05) ().
Table 1 Demographic data in the studied groups.
The mean body mass index (BMI) was 21.2 ± 2.20 kg/m2 in H. pylori +ve group and 20.9 ± 2.07 kg/m2 in H. pylori −ve group. There was no significant difference between both groups. (P is significant if <0.05) ().
The mean serum pepsinogen I was significantly lower in H. pylori +ve group (23.9 ± 21.84) unit compared to H. pylori −ve group (117.4 ± 43.47). (P is significant if <0.05) ().
Table 2 Relation between degree of gastritis and the other parameters.
The mean serum pepsinogen II was significantly lower in H. pylori +ve group (23 ± 23.31) unit compared to H. pylori −ve group (48.1 ± 28.94). (P is significant if <0.05) ().
The mean serum pepsinogen I/II ratio was significantly lower in H. pylori +ve group (1.4 ± 0.98) unit compared to H. pylori −ve group (4.1 ± 3.85). (P is significant if <0.05) ().
The mean serum gastrin was significantly lower in H. pylori +ve group (32.8 ± 25.92) compared to H. pylori −ve group (17.3 ± 8.24). (P is significant if <0.05) ().
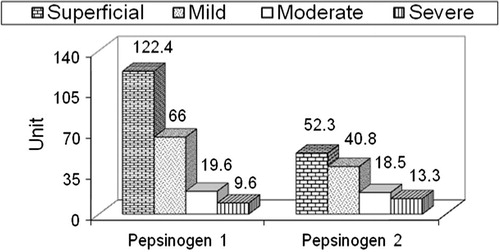
The mean serum pepsinogen I was significantly lower in mild, moderate and severe gastritis patients compared to superficial gastritis patients and it was significantly lower in moderate and severe gastritis patients compared to mild gastritis patients. (P is significant if <0.05) (, ).
Table 3 Relation between H. pylori and degree of gastritis.
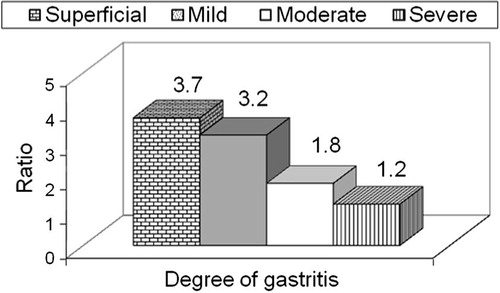
The mean serum pepsinogen II was significantly lower in moderate and severe gastritis compared to superficial and mild gastritis patients. The mean serum pepsinogen I/II ratio was significantly lower in moderate and severe gastritis patients compared to superficial and mild gastritis patients. (P is significant if <0.05) (, and ).
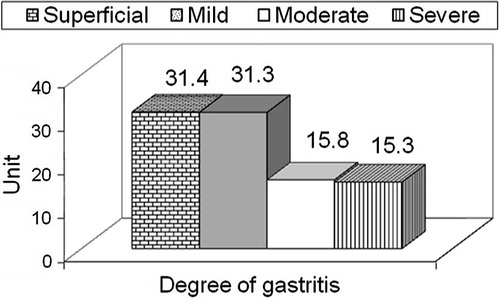
The mean serum gastrin was significantly lower in moderate and severe gastritis patients compared to superficial and mild gastritis patients. (P is significant if <0.05) (, ).
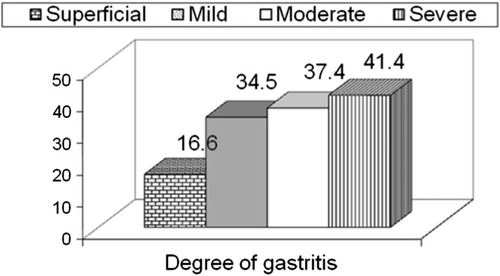
The mean H. pylori antibody was significantly higher in mild, moderate and severe gastritis patients compared to superficial gastritis patients ().
As regards serum pepsinogen I at cut off value <97, sensitivity was 100%, specificity 81.5%, positive predictive value 86.81, negative predictive value 100% and accuracy 91.7% in detecting atrophic gastritis ().
Table 4 Evaluation of different markers in prediction of atrophic gastritis.
As regards serum pepsinogen II at cut off value <52 sensitivity was 93.9%, specificity 63% positive predictive value 75.6%, negative predictive value 89.5% and accuracy 80% in detecting atrophic gastritis ().
As regards serum pepsinogen I/II ratio at cut off value <1.82 sensitivity was 66.7% specificity 66.7%, positive predictive value 71.0% negative predictive value 62.1% and accuracy 66.7% in detecting atrophic gastritis ().
