Abstract
Introduction
Cervical disc prolapse is a common disorder that results in spinal cord compression causing myelopathy or nerve root compression causing radiculopathy or both. For a posterolateral cervical disc prolapse causing radiculopathy, the common surgical approach used nowadays is the anterior approach to the cervical column. However, this is associated with many complications; some of them are devastating for example, carotid artery injury and cord injury. Therefore, the use of a simpler approach for the posterolateral disc prolapse is needed. The posterior approach making a keyhole foraminotomy is simpler.
Aim of the work
The aim of this work was to evaluate the role of posterior keyhole foraminotomy for the treatment of cervical radiculopathy caused by posterolateral cervical disc prolapse as compared to the anterior approach for cervical discectomy.
Methods
A retrospective study included 20 patients diagnosed with posterolateral cervical disc prolapse causing radiculopathy and they were divided into two groups each composed of 10 patients, group (1) had cervical anterior discectomy and group (2) had posterior cervical keyhole foraminotomy.
Results
Cervical posterior keyhole foraminotomy (group (2)) had much better results than the cervical anterior discectomy (group (1)). The duration of surgery was shorter in group (2) than in group (1). Also, the postoperative complications including dysphagia, hemiparesis and myelopathy were present only in group (1). The postoperative improvement was better in group (2) than in group (1) and the postoperative hospital stay was shorter in group (2) than in group (1).
Conclusion
As compared to cervical anterior discectomy, cervical posterior keyhole foraminotomy is a safe and effective approach for surgical treatment of posterolateral cervical disc prolapse causing nerve root compression resulting in brachialgia. Cervical keyhole foraminotomy has a shorter duration of surgery, less incidence of complications, less duration of postoperative hospital stay and a better improvement in symptoms.
Keywords:
1 Introduction
Cervical disc prolapse is a common disorder that may compress the spinal cord causing myelopathy or the nerve root causing radiculopathy.Citation1–Citation3 Common current surgical practice for cervical disc prolapse causing radiculopathy is to remove the prolapsed disc through an anterior cervical approach with or without insertion of a graft at the site of the removed disc.Citation4–Citation6 Anterior cervical discectomy with or without fusion has been commonly used for cervical disc disease since the description by Smith and Robinson in 1958.Citation7–Citation9
Anterior approach has many disadvantages. The trajectory to the anterior cervical spine has many important structures, such as the carotid arteries, the oesophagus and the recurrent laryngeal nerves, injury to any of them can cause devastating complications.Citation10–Citation12
Posterior approach has emerged as a better alternative to the anterior approach for the treatment of cervical radiculopathy caused by posterolateral cervical disc prolapse.Citation13–Citation15 The approach is easier with no vital structures in the trajectory to the cervical lamina. It takes less time and is less expensive because it does not require any artificial grafts during the surgery.Citation16–Citation19
2 Aim of the work
The aim of this work was to evaluate the role of posterior keyhole foraminotomy for the treatment of cervical radiculopathy caused by posterolateral cervical disc prolapse as compared to the anterior approach for cervical discectomy.
3 Patients and methods
This was a retrospective study; the data were collected from the archive of patients’ data. This study included 20 patients presented with brachialgia caused by cervical disc prolapse.
The patients were divided into two groups:
Group (1): Ten patients who had anterior cervical discectomy.
Group (2): Ten patients who had posterior keyhole foraminotomy.
Preoperatively, patients were submitted to the following:
Complete history-taking.
Complete general and neurological examination.
Investigations in the form of:
Laboratory investigations.
Radiological investigations, in the form of plain X-ray and magnetic resonance imaging of the cervical spine.
Intraoperatively, 10 patients had anterior cervical discectomy and the other ten patients had posterior cervical keyhole foraminotomy. The C-arm was used as a guide to the correct cervical level in all cases of cervical anterior discectomy but was used in some cases of cervical posterior keyhole foraminotomy according to surgeon's preference. In these cases, identification of the correct level was done by counting the spinous processes starting from C2 spinous process downwards and the level was later confirmed by finding the prolapsed disc that coincides with the MRI findings. The keyhole foraminotomy was done by removing part of the lamina above the prolapsed disc and part of the lamina below the prolapsed disc and widening of the neural foramen of the root using a Kerrison exposing an ample part of the nerve root. The nerve root was then retracted from its axilla, pushing it upwards thus exposing the prolapsed disc, which was then removed using a No. 11 scalpel and a small rongeur.
For cervical anterior discectomy group, insertion of a graft (an autograft from the iliac crest or a synthetic cage graft) at the site of the discectomy was done according to surgeon's preference
Postoperatively, patients were followed clinically for up to six months and radiological follow-up was done when indicated.
The confidentiality of the patients was kept and ethical concerns were met.
