Abstract
Introduction
Current obstetric practice strives to avoid difficult vaginal deliveries. The clinician's skill residing mainly in digital transvaginal examination is a subjective evaluation with several limitations. In recent years many reports have proposed a role for ultrasound in the evaluation of laboring patients.
Aim of the work
The aim of this work was to assess the ability of intrapartum ultrasound to accurately and objectively monitor the progress of normal labor as well as to predict successful vaginal birth.
Material and methods
The current work included 200 full term singleton pregnant women in the active phase of the first stage of labor. All cases were in cephalic presentation and in occipitoanterior position. Per vaginum examination (PV) was first performed followed by transabdominal then translabial ultrasound visualizing the infrapubic plane. Ultrasound parameters were tested for the ability to detect the engagement of fetal head and for the occurrence of vaginal delivery. Several parameters were measured at rest and during the peak of uterine contraction.
Results
70.5% of patients considered PV worse than translabial ultrasound. For a cut-off of 22.3 mm, the dynamic progression distance correctly identified cases that will deliver vaginally with a sensitivity of 74.4% and a specificity of nearly 82.9%. The dynamic angle of progression showed a sensitivity of 85.4% and a specificity of 88.7% at a cut-off of 112° to detect fetal head engagement. A statistically significant correlation was found between cervical diameter assessed using PV examination and using TLUS (r = 0.75, p < 0.001), as well as for the presence of caput and molding of the fetal skull.
Conclusion
Intrapartum ultrasound enabled the objective measurement of birth progress, providing a more scientific basis for assessing labor. This study has demonstrated the feasibility of defining a group of women at high risk of operative delivery.
1 Introduction
Birth represents one of the most important of all the experiences of the human kind. Despite the complexity and sophistication of modern obstetrics it is important to remember the simple objective of every pregnancy, namely the delivery of a healthy baby to a healthy mother. The fullest possible understanding of the birth process, its perturbations and appropriate management policies is central to that objective.Citation1 Current obstetric practice strives to avoid difficult vaginal deliveries. Although being the ‘gold standard’ for obstetric practice, the clinician's skill residing mainly in digital transvaginal examination is a subjective evaluation with several limitations.Citation2
Throughout the last decade, compact, mobile, high-resolution real-time ultrasound machines designed to enable service at the patient's bedside, have become increasingly available. As a result, most labor and delivery services can provide continuous ultrasound availabilities. This technology has become so user friendly that non-ultrasound-trained professionals, can provide high-quality basic ultrasound services.Citation3
In recent years many reports have proposed a role for ultrasound in the evaluation of laboring patients. A growing body of knowledge is accumulating regarding true intrapartum ultrasound, a relatively new application of ultrasound.Citation4 Intrapartum ultrasonography has enabled further understanding of the complex physiology of childbirth. It has been shown to provide objective information on the dynamics of different stages of labor, and may also be used to assess the prognosis for operative vaginal delivery.Citation5,Citation6
Engagement of the fetal head can be used as an ‘internal pelvimeter’ to determine whether the bony birth canal is sufficiently wide for an individual fetus. Assessment of fetal head station with regard to the narrowest part of the maternal bony pelvis is of crucial importance for vaginal delivery to occur. Recent studies have shown that ultrasound imaging might allow dynamic and objective quantification of the level of fetal head descent in the birth canal.Citation2 Various sonographic modalities have been employed in the intrapartum determination of fetal head engagement.Citation5,Citation7–Citation10 Translabial sonography allows a diagnosis of fetal station with an accuracy comparable to that of digital examination and may provide useful information for diagnosing obstructed labor in the second stage as well as assisting in the choice of instrumental delivery.Citation11
Several studies have developed ultrasound based parameters and have studied their evolution over the course of labor both individually and in combination to provide an objective measure of labor progression.Citation2,Citation5,Citation11 Translabial ultrasound imaging might allow the objective quantification of the level of fetal head descent in the birth canal. A “progression distance” of the fetal head was described as the minimal distance from a line through the infero-posterior symphyseal margin (parallel to the main transducer axis) and the leading edge of the fetal skull. The authors provided evidence that this method was highly reproducible and the progression distance correlated well with the station of the fetal head by a combination of abdominal palpation and vaginal digital examination. This measurement may also be of value in determining the progress of the head in the second stage of labor.Citation7 Another of the intrapartum ultrasound based parameters is the ‘angle of progression’ of the fetal head, described as the angle between a line through the midline of the pubic symphysis and a line from the inferior apex of the symphysis to the leading part of the fetal skull.Citation12 Evaluation of this angle showed a good intra- and inter-observer variability for the measurement that was less than 3°.Citation13 Some authors concluded that the measurement of the angle of progression on intrapartum ultrasound imaging is reliable regardless of fetal head station or the clinician's level of ultrasound experience.Citation2 Intrapartum ultrasound imaging might allow the dynamic assessment of the progress of labor with prognostic potentials, and provides a more scientific basis for assessing labor.Citation14
2 Aim of the work
The aim of this work was to assess the ability of intrapartum ultrasound to accurately and objectively monitor the progress of normal labor as well as to predict successful vaginal birth.