As regards serum gastrin at cut off value <28 sensitivity was 90.9%m specificity 44.4% positive predictive value 66.7%, negative predictive value 80%, accuracy 70% in detecting atrophic gastritis ().
4 Discussion
The present study indicates that, in association with H. pylori testing, the serum level of G-17 and PGI can be used as biomarkers of gastritis and atrophic gastritis in the antrum. In the present study S.G.17 decreased with increasing grade of antral atrophy among H. pylori infected patient. Correspondingly S-PGI decreased with increasing grade of antral atrophy in a way that has been demonstrated in many previous studies.Citation18–Citation24
Studies by using all three blood tests (H. pylori antibody assay, SG17, and SPGI as panels were done and by using the gastro soft computer program to generate the diagnosis it was possible to delineate the patients with advanced atrophic gastritis with a reasonably high accuracy. The data from the present prospective study among gastritis patients were comparable with those from observational case, control studyCitation25 and prospective Italian study,Citation26 these three studies suggested that the overall accuracy of the panel in the diagnosis of atrophic gastritis is approximately 80% when compared with the diagnosis from endoscopy and biopsies.
Serum PG known to be a marker for gastritis serum PG has been reported to be a marker for atrophic gastritisCitation27,Citation28 and is used for the eradication of H. pyloriCitation29–Citation31 Moreover low PG concentration defines groups at high risk of gastric cancer and adenomaCitation32,Citation33 in describing the relationship between gastritis and pepsinogen concentrations, Samloff et al.Citation27 used the term “serologic biopsy” and Miki et al.Citation28 reported that I:II ratio was correlated with the extent of atrophic gastritis.
Diagnosis of atrophic gastritis by biopsy specimen is often unreliable and the interobserver variation is large in particular in antral biopsy. This may be due to the fact that atrophic lesions are often patchy due to the fact that atrophic lesions are often patchy and a limited number of biopsy specimens may easily result in under or over diagnosis, the existing inflammation may also bias the microscopic appearance that leads to over estimation of atrophic gastritis due to artificial impression of loss of glands. It is conceivable that the blood test panel avoids these biases.Citation34
Therefore the blood test panel is not a direct test for cancer or peptic ulcer but it may reveal patients who are at risk for this disease and when endoscopy is mandatory.Citation34
5 Conclusion
From the study we concluded that H. pylori is common in the elderly and it is the most important cause of atrophic gastritis in the elderly. Atrophic gastritis in the elderly is considered as a major risk factor for gastric carcinoma. The diagnosis of atrophic gastritis obtained with the blood test panel of SG17 SPGI, ratio and H. pylori antibodies is in good agreement with the endoscopic and biopsy findings.
Our study recommends that the blood test panel is a noninvasive alternative in the initial examination of patient dyspepsia. The panel helps to identify easily and nonendoscopically patients with atrophic gastritis in the antrum.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 1 September 2012
References
- G.C.WilliamsPleotropy, natural selection and the evolution of senescenceSci Aging Knowl Environ 20011200113
- K.LijimaS.OharaT.KoikeGastric acid secretion of normal Japanese subjects in relation to Helicobacter pylori infection, aging and genderScand J Gastroenterol392004709716
- H.BrennerU.ArndtC.StegmaierIs Helicobacter pylori infection a necessary condition for noncardia gastric cancerAm J Epidemiol1592004252258
- J.KountenrasC.H.ZavosPyloric infection and reflex esophagitisGut532004912
- N.BhalaJ.NewtonUpper gastrointestinal alarms in older peopleLancet3662005982983
- J.KountourasM.BozikiE.GavalasEradication of Helicobacter pylori may be beneficial in the management of Alzheimer diseaseJ Neurol2562009758767
- A.PilottoAging and upper gastrointestinal disorders. Best pract res chinGastroenterol18Suppl.20047581
- P.CorreaJ.FoxT.FathomHelicobacter pylori and gastric carcinomaCancer60199025692574
- D.FormanD.G.NewallAssociation between infection and Helicobacter pylori and risk of gastric cancer evidence from investigationBr Med2003230234
- Who infection with Helicobacter pylori in: Schorpsanas, liver flucks and Helicobacter pylori. Lyon: International agency for research on cancer 1994; 61:177.241.
- Nilt consensus conference Helicobacter pylori in peptic ulcer disease. J Am Med assoc 1994; 274:65–69.