3.1 Statistical analysis
Data were presented as numbers and percentages.
4 Results
The most common age group was 18–30 years in both cervical anterior discectomy and cervical keyhole foraminotomy groups and the incidence of patients decreased with advancing age. This was shown in .
Table 1 Age of the patients under study.
As regards the sex of patients, in both patients’ groups, males were more common than females as shown in .
Table 2 Sex of patients under study.
The most common level of cervical disc prolapse was C5–6 (60% in cervical anterior discectomy group and 50% in cervical keyhole foraminotomy group) followed by C4–5 and finally by C6–7. This was shown in .
Table 3 Level of cervical discectomy.
Single cervical level disc prolapse ( and ) was the most common finding as regards the number of levels prolapsed followed by two levels of prolapse and then by three levels of prolapse as shown in .

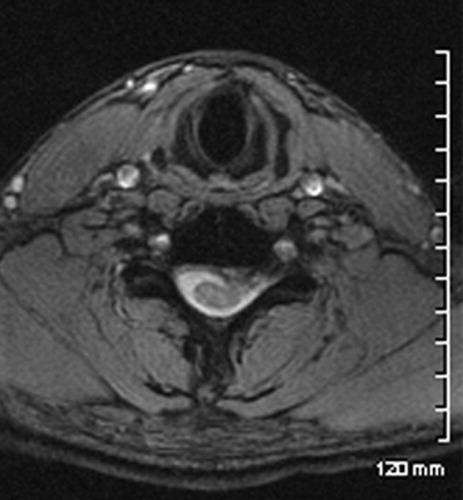
Table 4 Number of levels operated.
The average duration of surgery significantly increased in cervical anterior discectomy group as compared to the cervical keyhole foraminotomy group. Thirty percent of cervical keyhole foraminotomy group had a surgical duration of less than 1 h while none of the cervical anterior discectomy group had this duration. This was shown in .
Table 5 Average duration of surgery.
As regards the postoperative complications, they were significantly more frequent and more serious in the cervical anterior discectomy group than the cervical keyhole foraminotomy group. None of the cervical keyhole foraminotomy group patients had infection, dysphagia, myelopathy or hemiparesis postoperatively as shown in .
Table 6 Postoperative complications.
Postoperative improvement of brachialgia was more pronounced in cervical keyhole foraminotomy group which had a 70% excellent category as compared to 40% excellent category in cervical anterior discectomy group patients as shown in .
Table 7 Postoperative improvement of brachialgia.
The postoperative hospital stay was significantly shorter in cervical posterior foraminotomy group (70% less than two days) than the cervical anterior discectomy group (40% less than two days) as shown in .
Table 8 Duration of postoperative hospital stay.
5 Discussion
Cervical disc prolapse causing brachialgia is a common clinical diagnosis.Citation20,Citation21 Conservative treatment is advocated as a first line therapy. If the patient did not respond to medical treatment, surgical treatment is advocated.Citation22–Citation24 Cervical anterior discectomy has been and is still the commonest approach to excise the prolapsed cervical disc causing nerve root compression manifesting clinically as brachialgia.Citation25–Citation27 This may or may not be associated with insertion of a graft.Citation28,Citation29 However, because of the important anatomical structures encountered in this approach, many complications; some of them are devastating, were reported.Citation30–Citation32 These include oesophageal injury causing fistula formation or mediastinitis which could be fatal, carotid artery injury causing extensive bleeding or brain infarction, recurrent laryngeal nerve injury and spinal cord injury.Citation33–Citation35 This redirected the attention to the posterior cervical approach as a simpler approach for discectomy of the posterolateral cervical disc prolapse to relieve brachialgia.Citation36,Citation37
This study included 20 patients complaining of brachialgia caused by posterolateral cervical disc prolapse causing compression of the nerve root and not responding to conservative treatment. They were divided into two groups each included 10 patients: group (1) was operated by the cervical anterior approach and group (2) was operated using the cervical posterior keyhole foraminotomy approach. Young age group was predominant in our study constituting 60% in group (1) and 50% in group (2) (). This may be because soft disc prolapse causing posterolateral root compression is commoner in young age group.Citation38,Citation39 C5–6 disc prolapse was the commonest in both groups (60% in group (1), and 50% in group (2)) which was in agreement with the literature as regards the commonest cervical disc prolapse level in the populationCitation40 ().