3 Material and methods
The current work included 200 pregnant women admitted to the labor ward in the El-Shatby Maternity University hospital, Alexandria, Egypt during the period from May 2010 to May 2011. The patients included 100 primigravidae and 100 multigravidae, all of which were in the active phase of the first stage of labor. The same operator performed all ultrasound studies. Intrapartum ultrasound was always done after the transvaginal examination (by the obstetrician in charge). The managing obstetricians were blinded to the results of the intrapartum ultrasound.
The inclusion criteria were:
Full term singleton pregnancy (37 to 41 full menstrual weeks).
Spontaneous onset of the active phase of labor, as evidenced by the onset of regular rhythmic uterine contractions and dilatation of the internal cervical of beyond 4 cm, as evidenced by clinical examination.
The exclusion criteria were:
Abnormal presentations and positions including occipitoposterior.
Congenital fetal malformations.
Abnormalities of the amniotic fluid and/or placenta.
Maternal spine and/or pelvic disease and/or fractures.
Complicated pregnancies.
Patients attempting vaginal birth after cesarian section (VBAC).
Full history taking and complete clinical examination were undertaken for all participants. Maternal, fetal and birth characteristics of the study group were collected for statistical analysis, including mode and time of delivery. For intrapartum ultrasound as well as for the transvaginal digital examination, the laboring women were placed in a dorsal lithotomy position with their knees and hips flexed. Digital per vaginum examination was first performed by either a senior resident or an attending physician followed immediately by ultrasound done by one of the authors who was aware of the result of the digital exam. A 3.5 MHz curved array ultrasound transducer (Tellus UF-810XTD, FUKUDA company, Tokyo, JAPAN) was used.
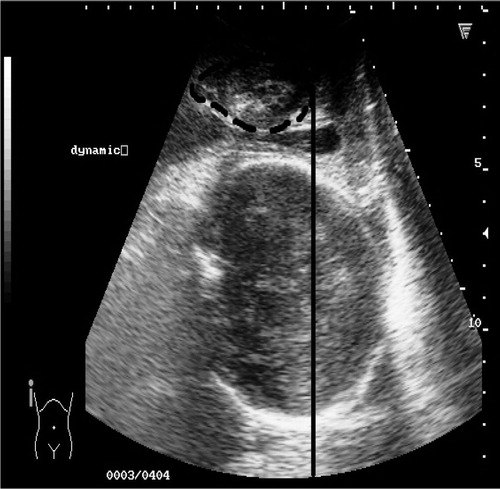
A conventional abdominal obstetrical ultrasound was first performed for fetal well-being and biometry; Biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL) and expected fetal weight (EFW) using Hadlock's formulaCitation15: Then, the probe was positioned translabiallyCitation7 along the sagittal plane (). Using this approach revealed the following anatomical structures: (1) The pubic symphysis joint. For standardization, the transducer was placed so that the symphysis was in a horizontal position. (2) The fetal skull, of which the anterior and lowermost parts were clearly depicted. (3) The dorsal part of the birth canal: soft tissue and sacrococcygeal bones. These structures could not be resolved individually nor with precision because of the acoustic shadowing from the fetal skull.Citation5 The plane encompassing these anatomical structures was referred to as the ‘infrapubic plane’ ().
