Abstract
Introduction
Complex acetabular fractures are not uncommon injuries in Egypt. The aim of surgical treatment is to preserve hip mobility and to avoid post-traumatic arthritis.
Aim
The aim of this study was to evaluate the clinical results of patients presented by displaced complex acetabular fractures and treated by open reduction and internal fixation. Factors affecting these results were to be determined.
Methods
Displaced acetabular fractures involving the both columns were included. Initial assessment and treatment were directed towards the patient's general condition. Posterior hip dislocation was reduced as fast as possible. Standard X-ray views and CT cuts were done for every patient. The definite surgery was done through an ilio-inguinal, a Kocher–Langenbeck or combined approaches. Postoperatively, the residual displacement was recorded together with the head roof relationship. Using Matta radiological and modified clinical grading, a correlation between radiological and clinical results was made. Factors affecting the outcome were defined.
Results
The study involved 55 patients between May 2007 and December 2010. The mean follow-up period was 29.62 ± 7.19 months with a minimum of 12 months and a maximum of 43 months. Excellent to good results were achieved in 38 cases, 69.1%, while fair to poor results were obtained in 17 cases, 30.9%. Anatomical reduction and/or restoration of perfect head/roof congruency were strongly associated with better outcome. Beside this there was significant relation between good clinical outcome and the utilisation of the anterior approach. On the other hand bad outcome was associated with these factors: (1) associated pelvic ring injury, (2) fracture of the posterior wall, (3) articular surface comminution and (4) the presence of intra-articular fragments.
Conclusion
Fracture personality and not the fracture type is the main determinant of its complexity. Surgical experience is required to achieve the best reduction while avoiding complications.
1 Introduction
The term complex acetabular fracture is not clearly defined in the literature. Some authors restricted its use only to the associated fracture patterns according to Letournel classification.Citation1–Citation5 Others used the term for any fracture that involves both columns of the acetabulum.Citation6–Citation13 Such patterns of fractures are more challenging in their treatment planning and implementation. The approach is not fixed, the reduction is more difficult and the overall clinical results are known to be worse than simpler fracture patterns.Citation4,Citation14–Citation17 The aim of this work was to document our clinical results after such difficult fracture patterns. Also we tried to determine factors affecting these results in order to reach a better definition for the term; complex acetabular fracture.
2 Methods
The study was done in Elhadarah University Hospital. A protocol was set to include 50 or more patients and to follow them prospectively. The minimum follow-up period was set to be 12 months for every individual case. Informed consent was taken from every patient to be involved in the study. Patients were selected according to these following inclusion and exclusion criteria.
2.1 Inclusion criteria
Following Letournel's classification, fractures that involve both columns of the acetabulum were only included.Citation18 These are the transverse, transverse posterior wall, T-type, anterior and posterior hemi-transverse type and the associated both columns fracture. Surgery was indicated if the acetabular fracture was presented with either (1) instability of hip due to a wall or a column fracture, (2) incongruity between the head and the dome of the acetabulum due to (a) displacement of the dome fragment or the posterior column in an associated both columns fracture, (b) a trans-tectal component of transverse or T-type fracture and (c) retained intra-articular fragments and marginal impactions. All fractures were treated within three weeks of injury. Medically fit adult patients without severe osteoporosis were only included.
2.2 Exclusion criteria
The following fracture patterns were excluded: (1) minimally displaced fractures with the hip joint stable and congruent, (2) both column fractures with secondary congruence, (3) fractures involving single wall or column, (4) fractures that present after three weeks of injury, (5) pathological fractures, (6) fractures on top of a previous hip disease and (7) patient with severe osteoporosis or severe systemic illness rendering operative intervention high risk.