Single level cervical disc prolapse was the commonest (70% in group (1) and 60% in group (2)) followed by two levels and then three levels disc prolapse (). This also was in agreement with statistics in the general population.Citation41 As regards the duration of surgery, there was a significantly lower duration of surgery in group (2) than those in group (1). Surgical duration of less than 1 h was recorded in 60% of cases of group (2) which was not recorded in group (1). One to two hours duration of surgery was present in 30% of cases in group (1) and 60% of cases in group (2), while 70% of cases in group (1) had more than 2 h surgery as compared to 10% of cases in group (2) (). This significantly shorter operative duration in cervical posterior foraminotomy as compared to cervical anterior discectomy is probably due to the shorter trajectory with the absence of significant anatomical structures that required careful dissection and the constant use of the C-arm in all cervical anterior discectomy cases as compared to the infrequent use of the C-arm in the cervical foraminotomy cases. This was in agreement with the results of most other authors.Citation42
As regards the postoperative complications, they were significantly fewer in the cervical keyhole foraminotomy cases as compared to the anterior approach cases. The only complication was neck pain in 20% of cases that resolved after six months of surgery. Otherwise, it was reported that the cervical anterior discectomy had 10% infection rate, 40% neck pain, 30% dysphagia, 20% myelopathy and 10% hemiparesis (). The increased infection rate could be due to the longer operative time. The dysphagia due to oesophageal retraction and the myelopathy was probably due to a tight cervical canal in these two cases causing cord trauma. However, these were temporary and resolved completely after three months of surgery. Excessive retraction on the carotid arteries was probably the cause of infarction causing hemiparesis that improved completely in one case and partially in the other. These results were in agreement to the results of other authors.Citation43
Again, the improvement in brachialgia in group (2) was better than those in group (1). Seventy percent of patients in group (2) had excellent improvement of brachialgia as compared to 40% in group (1). Forty percent of cases in group (1) had fair or poor improvement as compared to only 10% in group (2) (). The better improvement in brachialgia in cervical keyhole foraminotomy approach as compared to cervical anterior discectomy was reported by other authors.Citation18,Citation22,Citation44
Cervical keyhole foraminotomy cases (group (2)) had a shorter postoperative hospital stay than cervical anterior discectomy cases (group (1)). Seventy percent of group (2) had postoperative hospital stay less than two days as compared to 40% in group (1). Sixty percent of cases in group (1) stayed at hospital postoperatively for more than two days as compared to 30% of cases in group (2) (). This difference in the length of postoperative hospital stay was also reported by other authors.Citation15,Citation22,Citation35
From this study we concluded that the cervical posterior keyhole foraminotomy is safer and a more effective approach for surgical treatment of posterolateral cervical disc prolapse causing nerve root compression resulting in brachialgia than the cervical anterior discectomy. Cervical keyhole foraminotomy had a shorter duration of surgery, less incidence of complications, less duration of postoperative hospital stay and a better improvement in symptoms. We recommend the use of cervical posterior keyhole foraminotomy approach as the first choice in cases of posterolateral cervical disc prolapse causing brachialgia.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 21 July 2012
References
- R.A.DavisA long-term outcome study of 170 surgically treated patients with compressive cervical radiculopathySurg Neurol4661996523530 530–3
- C.WoertgenPrognostic factors of posterior cervical disc surgery: a prospective, consecutive study of 54 patientsNeurosurgery4041997724728
- C.P.SilveriCervical disk disease and the keyhole foraminotomy: proven efficacy at extended long-term follow upOrthopedics2081997687692
- G.R.KumarR.S.Maurice-WilliamsR.BradfordCervical foraminotomy: an effective treatment for cervical spondylotic radiculopathyBr J Neurosurg1261998563568
- H.S.AnSpinal disorders at the cervicothoracic junctionSpine1922199425572564
- H.BabaLaminoplasty with foraminotomy for coexisting cervical myelopathy and unilateral radiculopathy: a preliminary reportSpine2121996196202
- H.BabaLaminoplasty following anterior cervical fusion for spondylotic myeloradiculopathyInt Orthop181199415
- T.G.BurkeA.CaputyMicroendoscopic posterior cervical foraminotomy: a cadaveric model and clinical application for cervical radiculopathyJ Neurosurg932000126129
