Abstract
We report a rare case of posterior nut-cracker phenomenon and right adrenal incidentaloma in a young woman who was accurately diagnosed in the outpatient office with the help of the color flow Doppler Ultrasonography, and confirmed by Computed Tomography Angiography (CTA). However, the patient did not have obvious symptoms such as high blood pressure in some adrenal diseases except for occasionally microscopic hematuria and mild waist pain and is still under follow-up.
The posterior nut-cracker phenomenon and adrenal incidentaloma are a rare anomaly in youth. The adrenal incidentaloma is not easy to be perceived in youth while posterior nut-cracker phenomenon is more rare. Posterior nut-cracker phenomenon refers to the compression of the left renal vein (LRV) between the abdominal aorta (AO) and the vertebral column (VC). To our knowledge, coexistence of posterior nut-cracker phenomenon and right adrenal incidentaloma has not been reported in the literature.
1 Case report
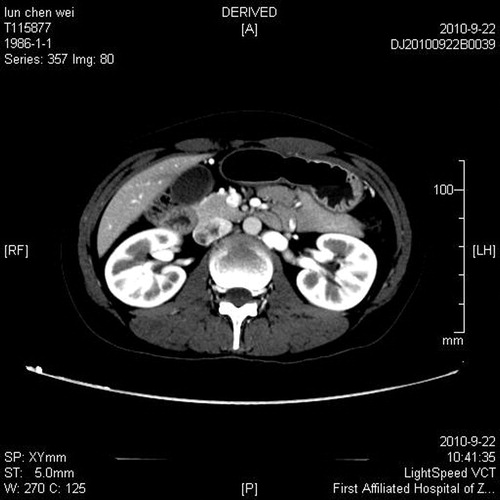
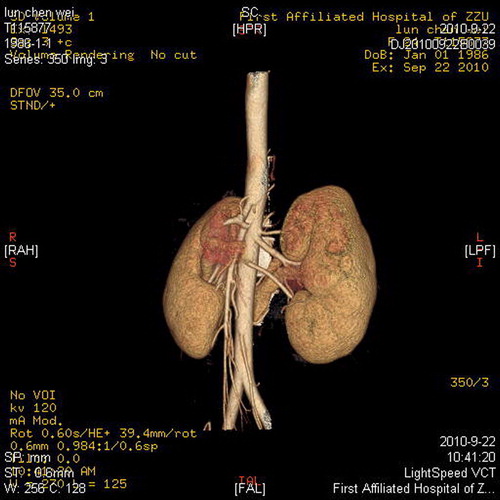
A 24-year-old girl was referred with intermittently mild left flank and abdominal pain, macroscopic hematuria and proteinuria of 5 months duration. The serum electrolyte showed that the K+ (3.25 mmol/L) was slightly lower than normal while others were normal. There were no other symptoms. Physical examination was unremarkable. Hemogram, BUN, and Cr were within normal limits, the urinalysis was normal. This patient underwent the renal Doppler Ultrasound in the supine position. It showed the left kidney was slightly larger than the right (14.4 × 11.4 × 9.0 cm3 VS13.3 × 11.2 × 8.6 cm3) and there was an occupying lesion (3.0 × 2.5 × 2.0 cm3) in the right adrenal area. The vessel diameter and blood peak velocity were measured at 2 points by Doppler ultrasound in the LRV, one at the lateral portion of the LRV near the renal hilus and the other where the LRV courses between the abdominal aorta (AO) and VC. It demonstrated the compression of the LRV between the AO and VC. The anteroposterior (AP) diameters of the LRV of the renal hilus and the compressed portion were 8.0 mm and 2.6 mm, respectively, and the ratio of the diameters was 3.07. Besides, the peak flow velocity in the aortomesenteric portion of the LRV (112.0 cm/s) was found to be significantly greater than that in the hilar portion (23.5 cm/s). The peak velocity ratio between the aortomesenteric and hilar portions was 4.76. Furthermore, the CT scan revealed that the occupying lesion in the right adrenal area originated from the right adrenal with CT value 76Hu, and at the third and fourth lumbar vertebral level the LRV passed through the space between the AO and VC but was significantly compressed (). To confirm the diagnosis computed tomography angiography (CTA) was performed, which demonstrated that the right adrenal incidentaloma was significantly reinforced, and that the LRV was compressed between the AO and VC and had become stenosed, while the distal portion of the LRV was dilated (). From these findings, a diagnosis of the right adrenal incidentaloma and posterior nutcracker phenomenon was made. According to the mild symptoms and will of the patient, the surgical operation was not performed and she is still during follow-up.