After admission, every patient underwent full assessment including history taking, clinical examination for the patient and the injured hip. Any neurological deficit was reported. Appropriate trauma series of X-rays was requested according to patient's presentation. Initial management was directed to patient's general condition and to the associated injuries if present. Closed reduction of the posterior hip dislocation was performed as fast as possible. Dislocation reduction interval, hip stability and the condition of the sciatic nerve before and after reduction were documented. All patients were encouraged to maintain active exercises for toes and ankle. A dose of 40 IU low molecular weight heparin was given for all patients once daily starting from the first day of injury. This was stopped 12 h before operation and then was given again from the first night after operation in the same dose for three weeks.
After stabilization of the patient, the full radiological workup was completed. This included the three X-ray views (A/P, obturator view and oblique view) and the CT scan with 3D reconstruction. The plain radiographs and CT scans were examined for the presence of certain modifiers that were thought to have a possible influence on the prognosis of the acetabular fracture. These modifiers included the presence of articular comminution, marginal impaction of the articular surface, incarceration of intra-articular fragments or a femoral head lesion.
2.3 Operative technique
General anaesthesia or spinal ± epidural analgesia was given according to the preference of the anaesthesiologist. A catheter was inserted in the urinary bladder before draping. A dose of 2 g from the third generation cephalosporin, Ceftriaxone was given during the induction of anaesthesia. The same dose was repeated at the first post-operative night and then once daily for another three days.
The operation was performed on a standard table. The image intensifier was positioned accurately before draping of the patient. Check preliminary images was taken in the A/P and oblique projection. The surgical approach was chosen based on the direction of displacement. All surgeries utilized either an anterior ilio-inguinal approach, or a posterior Kocher–Langenbeck approach.Citation18 In certain cases the two approaches were combined either in the same session of anaesthesia or in two separate occasions.Citation19,Citation20
When the ilio-inguinal approach was used the patient was positioned in the supine decubitus and the three windows were created. Traction was done manually by an assistant. Reduction was then started following the proximal to distal rule of Letournel.Citation18 Fixation was done using plates and screws as the fracture dedicated. Spring plates were applied to reduce and hold a separated medial wall.
When the Kocher–Langenbeck was used the patient was positioned either in the lateral or prone decubitus. Careful detachment of the external rotators and the piriformis was done while preserving the deep medial femoral circumflex artery. The sciatic nerve was protected by its special retractor. Inspection of the interior of the joint was done through the capsular rent or the posterior wall fracture and was helped by longitudinal traction on the limb combined with trochanteric traction by a T-handled hook. No re-dislocation was attempted. Reduction was done by traction and/or pelvic reduction clamps. Marginal impaction of the articular cartilage was treated by elevation and grafting. Fixation was done by small fragment reconstruction plates and lag screws.
Before closure a check by image intensifier was done to assess the reduction and to rule out an intra-articular hardware. Wound closure over suction drains was performed. Any intra-operative complication was recorded.
2.4 Post-operative regimen
The patient was mobilized from bed as early as possible. Partial weight bearing was allowed after 6 weeks and full weight bearing was allowed at 12 weeks. No routine prophylaxis for heterotopic ossification was adopted.
Within the first week, post-operative X-rays were done for the operated hip including three views (A/P view, obturator view and iliac view). The accuracy of the reduction was assessed using the modified radiological grading of Matta (anatomical: 0–1 mm, imperfect: 1–3 mm, poor >3 mm).Citation14 The relationship between the femoral head and the roof of the acetabulum was described following Letournel's descriptions as follows: (1) maintained head/roof congruency, (2) loss of parallelism in the upper joint space, (3) loss of parallelism and subluxation of the head and (4) secondary surgical congruence.Citation18
2.5 Follow-up
Patients were seen at 2 weeks for the removal of skin sutures or staples. Then, they were followed at 6 and 12 weeks, 6 months and one year.
The study adopted the modified clinical grading proposed by Matta.Citation14 The clinical grade includes three items each has six points and the total score will be out of 18 points. Any early or late complication was recorded.
Data were collected in a prepared sheet. Statistical analysis was done using SPSS version 11.0.1 for Windows (SPSS Inc., Chicago, Illinois). Spearman's correlation was used to detect linear relations between quantitative variables while Mann–Whitney and Kruskal–Wallis tests were used to rank and compare qualitative variables against the median final clinical score. A p-value .05 was considered to be statistically significant.