- V.DeboisSoft cervical disc herniation. Influence of cervical spinal canal measurements on development of neurologic symptomsSpine2419199919962002
- N.A.EbraheimThe projection of the cervical disc and uncinate process on the posterior aspect of the cervical spineSurg Neurol5141999363367
- J.P.GrieveResults of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathyBr J Neurosurg14120004043
- P.L.GrundyT.J.GermonS.S.GillTranspedicular approaches to cervical uncovertebral osteophytes causing radiculopathyJ Neurosurg93Suppl. 120002127
- K.KoshuT.TominagaT.YoshimotoSpinous process-splitting laminoplasty with an extended foraminotomy for cervical myelopathyNeurosurgery3731995430434
- S.W.RohEndoscopic foraminotomy using MED system in cadaveric specimensSpine2522000260264
- R.B.SnowH.WeinerCervical laminectomy and foraminotomy as surgical treatment of cervical spondylosis: a follow-up study with analysis of failuresJ Spinal Disord631993245250
- L.C.TanMedial cervical facetectomy for radiculopathy due to foraminal stenosis: 71 personal consecutive casesJ Clin Neurosci631999207211
- N.TanakaThe anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spineSpine2532000286291
- J.S.UllmanM.B.CaminsK.D.PostComplications of cervical disk surgeryMt Sinai J Med6131994276279
- F.P.WirthCervical discectomy. A prospective analysis of three operative techniquesSurg Neurol5342000340346
- C.WoertgenLong term outcome after cervical foraminotomyJ Clin Neurosci742000312315
- YŞÇağlarM.BozkurtG.KahilogullariH.TunaA.BakirF.TorunKeyhole approach for posterior cervical discectomy: experience on 84 patientsMinim Invasive Neurosurg5012007711
- W.D.ParkerCervical laminoforaminotomyJ Neurosurg96Suppl. 22002254261
- R.F.HearyT.C.RykenP.G.MatzP.A.AndersonM.W.GroffL.T.HollyResnick DK; Cervical laminoforaminotomy for the treatment of cervical degenerative radiculopathyJ Neurosurg Spine1122009198202
- T.E.AdamsonThe impact of minimally invasive cervical spine surgery. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004J Neurosurg Spine120044346
- T.G.BurkeA.CaputyMicroendoscopic posterior cervical foraminotomy: a cadaveric model and clinical application for cervical radiculopathyJ Neurosurg932000126129
- J.C.ChangH.K.ParkH.G.BeaS.J.ChoS.K.ChoiP.J.ByunMorphometric measurement of the anatomical landmark in anterior cervical microforaminotomyJ Korean Neurosurg Soc392006340346
- B.H.ChenR.N.NatarajanH.S.AnG.B.AnderssonComparison of biomechanical response to surgical procedures used for cervical radiculopathy: posterior keyhole foraminotomy versus anterior foraminotomy and discectomy versus anterior discectomy with fusionJ Spinal Disord1420011720
- M.J.ClarkeR.D.EckerW.E.KraussR.L.McClellandM.B.DekutoskiSame-segment and adjacent-segment disease following posterior cervical foraminotomyJ Neurosurg Spine6200759
- M.G.FehlingsR.J.GrayPosterior cervical foraminotomy for the treatment of cervical radiculopathyJ Neurosurg Spine102009343344
- R.G.FesslerL.T.KhooMinimally invasive cervical microendoscopic foraminotomy: an initial clinical experienceNeurosurgery512002S37S45
- V.C.GalaJ.E.O’TooleJ.M.VoyadzisR.G.FesslerPosterior minimally invasive approaches for the cervical spineOrthop Clin North Am382007339349
- J.P.GrieveN.D.KitchenA.J.MooreH.T.MarshResults of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathyBr J Neurosurg1420004043
- D.L.HiltonJr.Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imagingSpine J72007154158
- N.HosonoK.YonenobuK.OnoNeck and shoulder pain after laminoplasty. A noticeable complicationSpine21199619691973
- H.IshiharaM.KanamoriY.KawaguchiH.NakamuraT.KimuraAdjacent segment disease after anterior cervical interbody fusionSpine J42004624628
- J.JagannathanJ.H.ShermanT.SzaboC.I.ShaffreyJ.A.JaneThe posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-upJ Neurosurg Spine102009347356
- W.KruppH.SchattkeR.MükeClinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniationActa Neurochir (Wien)10719902229
- J.E.O’TooleK.M.EichholzR.G.FesslerMinimally invasive cervical foraminotomy and decompression of stenosisG.R.ScuderiA.J.TriaMinimally invasive surgery in orthopedics2009SpringerNew York561568
- J.K.RatliffP.R.CooperCervical laminoplasty: a critical reviewJ Neurosurg982003230238
- S.W.RohD.H.KimA.C.CardosoR.G.FesslerEndoscopic foraminotomy using MED system in cadaveric specimensSpine252000260264
- S.RuettenM.KompH.MerkG.GodoliasFull-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled studySpine332008940948
- W.F.SaringerB.ReddyI.Nobauer-HuhmannR.RegatschnigM.ReddyM.TschabitscherEndoscopic anterior cervical foraminotomy for unilateral radiculopathy: anatomical morphometric analysis and preliminary clinical experienceJ Neurosurg982003171180
- L.M.TumialánR.P.PontonW.M.GlufManagement of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusionNeurosurg Focus282010E17
- T.A.ZdeblickD.ZouK.E.WardenR.McCabeD.KunzR.VanderbyCervical stability after foraminotomy. A biomechanical in vitro analysisJ Bone Joint Surg Am7419922227