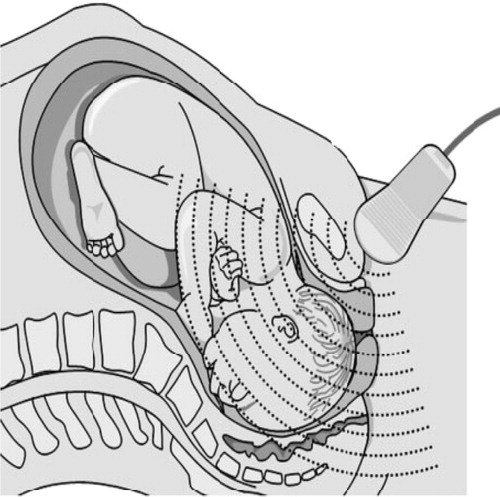
In the infrapubic plane, station of the fetal head within the maternal pelvis was determined by measuring the progression distance described as the minimal distance (in mm) from a line through the infero-posterior symphyseal margin (parallel to the main transducer axis) and the leading edge of the fetal skull.Citation7 In the same plane, the angle of progression of the fetal head, described as the angle between a line through the midline of the pubic symphysis and a line from the inferior apex of the symphysis to the leading part of the fetal skull is measured.Citation12 Lastly, while still in the same plane, the presence of either caput succedaneum, molding of fetal skull bones and the status of the fetal membranes were all noted.Citation3 Turning the probe in a transverse position, a trial was made to depict and measure the cervical diameter as the mean of two orthogonal maximal diameters. Vaginal examinations, as well as translabial ultrasound parameters were taken both at resting and, during a naturally occurring contraction, encompassing one voluntary pushing and gentle fundal pressure.
Data were analyzed using the Statistical Package for Social Sciences (SPSS ver.18 Chicago, IL, USA). Quantitative data were described using mean and standard deviation (SD). Qualitative data were described using number and percent. Comparison of quantitative variables in two groups was conducted using independent t-tests. Association between two qualitative variables (2 × 2) was done using Chi square test and by Fisher's Exact test when less than 25% of cells had expected cell count less than 5 and by Monte carlo significance test if more than 25% of cells had expected cell count less than 5 or more than 2 × 2 categories. Correlation between two quantitative variables was done using Pearson correlation test. ROC curve analysis was done to test the diagnostic performance of certain markers to predict the onset of vaginal birth. Sensitivity was defined as the fraction of parturients who delivered vaginally that the marker correctly identified as positive. On the other hand, specificity was defined as the fraction of people who delivered by cesarean section that the test correctly identified as negative. The area under a ROC curve (AUC) quantifies the overall ability of the test to discriminate between those individuals destined to deliver vaginally and those who did not. In all statistical tests, a level of significance of .05 was used, below which the results were considered to be statistically significant.
