Abstract
Introduction
Intracerebral hemorrhage (ICH) in children is relatively less common as compared to adults. It could be traumatic or spontaneous.
Objective
There are limited studies about ICH in children. In this study, we analyze the etiology, clinical features, management options and outcome assessment in this population.
Methods
All patients with intracerebral hemorrhage under 18 years of age admitted to the neurosurgery department; Alexandria University Main Hospital and Medical Research Institute over a period of one year (June 2008–May 2009) were subjected to clinical examination, laboratory and radiological investigations and the cause of hemorrhage was determined.
Results
Thirty patients with ICH were included in this study. Age of patients ranged from one month to 17.5 years with a higher predilection in males. Presenting features were symptoms of raised intracranial pressure (60%), deterioration in sensorium (46%), limb weakness (36%) and seizures (30.0%). Trauma was the most common cause of ICH and was found in 13 patients (43%), followed by bleeding diathesis in nine patients (30%), arteriovenous malformation (AVM) in five patients (17%), intracranial tumor in two patients and an aneurysm in one patient. Treatment modalities consisted of: hematoma evacuation, excision of AVM, AVM emobilization, aneurysm clipping, tumor excision, and conservative management. Eleven patients were treated conservatively and 19 patients were treated surgically. The outcome showed: good recovery in 14(47%), fair recovery in seven (23%), poor recovery in seven (23%), and death in two patients (7%).
Conclusions
Trauma is the leading cause of ICH in children. Bleeding diathesis and AVM come next. The initial neurological status of patients, the size, location and underlying pathophysiology of the hematoma are the most important determinants of patient outcome. Intracerebral hemorrhage due to bleeding diathesis was generally associated with a better outcome.
Abbreviations:
1 Introduction
The incidence and prevalence of intracranial hemorrhage is not known. The reported incidence of asymptomatic and symptomatic intracranial hemorrhage varies from study to study probably due to differences in populations studied and differences in the sensitivity and timing of diagnostic imaging used.Citation1–Citation4
Intracerebral hemorrhage may be either traumatic or non-traumatic (spontaneous intracerebral hemorrhage). In the pediatric age group, intracerebral hemorrhage is not common.Citation5
From the most frequent causes for spontaneous intracerebral hemorrhage (SICH) in children are vascular malformations.Citation6–Citation11 Other causes of SICH include: hematological diseases such as coagulopathies or thrombocytopenia, cerebral tumors and rare entities like moyamoya disease, septicemia or drug abuse.Citation12–Citation16 Arteriovenous malformations (AVMs) account for 14%Citation17 to 46%Citation18 of hemorrhagic stroke in children and nearly 50%Citation13 of intraparenchymal hemorrhage.
Hematologic abnormalities are reported to be the major risk factor in 10% to 30% of hemorrhagic strokes in most series. Hematologic causes of intraparenchymal hemorrhage include idiopathic thrombocytopenic purpura (ITP), acute lymphoblastic anemia (ALL), sickle cell anemia (SCA), hemophilia, and coagulopathies.Citation19–Citation24
Brain tumors are also found to be one of the causes of ICH in children with a much lower incidence than previously mentioned causes.Citation25,Citation26
Focal abnormality of brain functions from ICH are site specific and include: motor deficit, sensory deficit, speech problems, cranial nerves palsies, cerebellar manifestations, visual abnormalities and pupillary changes.Citation27,Citation28 Irritability and fits may occur in about 6–9% of intracerebral hemorrhages.Citation29 The hemorrhage may expand within minutes or few hours and act as a solid mass, increasing the intracranial pressure.Citation27
Computed tomography (CT), Magnetic resonance imaging (MRI), Conventional angiography and Computed tomography angiography (CTA) or Magnetic resonance angiography (MRA) may be needed to establish the diagnosis of intracranial vascular anomalies.Citation30 In cases of bleeding in children, the coagulation profile should be checked to exclude coagulation disorders and DIC that may develop as a result of thromboplastin release from the damaged brain tissue.Citation31
Management of ICH in children depends on the location of hemorrhage, the volume of the hematoma, the presence of mass effect, the clinical condition of the patient as well as the etiological factors involved in the bleeding.Citation32–Citation34
2 Patients and methods
This study represents all patients below 18 years of age diagnosed with intracerebral hemorrhage admitted to the neurosurgery department; Alexandria University Main Hospital and Medical Research Institute over a period of one year (June 2008–May 2009). Patients with other forms of intracranial hemorrhage were excluded.