3 Patients
This study included 55 patients between May 2007 and December 2010. Their age ranged between 17 and 65 years with a median age of 28 years. Most of patients were males (70.9%). All cases in this study got their acetabulae fractured due to high energy trauma. The dominant cause of trauma was motor vehicle accidents (85.5%). Twenty patients (36.4%) received the impact directly on the hip. Nearly, an equal number of patients (19 patients = 34.5%) received the impact on the knee as an indirect pattern of injury. Both sides were affected almost equally.
No case of haemodynamic instability was encountered. Skeletal injuries accompanied the acetabular fracture in more than one half of the patients (30 patients = 54.5%). The most frequently encountered injuries were that of the lower limb (30.9%) followed by the pelvic ring injuries (18.2%). There was only one associated skeletal injury in 17 patients (56.7%) and two injuries in eight patients (26.7%).
Preoperative neurological examination revealed that the common peroneal division of the sciatic nerve was paralysed in six patients (10.9%). During surgery, none of these nerves were found transected or grossly lacerated. Therefore, the diagnosis of traction injury was made in all of these cases. Local examination of the soft tissue around the hip revealed extensive contusions in 10 cases (18.2%).
Hip dislocation was encountered in 21 hips (38.2%). There were 12 posterior dislocations (21.8%) and nine medial dislocations (16.4%). Closed reduction was successful in 7/12 (58.3%) posterior dislocations. For the other five (41.7%) posterior dislocations; there were three irreducible hips and two unstable hips.
The most common fracture type was the associated both columns type (18 cases = 32.7%). The least common was transverse type (four cases = 7.3%). Marginal impaction of the posterior wall was present in four (7.2%) fractures. Although all these four fractures were belonging to the transverse + posterior wall family, the main pathology was in the posterior wall with minimally displaced transverse component. One case (1.8%) had marginal impaction in the dome area (Sea Gull sign).Citation21 Radiologically evident head lesions were diagnosed in six fractures (10.9%). Other subtle head lesion might be present but were not diagnosed. Intra-articular loose fragments (IAFs) were found in 27 (49.1%) fractures. The mean amount of preoperative maximum displacement was 24.1 ± 9.83 mm. The posterior wall of the acetabulum was fractured in 26 cases (47.3%). The fractured posterior wall was one fragment in 21 cases (38.2%) and comminuted in five (9.1%) cases. The quadrilateral surface of the acetabulum exhibited secondary independent fracture lines in 10 cases (18.2%).
Posterior approach was utilized in 54.5% of cases while anterior approach was utilized in 27.3% of cases. The rest of cases 18.2% were operated via combined approaches.
4 Results
4.1 Radiological results
The median post-operative displacement was 3 mm (0–15). Reduction was considered anatomical in 18 cases (32.7%) and imperfect in 16 cases (29.1%). Poor reduction was seen in 21 cases (38.2%). Head/roof congruency was restored perfectly in 40 cases (72.8%).
4.2 Clinical results
The mean follow-up period was 29.62 ± 7.19 months with a minimum of 12 months and a maximum of 43 months. Patients were categorized into four groups according to their total clinical score. Patients with excellent to good results were considered satisfactory (38 cases = 69.1%), while patients with fair to poor results were considered unsatisfactory (17 cases = 30.9%) ().
Table 1 Final clinical results.
4.3 Factors affecting the clinical results
According to the fracture type, anterior column + posterior hemi-transverse pattern had the highest scores followed by the pure transverse and then the associated both columns. The lowest scores were observed in transverse + posterior wall and in the T-type fractures. The difference among all these types did not reach the level of statistical significance (p = .09). Similarly speaking, neither the duration of dislocation nor its type had a significant effect on the final score (p = .9, .5).