4 Results
4.1 Patient characteristics
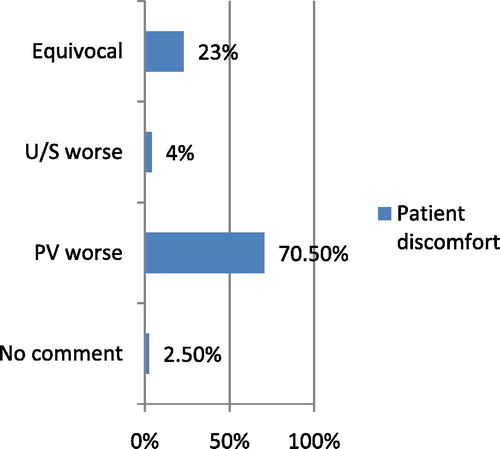
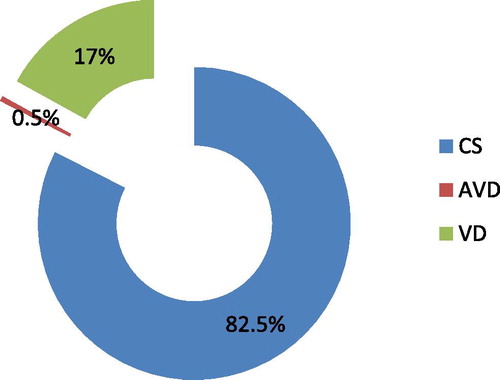
The mean patient age in the studied population was 24.8 ± 5.1 years. The median gravidity was 2, ranging from G1 to G7. The mean gestational age based on the last menstrual period was 39.3 weeks ranging from 37 to 41 weeks of amenorrhea. The mean fetal birth weight was 3223.2 ± 423.5 g with a mean BPD of 9 ± 0.5 cm and only 1% of newborns were admitted to the neonatal intensive care unit (NICU) all following vaginal delivery. The mean cervical dilatation among the studied population – using PV – was nearly 6 cm ranging from 4 to 9 cm dilatation and 62% of patients had their membranes spontaneously ruptured at the time of the first examination. Also, 28.4% of parturients had the fetal head engaged during their first examination. The majority of patients expressed their discomfort toward per vaginum examination (PV) and considered it worse than translabial ultrasound (U/S) as compared to only 4% who felt the opposite. However, around a quarter of patients found both, U/S and PV exam, to be equivocal, . Nearly 82% of patients delivered vaginally as compared to 17% who delivered by CS, and only a single case delivered vaginally using obstetric forceps, .
4.2 Correlations & associations
Using transabdominal ultrasound, 62.1% of all fetuses were in the left dorsoanterior position (LDA). The identification of fetal head position by PV was not possible in 18.5% of all exams, whereas ultrasound was capable of describing fetal position at all times. No significant correlation was found between ultrasound and PV findings regarding fetal position (r = 0.09, p = 0.16). Concerning the fetal membrane status, TLUS showed a sensitivity of around 70.5% in detecting intact membranes with a very high specificity (>95%). The correlation between TLUS and PV in determining the status of fetal membranes was found to be statistically significant (X2 = 122.3, p < 0.001). As regards cervical diameter, a statistically significant correlation was found between the diameter assessed using PV examination and using TLUS (r = 0.75, p < 0.001). Also, clinically assessed cervical dilatation positively correlated with fetal head station assessed by TLUS during the peak of a uterine contraction (r = 0.36, p < 0.001). Caput succedaneum of the fetal head was found in around 47.3% of all PV examinations and was not accessible in 2% of them. Using TLUS, a sensitivity of nearly 97.9% and a very high specificity (>95%) were found. The statistical correlation between PV and TLUS was found to be highly significant (X2 = 193.1, p < 0.00). While assessing the ability of TLUS in determining the presence of molding of fetal skull bones, a sensitivity of only 41.4% but a high specificity of 99.3% were depicted. Moreover, TLUS was well correlated with PV exam reaching a statistically significant level (X2 = 68.786, p < 0.001).
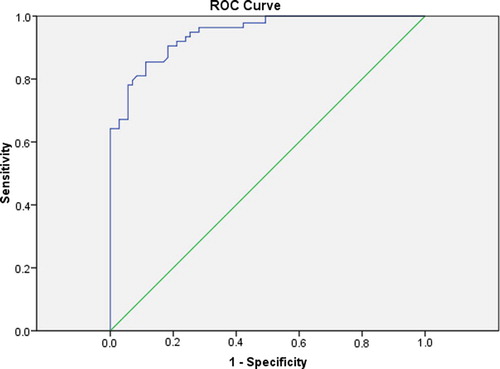
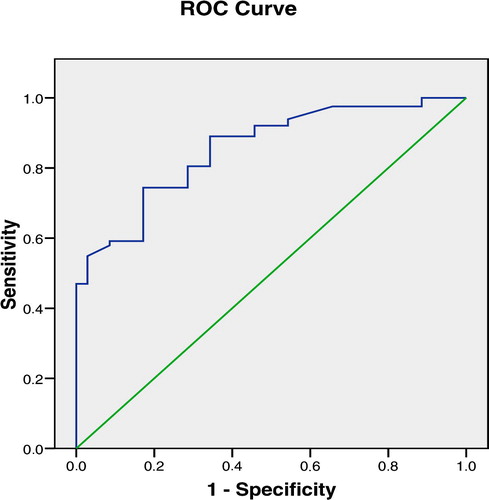
The mean value of the ‘dynamic progression distance’ of the fetal head (=during uterine contraction &/or fundal pressure) was 26.2 ± 17.7 mm. The ROC curve produced showed an AUC = 0.93 at a high level of statistical significance (p < 0.001). The sensitivity and specificity of such a measure would be around 92% and 76.1% respectively for a cut-off of 20.4 mm in detecting fetal head engagement ().
