Abstract
Background
This study was carried out to evaluate, compare the clinical utility of delta neutrophil index (DNI) values and lactate-6h-clearance as early indicators for outcome prediction in septic shock patients and to find out and correlate the specificity and sensitivity of each to the patient's mortality.
Methods
The study was carried out in Alexandria Main University Hospital on 53 adult patients with severe sepsis/septic shock after taking an informed written consent and approval of the ethics committee. All patients received all standard therapy and resuscitation measures. Arterial blood samples were obtained for measurement of DNI using an ADVIA 2120 automated cell analyzer. Initial arterial serum lactate level and arterial lactate after 6 h from admission were measured for lactate-6h-clearance calculation. Primary outcome measures were hospital mortality (non-survivors) and discharge or transfer to a general medical ward (survivors). Data were analyzed by SPSS® software using (“t” test and chi-square χ2) P < 0.05 was considered significant.
Results
A total of 53 severe sepsis/septic shock patients were enrolled in the study, patients were (36) survivors and (17) non-survivors. This study demonstrated the reliability of DNI and lactate-6h-clearance as predictors of negative outcome. Variables identified by the backward logistic regression model as significantly correlated with negative outcome were lactate-6h-clearance <15%; (sensitivity, 92.5%; specificity, 85.0%; positive predictive value, 90.0%; and negative predictive value, 88.0%) and DNI value >5.2; (sensitivity, 95.0%; specificity, 90.0%; positive predictive value, 92.0%; and negative predictive value, 95.0%).
Conclusion
Monitoring of lactate-6h-clearance can be used to identify patients with severe sepsis/septic shock at high risk of mortality. DNI may serve as a more useful diagnostic and prognostic marker for early diagnosis of disease severity in patients with severe sepsis/septic shock, it is suggested that, increased DNI value should alert clinicians to apply more aggressive therapy.
1 Introduction
In spite of recent advances in antibiotic therapy and general critical care practices, mortality of patients with severe sepsis/septic shock is still substantial. Many investigators have tried to find reliable biomarkers which are useful for the diagnosis and management of sepsis. Ideally, the biomarker should reflect not only the presence of sepsis, but also its severity. Although several biomarkers have been investigated, no single biologic marker has been shown to reliably identify patient's outcome.Citation1
During stress or infection, less mature neutrophil forms enter circulation, including an increased number of bands. This is referred to as a left-shift, which is defined as an elevated immature/total granulocyte ratio or an elevated neutrophil band count. Recent technological advances have led to specific modern automated cell analyzers that can provide information on leukocyte differentials based on cytochemical myeloperoxidase (MPO) reaction and nuclear lobularity of the white blood cells.Citation1 Delta neutrophil index (DNI), the difference between the leukocyte differentials measured in the MPO channel and those assayed in the nuclear lobularity channel, reflects the fraction of circulating immature granulocytes. DNI has been reported to be significantly associated with mortality in patients with suspected severe sepsis/septic shock in the ICU setting. The data, however, are limited and little is known about the clinical usefulness of DNI in evaluating sepsis severity and in assessing the risk of mortality in severe sepsis/septic shock patients.Citation2,Citation3
Patients with severe sepsis/septic shock may experience ineffective arterial circulation due to the vasodilatation associated with infection or impaired cardiac output, when oxygen delivery fails to meet tissue oxygen demands in critical illness, there is a compensatory increase in oxygen extraction. If the imbalance between oxygen delivery and consumption is uncorrected, the compensatory response is exhausted, resulting in an oxygen debt, global tissue hypoxia, anaerobic metabolism, and increased lactate production. Poorly perfused tissue beds result in global tissue hypoxia, is often found in association with an elevated serum lactate level.Citation4–Citation6 Although the mechanisms are complex, global tissue hypoxia that accompanies severe sepsis and septic shock independently