The clinical results were significantly better among cases operated through a single anterior approach. On the other hand, the clinical results were significantly worse among patients suffered an associated pelvic ring injury (p = .018); if the posterior wall was involved (p = .006); in the presence of two modifiers namely, articular surface comminution (p = .002) or intra-articular fragments (p = .001). Considering the other two modifiers namely; femoral head lesion and marginal impaction were also associated with better results. However their effect was not statistically significant.
The measured maximum post-operative displacement in mm had an inverse statistically significant relationship with the final score. The more the displacement, the less the score (p = .003). Anatomical and imperfect reductions were significantly better than poor reduction (p = .002, .045). However, the difference between anatomical and imperfect reductions did not reach the level of statistical significance (p = 1.0).
Congruent reduction of the femoral head under the acetabular dome was associated with the best final scores (see ). The final score for cases with incongruent reductions was lower. When subluxation was added to incongruency, the final score was even worse. Secondary congruent hips achieved a little bit higher scores than did incongruent and/or subluxed hips. However, the only statistically significant difference was found between the congruent group and all other groups (p = .000). summarizes the distribution of different variables and their effect on the final outcome.
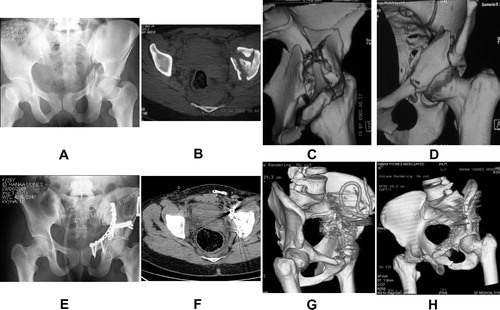
Table 2 The relationship between various variables and the final clinical score.
4.4 Complications
All cases of iatrogenic partial sciatic nerve palsy were recovered by the end of follow-up (five cases = 9.1%). On the other hand, all cases with traumatic sciatic nerve injury did not recover from their neurological deficit by the end of follow-up. In addition to the sciatic nerve, the lateral cutaneous nerve of the thigh was injured in seven cases (12.8%). Femoral nerve suffered injury in two cases (3.6%) with a complete recovery in one case and partial in the other one. These rates became even higher when adjusted according to exposure utilized. For example, the lateral cutaneous nerve was injured in 28% of anterior exposures and the sciatic nerve was injured in 12.5% of posterior exposure.
There was only one case with intra-operative excessive bleeding during a second session where ilio-inguinal approach was done one week after posterior fixation. Bleeding came out from the area of the greater sciatic notch after mobilisation of a displaced quadrilateral plate. Initial packing was done until the vascular surgeon came to field. He decided that bleeding is coming out from the presacral plexus of veins. Ligation of the internal iliac artery together with pelvic packing was done. Packs were removed after 72 h and no further bleeding was encountered. Unfortunately this patient developed deep wound infection. Inspite of repeated debridement infection reached the bone causing chronic osteomeylitis and hip joint arthrosis.
Secondary loss of reduction was encountered in two cases. One case was a T-type fracture operated posteriorly lifting the anterior column without fixation. The other case was an associated both columns fracture operated anteriorly and the posterior column was fixed only by two unicortical screws for fear of joint penetration. Unfortunately the non-fixed columns moved again in the early follow-up. These cases demonstrated the cost of the learning curve.
The relation between early joint related complications and the final outcome was observed. Patients who suffered from post-operative joint infection or early loss of reduction had lower median score compared to remaining patients. This difference was highly significant. (z = −2.564, p = .01).
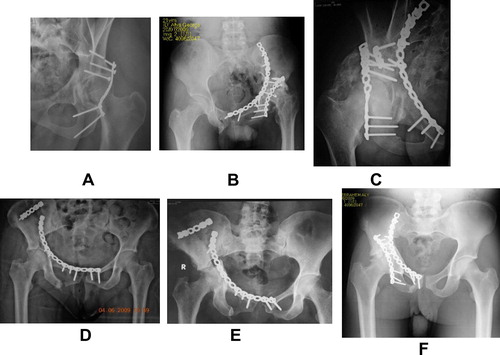
Hardware related complications were in the form of inadvertent intrarticular screw which necessitated the removal in one case. The drill bit was broken in one case. In another two cases the screws holding the posterior column plates were broken after healing of the fracture .