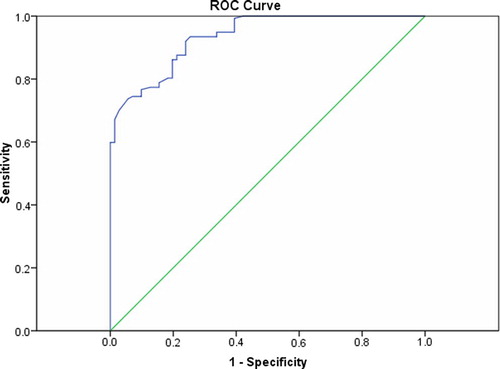
Dynamic angle of progression measurements revealed a mean value of 114.98 ± 19.35°. The corresponding ROC curve showed an AUC of 0.94 reaching a statistically significant level (p < 0.001). Applying this measurement to test the engagement of the fetal head would have a sensitivity of 85.4% and a specificity of 88.7% for a cut-off angle of 112° (). Testing the ‘dynamic progression distance’ of the fetal head to identify patients who will deliver vaginally showed a ROC curve having an AUC of 0.85 with a strong statistical significance (p < 0.001). For a cut-off value of 22.3 mm, such a test will have a sensitivity of 74.4% and a good specificity of nearly 82.9% ().
5 Discussion
Current obstetric practice strives to avoid difficult vaginal deliveries. Although being the ‘gold standard’ for obstetric practice, the clinician's skill residing mainly in digital transvaginal examination is a subjective evaluation with several limitations.Citation2 A growing body of knowledge is accumulating regarding true intrapartum ultrasound, a relatively new application of ultrasound.Citation4 Intrapartum ultrasonography has enabled further understanding of the complex physiology of childbirth. It has been shown to provide objective information on the dynamics of different stages of labor, and has also been used to assess the prognosis for operative vaginal delivery.Citation5,Citation6
In the current work, the majority of patients (70.5%) expressed their discomfort toward per vaginum examination (PV) and considered it worse than translabial ultrasound (TLUS) as compared to only 4% who felt the opposite. This could be regarded as a potential advantage of the technique since intrapartum epidural analgesia is not in routine use in our labor ward.
Using transabdominal ultrasound, 61.9% of all fetuses were in the left dorsoanterior position (LDA) confirming the original observation of Caldwell et al.Citation16 (derived from radiographic studies) that the fetal head usually engages in the occipitotransverse position, more commonly in the left than right position. The identification of the fetal head position by PV was not possible in 18.5% of all exams, whereas ultrasound was capable of depicting fetal position at all times, however no significant agreement was found between the ultrasound and PV examination findings (r = 0.09, p = 0.16). Many studies regarded transvaginal digital examination as being less accurate than ultrasonography for determining the fetal head position during the first stage of labor,Citation17,Citation18 some even demonstrated an overall high rate of error (76%) in transvaginal digital compared with ultrasound determinations of fetal head positioning during active labor.Citation19 A high rate of disagreement between digital examination and ultrasound examination exists, some studies even recommended the routine use of ultrasound in early first stage of labor.Citation17,Citation18,Citation20
Concerning the fetal membrane status, TLUS showed a sensitivity of around 70.5% in detecting intact membranes with a very high specificity (>95%). A strong statistically significant correlation exists between TLUS and PV in determining the status of fetal membranes (X2 = 122.3, p < 0.001). In clinical practice, approximately 10% of cases of PROM require additional confirmation. In case of doubt, a test determining the pH of vaginal secretions and ultrasonography with the assessment of amniotic fluid index may be applied. Visualizing fetal membranes forewater is possible using TLUS and may be helpful in the early stages of cervical dilatation. Some studies even measured the thickness of fetal membranes for the prediction of the risk of preterm birth.Citation21