3 Results
The study group consists of 30 patients, 18 boys and 12 girls. The age ranged from one month to 17.5 years with a mean age of 11.0 years. Mean ages were 11.7 and 10.2 years for boys and girls, respectively.
Symptoms included headache (60%), vomiting (43%), impaired consciousness (46%), focal neurological deficits (36%) and convulsions (30%) as shown in . Patients with traumatic ICH, aneurysms and AVMs presented acutely as well as three patients with bleeding diathesis and one patient with a cerebral tumor. Five children were younger than 3 years at the time of onset of bleeding. They presented with non specific symptoms like: deterioration of general condition, increased crying, sleepiness, irritability, feeding difficulty, vomiting and fits.
Table 1 Clinical features in 30 patients with ICH.
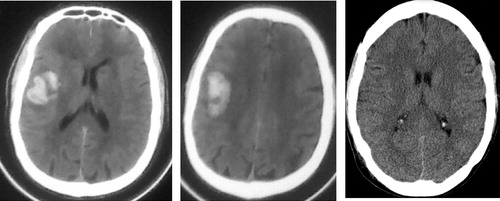
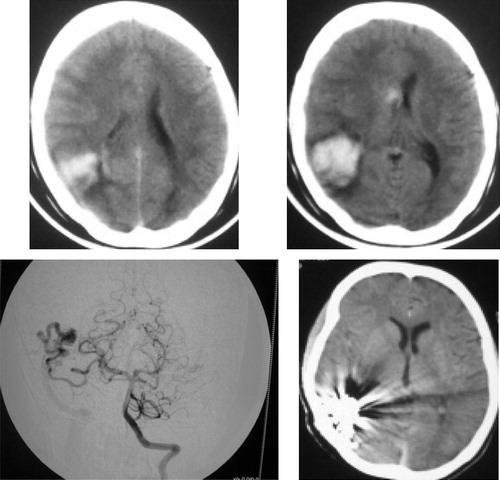
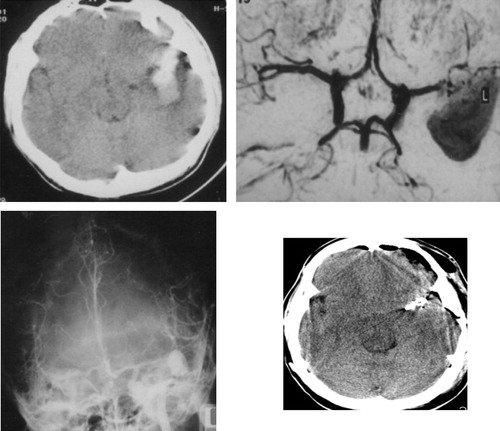
Trauma was the most common cause of ICH, causing hemorrhage in 13 patients (43%), followed by bleeding diathesis in nine cases (30%), AVM in five patients (17%), intracranial tumor in two patients (hemorrhage in pilocytic astrocytoma and posterior fossa tumor) and a middle cerebral artery aneurysm in one patient (–). Nine cases of bleeding diathesis included; three cases of idiopathic thrombocytopenic purpura, three cases with hemophilia, two cases with acute lymphoblastic leukemia and a case of sickle cell anemia (). In the three of cases of ITP, the bleeding was probably due to decrease platelet count. Severe factor VIII deficiency (from 5–15%) was the incriminated factor for ICH in hemophilics. In SCA patient, the severe anemia and thrombocytopenia were the main reasons for ICH. In ALL the main cause of ICH was most probably either anemia or thrombocytopenia or both.
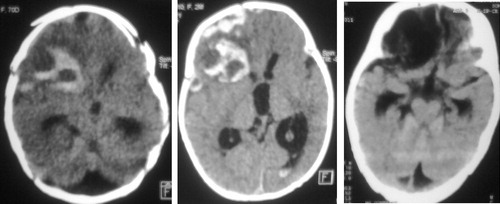
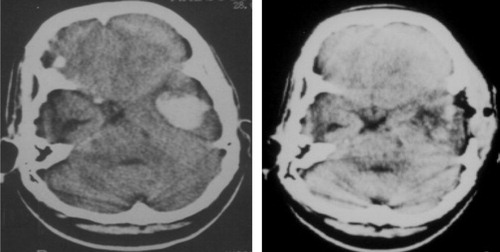
Table 2 Etiology of ICH in our 30 cases.