4.4.1 Late complications
We had only two cases with immature heterotopic ossification. Early osteoarthritis supervened in 14 cases (24.45%). The median post-operative displacement in the non-arthritic group was lower than in the arthritic group (2, 5 mm, respectively). This difference was highly significant (z = −3.36, p = .001). Examples of some complications encountered in our series are shown in .
5 Discussion
The design of this study had included only the most technically difficult acetabular fractures. The most important output of this work is the correlation between the accuracy of reduction and the clinical results. It was possible, even in these difficult patterns to end by a satisfactory outcome when every effort was done to achieve the best possible reduction. Therefore, at the time of reconstruction, the surgeon who is dealing with these injuries should think only about preservation of hip function as possible as the injury allowed him. This comes though striving for anatomical reduction. In other words, acetabular fixation is not just a preparation for hip replacement.
However, the relatively low rate of anatomical reductions in this work clarified how long could be the learning curve especially in these most challenging acetabular injuries. It was not an easy job to bring down every displaced often multi-fragmentary acetabular fracture to the perfect reduction (i.e. <1 mm residual displacement). As expected, a long and very steep learning curve is required. This may explain why anatomical reductions in this series were as low as 32.7%. Similarly speaking, Schmidt et al. treated 21 similar complex cases involving the two columns of the acetabulum and achieved anatomical reduction in only one-third of their cases.Citation22 Mears et al. showed in their study of 424 fractures treated by operation that simple fractures were reduced anatomically in 87% of patients, whereas associated fractures could be reduced anatomically in only 59%.Citation23 Considering the German Registry, Ochs et al. found that despite changes in the chosen approaches and an increased surgical frequency, the operative treatment of acetabular fractures of the last 15 years did not lead to an increased reduction quality.Citation24 On the other hand, Matta achieved perfect anatomical reduction in 64% of associated fracture patterns included in his series.Citation14 This is almost double the rate of this series and reflects the higher experience of the author. Stockle et al. achieved anatomical reduction in 79.5% of similar complex cases included in his series. This relatively higher rate of anatomical reductions may be attributed to their use of extensile approaches in most of their cases and to the selection of non-comminuted cases to fit for their method of fixation with screws only.Citation25
The second important output is the redefinition of the term complex acetabular fracture. LetournelCitation26 classification was introduced to facilitate management rather than to determine the prognosis. Instead, factors like bone comminution and primary cartilage damage should be the real challenger during acetabular surgery. In this series and regardless of the fracture type, bad prognosis was expected if the posterior wall was involved, if there was an associated pelvic ring injury or if there was articular surface comminution or intra-articular fragments. All these factors might reflect the picture of the primary cartilage damage or might add obstacles to reach the goal of anatomical reduction. The significance of these traumatic lesions of the acetabular cavity was clearly depicted in the report of Rommens et al.Citation27 who found that fracture comminution, subchondral impaction or intra-articular fracture fragments, which were present in half of their patients, significantly worsened the outcome despite of the anatomical reduction achieved in these cases. They reported that 20 of 23 patients, who had moderate or bad results following the Merle d’Aubigne score (86.9%) had one or more modifiers. Therefore, they recommended thorough analysis of preoperative CT-data to have a more detailed view on the “personality” of the acetabular fracture helping in better patient selection and in predicting the prognosis of an individual fracture.Citation27
Experts in this field agree that there is no simple acetabular fracture.Citation28 Local complications which are partially controllable showed a significant association with poor outcome. This association was true also for Murphy et al. who found that local complications necessitating re-operation and imperfect reduction were two prognostic factors strongly associated with sub-optimal outcome. Citation5 Since both factors can be reduced by experienced surgical management, this lends weight to the argument that these injuries should be treated at specialized centres.Citation16
This study has some limitations. First of all, the number included in this study is relatively small given that this sample was fragmented many times to study the effect of a given factor on the clinical result. The paucity of patients per subgroup in this study did not allow multivariate statistical analysis and hence there was no control for the confounding factors. Difficulties related to the statistical analysis of outcome after acetabular fracture had been highlighted by Matta.Citation29 Given the facts that these injuries are relatively uncommon, that there are many fracture types and that there is a wide spectrum of patients and surgical treatment, it is difficult to come to a meaningful statistical conclusion as the sub groups are too small to reach significance.