The mean cervical dilatation among the studied population – using transvaginal examination – was nearly 6 cm ranging from 4 to 9 cm dilatation. A statistically significant correlation was found between cervical diameter assessed using PV examination and that using TLUS (r = 0.75, p < 0.001). The presence of caput succedaneum or intact membranes further enhanced the visualization of the cervix uteri since successful measurement of the cervix was possible in 50% of cases showing either caput or intact membranes as compared to only 25.9% of cases showing neither of them. A paucity of data exists regarding cervical dilatation during the active stage of labor. The general consensus was that, current ultrasound technology fails to provide precise, objective assessment of cervical dilatation throughout the active phase of labor. This probably reflected technical difficulty resulting from a combination of two main factors: the increasing diameter of the advancing cervical dilatation complicated further by the bony structure of the fetal head and the relative thinness of the effaced and dilated cervix.Citation3 However, in a more recent work by Zimerman et al. translabial 3D ultrasonographic measurements of the cervical diameter showed a positive correlation with digital vaginal examinations (r2 = 0.609 p < .001). The author concluded that the assessment of cervical dilatation using 3D ultrasonography during labor is both feasible and reproducible.Citation22
Caput succedaneum of the fetal head was found in around 47.3% of all PV examinations and was not accessible in 2% of them. TLUS showed a sensitivity of nearly 97.9% and a very high specificity (>95%) in detecting caput of the fetal head. The statistical correlation between PV and TLUS was found to be highly significant (X2 = 193.1, P < 0.00). While assessing the ability of TLUS in determining the presence of molding of fetal skull bones, a sensitivity of only 41.4% but a high specificity of 99.3% were depicted. Moreover, TLUS correlated well with PV examination reaching a statistically significant level (X2 = 68.786, p < 0.001). Ultrasonographic depictions of various adaptations of the fetal head to the maternal pelvis, as molding of the fetal head, have been reported since the early nineties.Citation23 Similarly, ultrasonographic reporting of various adaptations of the fetal head to the maternal pelvis as indentation or compression of the fetal parietal bones in association with obstructed labor or with external pressure, the occurrence of both caput succedaneum before complete cervical dilatation and cephalhematomas have all been depicted during labor with accepted sensitivities and specificities.Citation3
In the current work, 83% of patients delivered vaginally as opposed to only 17% who delivered by CS. Assessment of fetal head station with regard to the narrowest part of the maternal bony pelvis is of crucial importance for vaginal delivery to occur. Therefore, engagement of the fetal head can be used as an ‘internal pelvimeter’ to determine whether the bony birth canal is sufficiently wide for an individual fetus.Citation24 Receiver operating characteristic (ROC) curves were produced in an attempt to show the ability of certain TLUS – specific markers to correctly identify engagement of the fetal head with accepted sensitivity and specificity. Moreover, an attempt has been made to test the ability of TLUS – specific markers (that showed a statistically significant difference between vaginal and CS delivery groups), to predict the occurrence of vaginal delivery.
The mean value of the ‘static angle of progression’ was 104 ± 16.6° in cases who delivered vaginally, a value higher than that found in cases delivered by CS (88.3 ± 14°). This difference was of high statistical significance (p < 0.001). The mean value of the ‘dynamic angle of progression’ – measured during the peak of a uterine contraction – was 118.6 ± 17.9° in cases who delivered vaginally, a value also higher than that found in cases delivered by CS (94.7 ± 14°). This difference was of high statistical significance (p < 0.001).