Computed tomography (CT) was performed in all our patients, CTA in three patients, angiography in seven patients, magnetic resonance imaging (MRI) in twelve and magnetic resonance angiography (MRA) in nine patients.The location of hemorrhage was supratentorial in 24 patients (80%) and infratentorial in six patients (20%) (two brain stem hematoma and four cerebellar hematomas). In supratentorial hematomas, the most common location was lobar in 19 patients, putamenal in two patients, thalamic in two patients and one case with a caudate hematoma (). Intraventricular hemorrhage was associated in six of our patients.
Table 3 Location of ICH.
The treatment was based on the child's presentation, the precipitating cause and the radiological findings. Eleven patients were treated conservatively; five patients with traumatic ICH and six patients with bleeding diathesis. The conservative treatment consisted of; care of the general condition (airway, breathing and circulation), control of the intracranial pressure, antiepileptic measures as well as correction of the underlying coagulation problem. Nineteen patients were treated surgically and consisted of: hematoma evacuation via craniotomy in eight patient and suboccipital craniectomy in three patients, excision of AVM nidus and clipping of feeders in three patients, emobilization of AVM in two patients, aneurysmal clipping in one patient and tumor excision in two patients. Seven patients required an external ventricular drain and three patients required a permanent ventriculo-peritoneal shunt. The average length of hospital stay was 19 days.
The outcome of our patients was classified as good, fair, poor and death. In our series, the outcome of our patients was as follow: good recovery in 14(47%), fair recovery in 7(23%), poor recovery in 7(23%), and death in two patients (7%) ().
Table 4 Outcome of patients.
4 Discussion
This study focuses on ICH in children. We included all children presenting with ICH regardless the etiology (traumatic or non-traumatic). This did not match with what is found in the literature as the majority of studies focused either on traumatic ICH alone as in the Kang et al.Citation35 series or Spontaneous ICH alone as in Beslow et al.Citation36, Meyer-heim and BoltshauserCitation13, Lin et al.Citation3, Al-Jarallah et al.Citation12 and Kumar et al.Citation31 series ().
Table 5 Summary of data from series of ICH in children reported in the literature.
The mean age of our patients was 11.0 years. A male predilction was found with a male to female sex ratio to equal 1.5:1. This was consistent with the Kumar et al.Citation31 series which studied SICH in children as well as the Kang et al.Citation35 series that studied traumatic ICH and showed more prevelance in boys than girls.
In our series, headache, vomiting and impaired conscious level were the main presenting symptoms in older children while those younger than three years old presented mainly with irritability, fits, feeding difficulty, lethargy and sleepiness. LiteratureCitation3,Citation4,Citation12 is quite homogeneous concerning the presenting symptoms in ICH in children.
Trauma was the most frequent cause of ICH in our study group. This finding did not match the results of Meyer-Heim and BoltshauserCitation13, Kumar et al.Citation31 and Lin et al.Citation3 series, in which AVMs represented the major cause of ICH (). This difference can be explained by selection criteria of our patients that included both traumatic and spontaneous cases of ICH, however in their seriesCitation3,Citation13,Citation31 spontaneous ICH was only included.
The second most common cause of ICH in our series was bleeding disorders reported in 30% of the cases. Similarly, Al-Jarallah et al.Citation12 reported bleeding disorders in 32% of his patients. However, this was much higher compared to Meyer-Heim and BoltshauserCitation13 and Kumar et al.Citation31series (). The high incidence of ICH due to bleeding disorders in our series can be explained by high number of children suffering from hematological disorders treated in the Medical Research Institute of Alexandria, a referral center for such cases.
In our series AVMs were the third leading cause of ICH in children seen in 17% of the patients. Hemorrhage is the most frequent clinical presentation of an AVM in adults and children but is more often seen in pediatric patients than in adults.Citation37 In Beslow et al.Citation36 series, AVMS represented the major cause of ICH () however this study did not include cases of trauma and tumors.
It is well known that brain tumors can cause SICH.Citation26 Intracerebral hemorrhage associated with brain tumors is not common and children are rarely involved with this type of hemorrhage.Citation38 In our study ICH caused by tumors was rare and found only in two patients. This was consistent with the series of Meyer-Heim and BoltshauserCitation13 and Kumar et al.Citation31 who showed a similar incidence of ICH due to brain tumors ().