The second important limitation was the relatively short follow-up period. The mean follow-up period in this study was about 2.5 years. However, most of the poor clinical results in this series were already obvious within the first year. MattaCitation30, Rowe and LowellCitation31 as well EpsteinCitation32 were believing that one year results were indicative for long term results. However, LetournelCitation33,Citation34 insisted on long follow-up to detect any further degenerative changes. LetournelCitation33,Citation34 found two peaks of failures. Early failures were attributed to imperfect reductions or biological failures such as infection or avascular necrosis, while late failures were due to the inevitable development of osteoarthritis. The first peak occurred within the first three years while the second peak occurred at 10–15 years follow-up.Citation33,Citation34 As 75% of patients included in the study group already passed two years follow-up, i.e. they almost had passed the first peak, a fair comparison to other authors reporting their medium term results (2–10 years) might be permissible. This does not cancel the need to follow this cohort of patients furthermore and to document any further deterioration of the clinical results in the coming reports.
6 Conclusions
We identified two main determinants for the clinical outcome after internal fixation of such fractures: (1) the personality of the fracture determined by the modifiers that reflect the degree of the primary cartilage damage and not by the fracture type and (2) the surgical expertise in achieving a perfect reduction and avoiding complications. Moreover we found that the presence of a posterior wall fracture or an associated pelvic ring injury was bad prognostic factors. Finally, based on our lowered rates of anatomical we could conclude that the learning curve to master these difficult injuries is very steep.
Conflict of interest statement
None were declared for all authors.
Acknowledgements
Thanks to all our patients. Without their compliance and patience this work would not be completed at all. We would like to acknowledge Abu-sheasha G.A., MBBCh, MPH, for her assistance in doing the statistics of this paper.
Notes
Available online 23 January 2012
Peer review under responsibility of Alexandria University Faculty of Medicine.
References
- G.PetsatodisP.AntonarakosB.ChalidisP.PapadopoulosJ.ChristoforidisJ.PournarasSurgically treated acetabular fractures via a single posterior approach with a follow-up of 2-10 yearsInjury3832007334343
- J.E.AlonsoR.DavilaE.BradleyExtended iliofemoral versus triradiate approaches in management of associated acetabular fracturesClin Orthop Relat Res30519948187
- Q.LiuD.WuP.LiS.F.HanSurgical treatment for complex acetabular fracturesChin J Traumatol962006325328
- R.MadhuR.KotnisA.Al-MousawiN.BarlowS.DeoP.WorlockOutcome of surgery for reconstruction of fractures of the acetabulum: the time dependent effect of delayJ Bone Joint Surg Br Vol88920061197
- D.MurphyM.KaliszerJ.RiceJ.P.McElwainOutcome after acetabular fracture: prognostic factors and their inter-relationshipsInjury3472003512517
- H.KinikM.ArmangilExtensile triradiate approach in the management of combined acetabular fracturesArch Orthop Trauma Surg12472004476482
- D.B.GriffinP.E.BeauleJ.M.MattaSafety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulumJ Bone Joint Surg Br Vol871020051391
- M.L.RouttJrM.F.SwiontkowskiOperative treatment of complex acetabular fractures. Combined anterior and posterior exposures during the same procedureJ Bone Joint Surg Am7261990897904