The ‘dynamic progression distance’ showed an area under the curve (AUC) of 0.93 with a stronger statistical significance (p < 0.001). For a cut-off value of 20.4 mm, such a test will have a sensitivity of 92% and a specificity of nearly 76.1% in detecting the engagement of the fetal head. Dietz et al. first described the progression distance of the fetal head in 140 nulliparous pregnant women who were not in labor for the assessment of head engagement. The authors provided evidence that this method was highly reproducible and the progression distance correlated well with the station of the fetal head by a combination of abdominal palpation and vaginal digital examination.Citation7 The dynamic cut-off value set by the current work as a predictor of fetal head engagement (20.4 mm) was near to the results of the original work by Henrich et al.Citation5 where they used three-dimensional CT reconstruction of standard pelvimetric measurements of normal female pelves in correlation with intrapartum ultrasound and confirmed that a line parallel to the infrapubic line and 30 mm caudal to it indicates the level of the ischial spines and hence the plane of fetal head engagement.
The ability of the angle of progression to correctly identify cases with engaged fetal head was illustrated in a previous ROC curve (). ‘Dynamic angle of progression’ showed a low sensitivity but a good specificity of 85.4% and 88.7% respectively for a cut-off angle of 112°; the corresponding ROC curve had a statistically significant AUC of 0.94 (p < 0.001). The results of the current study agreed with the work done by Barbera et al. in which they developed a geometric model from computed tomographic (CT) images and from TLUS. Using this model, they concluded that a TLUS angle of 99° correlated with zero station of the fetal head.Citation25 In the current study, the ‘dynamic’ cut-off for the prediction of fetal head engagement was above 99°. Moreover, cases who delivered vaginally had the mean values for their progression angles (static and dynamic) well above 99° unlike those who delivered by CS.
The ‘dynamic angle of progression’ was shown to have a sensitivity of 63.4% and a specificity of 100% in detecting cases that are meant to deliver vaginally, at a cut-off value of 113.2°. The corresponding ROC curve had an AUC = 0.86 still of high statistical significance (). Nader et al.Citation26 posed the question: ‘Can we predict how labor will proceed?’ There is a clear interest among practitioners in knowing how a delivery will proceed. Dietz et al. reported the possibility of detecting patients at risk of instrumental delivery using intrapartum ultrasound, they used translabial ultrasound before labor to measure head engagement, assessed pelvic organ mobility, and combined these measurements with patient history and other clinical parameters to predict the mode of delivery.Citation6 Some authors even proved ultrasound to be more effective than the traditional Bishop score in the prediction of vaginal delivery.Citation26,Citation27 A series of models have even been developed to classify women into high- and low-risk groups for cesarean section.Citation28 In accordance with the results of the current work, Kalache et al.Citation12 evaluated prospectively this measurement and found a strong relationship between the angle of progression and the need for cesarean delivery. When the angle of progression was 120°, a probability of 90% for either spontaneous vaginal delivery or for a successful vacuum extraction existed. Barbera et al.Citation13 studied the same angle and described a good intra- and inter-observer variability that was less than 3°. Their data showed that an angle of at least 120° was always associated with subsequent spontaneous vaginal delivery. Tutscheck et al.Citation14 concluded that for a dynamic value of >135°, 94% of parturients will deliver vaginally. These figures are close to the dynamic cut-off values of the current work. In his recent work, Torkildsen et al.Citation29 defined an angle of progression of 110° as a cut-off to predict vaginal delivery which occurred in 87% of patients.