In the present study, an aneurysm was found in only one case and presented with a temporal ICH. This is a much lower incidence compared to Meyer-Heim and Boltshauser seriesCitation13 who found aneurysms in 15% of their cases. This may be due to inclusion of only spontaneous cases of ICH in Meyer-Heim and Boltshauser seriesCitation13 in contrast to our study that included all cases of ICH in children.
In consistence with the findings of Al-Jarallah et al.Citation12 and Meyer-Heim and BoltshauserCitation13, the main location of hemorrhage was supratentorial (). The most common site for supratentorial ICH in the present study was lobar found in 64% of our cases, which was consistent with Lin et al.Citation3 who found lobar ICH in 50% of their cases.
Treatment methodology in the present study was based on the child's clinical presentation, the cause of ICH as well as the radiological criteria of the hematoma. In our study, 11 patients were managed conservatively and 19 cases were managed surgically. These findings were consistent with Meyer-Heim and BoltshauserCitation13 results, where 32% of patients were treated conservatively and 68% were surgically treated (). Kang et al.Citation35 in their series reported a higher incidence of conservative treatment followed in 71% of their patients. Beslow et al.Citation36 reported in their series of spontaneous ICH that conservative treatment was followed in 50% of the cases.
The outcome after intracranial bleeding depends on many different factors such as size and localization of hemorrhage as well as the clinical status at time of presentation. In the present study the outcome of our patients () showed: good recovery in 47%, fair recovery in 23%, poor recovery in 23%, and death in 7%. Al-Jarallah et al.Citation12 in their series found a mortality of 8.8%, where as Lin et al.Citation3 found a mortality of6% ().
5 Conclusion
Trauma is an important cause of ICH in children, alongside bleeding diathesis and AVMs which are the next leading causes. The initial neurological status of the patients beside the size, location and underlying pathophysiology of the hematoma are the most important determinants of the patient's outcome. Intracerebral hemorrhage due to bleeding diathesis was generally associated with a better outcome due to the appropriate diagnosis and treatment of the underlying disease, in addition to early surgical intervention when indicated.
Acknowledgment
We are grateful to our patients, paramedical staff, nurses, laboratory technicians and persons who donated either money or blood substitutes and all who allowed completion of this work.
Notes
Available online 1 April 2012
Peer review under responsibility of Alexandria University Faculty of Medicine.
References
- S.N.GuptaA.M.KechliU.S.KanamallaIntracranial hemorrhage in term newborns: management and outcomesPediatr Neurol402009112
- C.VeiraD.Castro-VilanovaA.FerreiroC.Sanchez-SuarezM.L.CuadradoR.SimonSpontaneous intracranial hemorrhages in childhoodRev Neurol25199713811382
- C.L.LinJ.K.LohA.L.KwanS.L.HowngSpontaneous intracerebral hemorrhage in childrenKaohsiung J Med Sci151999146151
- M.E.May LlanasE.Alcover BlochF.J.Cambra LasaosaJ.Campistol PlanaA.Palomeque RicoNon-traumatic cerebral hemorrhage in childhood: etiology, clinical manifestation and managementAn Esp Pediatr511999257261
- P.StathamN.ToddIntracerebral hematoma: aetiology and hematoma volume determine the amount and progression of brain oedemaActa Neurochirurg511990289
- C.MottoleseM.HermierH.StanA.JouvetG.Saint-PierreJ.C.FromentCentral nervous system cavernomas in the pediatric age groupNeurosurg Rev2420015571
- C.Di RoccoG.TamburriniM.RolloCerebral arteriovenous malformation in childrenActa Neurochir1422000145158
- C.MillarB.BissonetteR.P.HumphreysCerebral arteriovenous malformations in childrenCan J Anaesth411994321331
- K.MoriT.MurataN.HashimotoH.HandaClinical analysis of arteriovenous malformations in childrenChild's Brain619801325