- M.SuzukiS.MituraSemesterHelicobacter pylori elicits gastric mucosal cell damage associated with dyplasiaGut52002230231
- D.W.FaddenJ.ValleK.VarisGastorduodenal disease in the elderly patientSur Clin North Am741994113
- K.VarisP.SipponenF.LaxenI.M.SamloffJ.K.HuttunenP.R.TalorAnt the Helsinki Gasritis Study Group. Implications of serum pepsinogen in early endoscopic diagnosis of gastric cancer and dysplasiaScand J Gastroenterol352000950956
- F.Di-MarioA.M.MouraSerological biopsy in the first degree relative patients with gastric cancer affected by Helicobacter pylori infectionScand J Gastroenterol38200312231227
- M.F.DixonR.M.GentaJ.H.YardleyP.CorreaClassification and grading of International workshop on the histopathology of gastritis, Houston 1994Am J Surg Pathol2010199611611181
- N.BroutertM.PlebaniPepsinogen, I pepsinogen II and gastrin as markers of atrophic gastritis in European dyspepticsBr J Cancer88200312471259
- K.VarisI.M.SamloffT.IhamakiM.SiuralaAn appraisal of tests for severe atrophic gastritis in relatives of pernicious anemiaDig Dis Sci242009187191
- K.MikiM.IchinoseN.YahagiT.SuzukiM.OkaY.ShimizuEfficiency of gastric screening system using serum pepsinogen testSecond international gastric cancer congress, Munich, Germany1019972730
- N.BroutetM.PlebaniC.SakarovitchP.SipponenPepsinogen A, Pepsinogen C and Gastrin as markers of atrophic chronic gastritis in European dyspeptics F Megraud and the Europygast Study GroupBritish Journal Cancer88200312391247
- A.KorstanjeS.van EedenJ.A.OfferhausF.L.WaltmanG.HartogF.W.RoelandseComparison between serology and histology in the diagnosis of advanced gastric body atrophy: a study in a Dutch primary communityJ Clin Gastroenterol.4220081822
- E.MoranaL.GuidaL.G.CavallaroR.Merli2R.ZuppardoR.CavestroGastrin-17 (G-17): a serological bio-marker for diagnosis of gastroesophageal reflux disease (GERD)Digest Liv Dis402008S77
- L.G.CavallaroA.MainiA.NovenneE.MoranaR.MerliM.VeneritoSerum pepsinogen II as a marker of both Helicobacter pylori and acetyl salicylic – acid related gastritisHelicobacter112006395
- B.GermanàF.Di MarioL.G.CavallaroA.M.MoussaP.LecisS.LiatopoulouClinical usefulness of serum pepsinogens I and II, gastrin-17 and anti-Helicobacter pylori antibodies in the management of dyspeptic patients in primary careDig Liver Dis372005501508
- P.SipponenP.RantaT.HelskeT.Kaarainen Im MakiA.LinnalaSerum levels of amidated gastrin-17 and pepsinogen I in atrophic gastritis. An observational case-control studyScand J gastroenterol372002785791
- G.NicoliniR.ZagariP.PozzatoV.LunedeiL.De LucalF.AntoniniDiagnosis of atrophic gastritis based upon a combination of three non-invasive tests: preliminary results of the lciano-Monghidoro projectJ Gastroenterol Hepatol172002A264
- I.M.SamloffK.VarisT.IhamakiM.SiuralaJ.I.RotterRelationships among serum pepsinogen I, serum pepsinogen II, and gastric mucosal histology: a study in relatives of patients with pernicious anemiaGastroenterology831982204209
- K.MikiM.IchinoseA.ShimizuS.C.HuangH.OkaC.FurihataSerum pepsinogens as a screening test of extensive chronic gastritisGastroenterol Jpn221987133141
- F.Di MarioL.G.CavallaroA.M.MoussaP.CaruanaR.MerliA.MainiUsefulness of serum pepsinogens in Helicobacter pylori chronic gastritis: relationship with inflammation, activity, and density of the bacteriumDig Dis Sci51200617911795
- T.FurutaE.KanekoS.BabaH.AraiH.FutamiPercentage changes in serum pepsinogens are useful as indices of eradication of Helicobacter pyloriAm J Gastroenterol9219978084
- F.Di MarioA.M.MoussaL.G.CavallaroP.CaruanaR.MerliS.BertoliniClinical usefulness of serum pepsinogens II in the management of Helicobacter pylori infectionDigestion702004167172
- F.M.HunterP.CorreaE.FonthamB.RuizM.SobhanI.M.SamloffSerum pepsinogens as markers of response to therapy for Helicobacter pylori gastritisDig Dis Sci38199320812086
- K.MikiM.IchinoseK.B.IshikawaN.YahagiM.MatsushimaN.KakeiClinical application of serum pepsinogen I and II levels for mass screening to detect gastric cancerJpn J Cancer Res10199310861090
- A.KodoiM.YoshiharaK.SumiiK.HarumaG.KajiyamaSerum pepsinogen in screening for gastric cancerJ Gastroenterol301995452460