6 Conclusion
Vaginal birth is a natural process, but occasionally requires urgent medical intervention to avoid harm to the laboring woman and her unborn child. Intrapartum translabial ultrasound is a simple technique that improves the understanding of normal and abnormal labor, enables the objective measurement of birth progress and provides a more scientific basis for assessing labor.Citation14 Furthermore, the use of ultrasound is of crucial importance in performing a safe operative delivery and can help in the prediction of whether a vaginal delivery would be successful.Citation30
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 9 July 2012
References
- A.CalderNormal labourDewhurst's textbook of obstetrics and gynaecology7th ed.2007Blackwell PublishingLondon4655
- A.M.DuckelmannBCS.A.MichaelisMeasurement of fetal head descent using the ‘angle of progression’ on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertiseUltrasound Obstet Gynecol352010216222
- D.ShererIntrapartum ultrasoundUltrasound Obstet Gynecol.302007123139
- S.AkmalTEK.H.NicolaidesIntrapartum sonography to determine fetal occipital position: interobserver agreementUltrasound Obstet Gynecol.242004421424
- W.HenrichDJI.FuchsIntrapartum translabial ultrasound (ITU): sonographic landmarks and correlation with successful vacuum extractionUltrasound Obstet Gynecol.282006753760
- H.P.DietzLVJ.M.SimpsonPredicting operative deliveryUltrasound Obstet Gynecol272006409415
- H.P.DietzLVMeasuring engagement of the fetal head: validity and reproducibility of a new ultrasound techniqueUltrasound Obstet Gynecol252005165168
- T.M.EggeboGLC.HeienPrediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at termUltrasound Obstet Gynecol272006387391
- T.M.EggeboHCI.OklandUltrasound assessment of fetal head–perineum distance before induction of laborUltrasound Obstet Gynecol322008199204
- D.M.ShererAOIntrapartum assessment of fetal head engagement: comparison between transvaginal digital and transabdominal ultrasound determinationsUltrasound Obstet Gynecol212003430436
- T.GhiFAA.PedrazziG.PiluDiagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasoundUltrasound Obstet Gynecol332009331336
- K.D.KalacheDAS.A.MichaelisTransperineal ultrasound imaging in prolonged second stage of labor with occipito anterior presenting fetuses: how well does the ‘angle of progression’ predict the mode of delivery?Ultrasound Obstet Gynecol332009326330
- A.BarberaPXG.PeruginoA new method to assess fetal head descent in labor with transperineal ultrasoundUltrasound Obstet Gynecol332009313319
- B.TutschekBTF.ChantraineA study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descentBJOG118120116269
- F.P.HadlockHRR.S.SharmanEstimation of fetal weight with the use of head, body, and femur measurements – a prospective studyAm J Obstet Gynecol15131985333337
- W.CaldwellMHD.D’EsopoA roentgenologic study of the mechanism of engagement of the fetal headAm J Obstet Gynecol281934824841
- M.R.ChouKDM.TaslimiVaginal versus ultrasound examination of fetal head position during the second stage of laborAm J Obstet Gynecol1912004521524
- O.DupuisRSD.CorinneFetal head position during the second stage of labor: comparison of digital vaginal examination and transabdominal ultrasonographic examinationEur J Obstet Gynecol Reprod Biol1232005193197
- D.M.ShererMMK.BradleyIntrapartum fetal head position I: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of laborUltrasound Obstet Gynecol192002258263
- I.KawabataNAA.OyaFactors influencing the accuracy of digital examination for determining fetal head position during the first stage of laborJ Nippon Med Sch7762010290295
- F.SeveriBCC.VoltoliniThickness of fetal membranes: a possible ultrasound marker for preterm deliveryUltrasound Obstet Gynecol3222008205209
- A.L.ZimermanSAR.MaymonIntrapartum measurement of cervical dilatation using translabial 3-dimensional ultrasonography. Correlation with digital examination and interobserver and intraobserver agreement assessmentJ Ultrasound Med28200912891296
- S.J.CarlanWLJ.LenseFetal head moulding: diagnosis by ultrasound and a review of the literatureJ Perinatol111991105111
- Lee .C Study designs. In: Introductory biostatistics, 1st edition, John Wiley & Sons publishing: Hoboken, New Jersey. 2003:445–482.
- A.BarberaIFT.BeckerAnatomic relationship between the pubic symphysis and ischial spines and its clinical significance in the assessment of fetal head engagement and station during laborUltrasound Obstet Gynecol3332009320325
- R.NaderSKH.DietzPredicting the outcome of induction of labourAust N Z J Obstet Gynaecol502010329333
- P.BastaniHKF.AbasalizadehTransvaginal ultrasonography compared with Bishop score for predicting cesarean section after induction of laborInt J Womens Health32011277280 [Epub 2011 12.7.11]
- S.RaneGRB.HigginsThe value of ultrasound in the prediction of successful induction of laborUltrasound Obstet Gynecol2452004538549
- E.TorkildsenSKT.EggeboPrediction of delivery mode with transperineal ultrasound in women with prolonged first stage of laborUltrasound Obstet Gynecol201137
- F.S.MolinaK.H.NicolaidesUltrasound in labor and deliveryFetal Diagn Ther2720106167