- P.CelliL.FerranteL.PlamaG.CavedonCerebral arteriovenous malformations in children. Clinical features and outcome of treatment in children and in adultsSurg Neurol119844349
- P.LasjauniasInterventional neuroradiology management. Vascular diseases in neonates, infants and children1997SpringerBerlin, Heidelberg pp. 1–53
- A.Al-JarallahM.T.Al-RifaiA.R.RielaE.S.RoachNontraumatic brain hemorrhage in children: etiology and presentationJ Child Neurol152000284289
- A.D.Meyer-HeimE.BoltshauserSpontaneous intracranial haemorrhage in children: aetiology, presentation and outcomeBrain Dev252003416421
- D.I.SandbergM.Lamberti-PasculliJ.M.DrakeR.P.HumphreysJ.T.RutkaSpontaneous intraparenchymal hemorrhage in full-term neonatesNeurosurgery48200110421048
- R.DuhemM.VinchonP.LeblondG.Soto-AresP.DhellemmesCavernous malformations after cerebral irradiation during childhood: report of nine casesChilds Nerv Syst212005922925
- L.C.JordanA.E.HillisHemorrhagic stroke in childrenPediatr Neurol3620077380
- B.ChungV.WongPediatric stroke among Hong Kong Chinese subjectsPediatrics1142004e206e212
- M.GiroudM.LemesleG.MadinierE.ManceauG.V.OssebyR.DumasStroke in children under 16 years of age: clinical and etiological difference with adultsActa Neurol Scand961997401406
- I.BlomE.L.De SchryverL.J.KappelleG.J.RinkelA.Jennekens-SchinkelA.C.PetersPrognosis of hemorrhagic stroke in childhood: a long-term follow-up studyDev Med Child Neurol452003233239
- W.KrivitD.TateJ.WhieIdiopathic thrombocytopenic purpura and intracranial hemorrhagePaediatrics671981570571
- I.TreutigerJ.RajantieB.ZellerDoes treatment of newly diagnosed ITP reduce morbidity?Arch Dis Child922007704
- Hoffbrand A, Muss P, Petit J. Coagulation disorders. Essen Hemat 2006;24:290–302 [5th ed.].
- Ashutosh L, Elliot P. In: Hoffbrand A, Catovsky D. editors. Sickle cell disease in postgraduate hematology, vol. 7. Blackwell publishing, Oxford UK; 2005.
- H.KimJ.LeeJ.ChoiRisk score model for fatal intracranial hemorrhage in acute leukemiaLeukemia202006770776
- E.L.RushingUndiagnosed medulloblastoma presenting as fatal hemorrhage in a 14-year-old boy: case report and review of the literatureChilds Nerv Syst232007799805
- J.P.LaurentD.A.BruceL.SchutHemorrhagic brain tumours in paediatric patientsChild's Brain81981263270
- L.GlantzL.A.EidelmanC.L.SprungSpontaneous intracerebral hemorrhageCritically Ill Pat251Jan. 19996367
- Thomas B. Spontaneous intracerebral hemorrhage. In: Wilkins R, Rengachary S. editors. Neurosurgery, 2nd ed. New York: Mc Graw-Hill companies, Inc; 1985. p. 1511.
- D.I.SandbergM.Lamberti-PasculliJ.M.DrakeR.P.HumphreysJ.T.RutkaSpontaneous intraparenchymal hemorrhage in full-term neonatesNeurosurgery48200110421048
- J.P.BroderickH.P.AdamsJr.W.BarsanGuidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the stroke council. American Heart AssociationStroke301999905915
- R.KumarD.ShuklaA.K.MahapatraSpontaneous intracranial hemorrhage in childrenPediatr Neurosurg45120093745
- J.GaribiG.BilbaoI.PomposoPrognostic factors in spontaneous supratentorial intracerebral hemorrhageBr J Neurosurg1642002355361
- R.W.KirollosA.K.TyagiS.A.RossManagement of spontaneous cerebellar hematomas: a prospective treatment protocolJ Neurosurg49200113781387
- M.ColliceG.D’AlibertiG.TalamontiS.BacigaluppiSurgery for intracerebral hemorrhageNeurol Sci242004S10S11
- J.K.KangC.K.ParkM.C.KimKimDal SooJ.U.SongTraumatic isolated intracerebral hemorrhage in childrenChild's Nerv Syst51989303306
- L.A.BeslowD.J.LichtS.E.SmithP.B.StormG.G.HeuerR.A.ZimmermanA.M.FeilerS.E.KasnerR.N.IchordL.C.JordanPredictors of outcome in childhood intracerebral hemorrhage: a prospective consecutive cohort studyStroke4122010313318
- C.MillarB.BissonetteR.P.HumphreysCerebral arteriovenous malformations in childrenCan J Anaesth411994321331
- K.FujitaS.MatsumotoIntracerebral hemorrhage in brain tumorsNo Shinkei Geka8101980929934