- S.E.PutnisB.M.Dala-aliM.BircherPosterior wall osteotomy to facilitate reduction of complex acetabular fracturesInjury3810200712141217
- C.M.ReinertM.J.BosseA.PokaT.SchachererR.J.BrumbackA.R.BurgessA modified extensile exposure for the treatment of complex or malunited acetabular fracturesJ Bone Joint Surg Am7031988329337
- R.HoffmannU.StockleM.NittingerN.P.SudkampN.P.HaasOperative treatment of complex acetabular fractures through the modified extensile iliofemoral approachUnfallchirurg103120001221
- D.L.HelfetG.J.SchmelingManagement of complex acetabular fractures through single nonextensile exposuresClin Orthop Relat Res30519945868
- U.StockleR.HoffmannN.P.SudkampR.ReindlN.P.HaasTreatment of complex acetabular fractures through a modified extended iliofemoral approachJ Orthop Trauma1642002220230
- J.M.MattaFractures of the acetabulum: accuracy of the reduction and clinical results in patients managed operatively within three weeks after the injuryJ Bone Joint Surg Am78199616321645
- A.GansslenC.KrettekInternal fixation of acetabular both-column fractures via the ilioinguinal approachOper Orthop Traumatol2132009270282
- J.GenuarioK.J.KovalR.V.CantuK.F.SprattDoes hospital surgical volume affect in-hospital outcomes in surgically treated pelvic and acetabular fractures?Bull NYU Hosp Jt Dis6642008282289
- P.V.GiannoudisM.R.W.GrotzC.PapakostidisH.DinopoulosOperative treatment of displaced fractures of the acetabulum: a meta-analysisJ Bone Joint Surg Br Vol87120052
- E.LetournelAcetabulum fractures: classification and managementClin Orthop Relat Res151198081
- A.M.HarrisP.AlthausenJ.F.KellamM.J.BosseSimultaneous anterior and posterior approaches for complex acetabular fracturesJ Orthop Trauma2272008494497
- E.GueradoJ.R.CanoE.CruzSimultaneous ilioinguinal and Kocher–Langenbeck approaches for the treatment of complex acetabular fracturesHip Int20Suppl. 72010210
- J.O.AnglenT.A.BurdK.J.HendricksP.HarrisonThe “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fracturesJ Orthop Trauma1792003625634
- C.C.SchmidtG.S.GruenNon-extensile surgical approaches for two-column acetabular fracturesJ Bone Joint Surg Br7541993556561
- D.C.MearsJ.H.VelyvisC.P.ChangDisplaced acetabular fractures managed operatively: indicators of outcomeClin Orthop Relat Res4072003173186
- B.G.OchsI.MarintschevH.HoyerB.RolauffsU.CulemannT.PohlemannChanges in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU)Injury4182010839851
- U.StockleR.HoffmannM.NittingerN.P.SudkampN.P.HaasScrew fixation of acetabular fracturesInt Orthop2432000143147
- E.LetournelFractures of the cotyloid cavity, study of a series of 75 casesJ Chron Dis82196147
- P.RommensP.IngelfingerT.NowakS.KuhnM.HessmannTraumatic damage to the cartilage influences outcome of anatomically reduced acetabular fractures: a medium-term retrospective analysisInjury2011
- T.PohlemannU.CulemannSummary of controversial debates during the 5th “Homburg Pelvic Course” 13–15 September 2006Injury382007424430
- J.MattaStriving for statistical significance: how important is it?J Trauma142000227229
- J.M.MattaL.M.AndersonH.C.EpsteinP.HendricksFractures of the acetabulum: a retrospective analysisClin Orthop Relat Res2051986230
- C.R.RoweJ.D.LowellPrognosis of fractures of the acetabulumJ Bone Joint Surg431196130
- H.C.EpsteinPosterior fracture-dislocations of the hip: long-term follow-upJ Bone Joint Surg56619741103
- Letournel E, Judet R. In: Elson R, editor. Fractures of the acetabulum. Berlin: Springer; 1993.
- M.BircherResults for treatment for fractures of the acetabulumM.TileJ.F.KellamFractures of the pelvis and acetabulum3rd ed.2005Lippincott Williams & WilkinsPhiladelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo807815