2 Discussion
Left renal vein entrapment syndrome, characterized by the compression of the left renal vein (LRV) between the superior mesenteric artery (SMA) and the abdominal aorta was first described in 1950.Citation1 We call this finding anterior nut-cracker phenomenon while regarding that the LRV was compressed between the aorta and the vertebral column the posterior nutcracker phenomenon.Citation2 The phenomenon results in left renal venous hypertension. The syndrome is manifested by left flank and abdominal pain, with or without unilateral hematuria. Other possible symptoms include ‘pelvic congestion syndrome’ characterized by symptoms of dysmenorrhea, dyspareunia, post-coital ache, lower abdominal pain, dysuria, pelvic, vulvar, gluteal or thigh varices and emotional disturbances, midline congestion syndrome, chronic fatigue syndrome and orthostatic dysregulation.Citation3 Diagnosis of nutcracker syndrome includes phase contrast microscopy, abdominal ultrasound and intravenous urography, coagulation profiles, tests for urinary bilharziasis, cystoscopic localization of the hematuria, selective urine cytology, flexible uretero-reno-scopy, renal biopsy, CT/CTA and/or MR angiography, renal vein and inferior vena cava (IVC) phlebography and venous pressure manometry.Citation4 It has been reported that patients suspected of having nutcracker syndrome should undergo computerized tomography angiography (CTA) of the abdomen to delineate the anatomic relation of LRV and other circum-structure near it. The treatment included surveillance, open surgical procedures, intra-pelvic chemical cauterization and intra-or extra vascular stents.Citation5 Marone et al. reported a case of posterior nut-cracker syndrome (PNS) in a 17-year-old woman, who presented with a 2 year history of recurrent hematuria associated with severe left flank and back pain, successfully treated with anterior transposition of the LRV.Citation6 However, our patient was referred with intermittently mild left flank and abdominal pain, macroscopic hematuria and proteinuria of 5 months duration. According to these, we gave the patient a close follow-up without surgical treatment.
Adrenal incidentalomas are defined as no or less clinical endocrine symptoms and signs, and usually were discovered by accident when checking adrenal lesions, which are often subclinical. The prevalence of adrenal incidentaloma has increased with the increasing use of imaging techniques, which on computed tomography (CT) in the general population has been reported to be as high as 4.2%.Citation7 While majority are benign adenoma, a small but significant minority may be primary adrenal carcinoma or have endocrine hypersecretion.Citation8 There are various types in the adrenal incidentalomas, and cystosteatoma is the most common, followed by medullary tumor while the prevalence of malignant tumor is reported to be about 1.2–11%.Citation9 The I-IMBG and adrenal scintigraphy examination play an important role in the identification of adrenal incidentalomas.Citation10 In order to determine whether hypersecretions existed, endocrine examination should be performed before operation. Our patient was a typical case of adrenal incidentaloma, with no obvious symptoms, which was found during the examination of kidney blood vessels. Besides, the patient did not accept a surgery operation. So, this patient is still during follow-up.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 14 August 2012
References
- A.R.El SadrA.MinaAnatomical and surgical aspects in the operative management of varicocelesUrol Cut Rev541950257262
- K.R.L.SharperJ.E.JacksonG.WilliamsThe nutcracker syndrome: an uncommon cause of haematuriaBJU741994144146
- ThomasScholbachFrom the nutcracker-phenomenon of the left renal vein to the midline congestion syndrome as a cause of migraine, headache, back and abdominal pain and functional disorder of pelvic organsMed Hypotheses68200713181327
- Ali-El-Dein B, Osman Y, Shehab El-Din AB, El-Diasty T, Mansour O, Ghoneim MA. Anterior and posterior nutcracker syndrome: a report on 11 cases. Transplant Proc, 2003;35:851–3.
- K.AhmedR.SampathM.S.KhanCurrent trends in the diagnosis and management of renal nutcracker syndrome: a reviewEur J Vasc Endovasc Surg312006406410
- E.M.MaroneD.PsacharopuloA.KahlbergSurgical treatment of posterior nutcracker syndromeJ Vasc Surg542011844847
- C.DavenportA.LiewB.DohertyThe prevalence of adrenal incidentaloma in routine clinical practice [J]Endocrine4020118083
- S.BujawansaD.Bowen-JonesLow investigation rate for adrenal incidentalomas[J]Endocrine402011134136
- L.BarzonM.BoscaroDiagnosis and management of adrenal incidentalomas [J]J Urol1632000398407
- S.MaureaM.KlainC.MainolfiThe diagnostic role of radionuclide imaging in evaluation of patients with non hypersecreting adrenal masses [J]J Nucl Med422001884892