contributes to the systemic inflammatory response leading to endothelial activation, vasodilation, release of inflammatory mediators, and modulation of the coagulation system, all resulting in the multiple organ dysfunction syndrome and death.Citation7–Citation9 Numerous studies have established the use of lactate as a diagnostic, therapeutic, and prognostic marker of global tissue hypoxia in severe sepsis/septic shock patients.Citation6 A serum lactate value greater than 4 mmol/L is correlated with increased severity of illness and poorer outcomes.Citation10,Citation11 The sensitivity and specificity of single lactate concentrations as markers of tissue hypoperfusion have been debated; however, serial measurements or lactate clearance over time may be a better prognostic marker of organ failure and patient's mortality. A huge bulk of research has been focused on lactate production/removal in critically ill patients. Some evidence suggests that persistent elevation in lactate is associated with high mortality rate. It is generally agreed that the longer the lactate levels remain high, the worse the prognosis.Citation12–Citation14
Systemic inflammatory response syndrome (SIRS) was defined as two or more of the following conditions:(a) body temperature >38 °C or <36 °C; (b) leukocytosis (>10,000/μl), leukopenia (<4000/μl), or >10% bands; (c) heart rate >90 beats/min; and (d) respiratory rate >20 breaths/min or PaCO2 < 32 mm Hg. Sepsis was defined as SIRS with proven or suspected microbial etiology. Severe sepsis was defined as sepsis plus sepsis-induced organ dysfunction or tissue hypoperfusion. Septic shock was defined as an acute circulatory failure characterized by persistent arterial hypotension (systolic arterial pressure below 90 mm Hg, mean arterial pressure <60 mm Hg, or a reduction in systolic pressure of >40 mm Hg from baseline despite adequate fluid resuscitation in the absence of other causes of hypotension).Citation15
This study was carried out to evaluate, compare the clinical utility of (DNI) values and lactate-6h-clearance as early indicators for outcome prediction in septic shock patients and to find out and correlate the specificity and sensitivity of each to the patient's mortality.
2 Methods
This prospective observational study was carried out in Alexandria Main University Hospital on 53 adult patients with severe sepsis/septic shock in the Intensive Care Unit (ICU) after taking an informed written consent and approval of the ethics committee. Diagnosis of sepsis was suspected in patients with body temperature above 38°,or less than 36°, heart rate more than 90 beats/min, presence of leucocytosis above 10,000/μl, positive blood culture or presence of radiological findings indicating for pneumonia. All patients received all standard therapy and resuscitation measures to control their condition. Patients with Glasgow Coma Scale (GCS) ⩽8, patients with age <18 years, myocardial infarction, pulmonary edema, hemorrhagic shock, trauma, seizure, pregnancy, do-not-attempt-resuscitation orders, or requiring immediate surgery were excluded from the study. All patients were evaluated by the Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission to the ICU.Citation16 SOFA score was used to evaluate the patients during ICU stay.Citation17
Blood samples for the analysis of DNI and other laboratory parameters were taken within the first 6 h of ICU admission; blood samples for DNI were collected in EDTA tubes. All samples were immediately transported to clinical pathology laboratory department. Blood culture was done as a routine work in ICU to confirm the diagnosis, before the initiation of antibiotic therapy. Determination of DNI assay was performed within 1 h of blood sampling. A specific type of automated cell analyzer (ADVIA 2120 Hematology System, Siemens Healthcare Diagnostics, Forchheim, Germany) was used for calculating DNI. This is a flow cytometry-based hematologic analyzer which has two independent white blood cell (WBC) analysis methods, an MPO channel and lobularity/nuclear density channel. First, after lysis of red blood cells (RBCs), the tungsten-halogen based optical system of the MPO channel measures cell size by forward light scatter, and stain intensity by absorbance, thereby counting and differentiating granulocytes, lymphocytes and monocytes based on their size and MPO content. Second, the laser diode-based optical system of the lobularity/nuclear density channel counts and classifies cells according to size, lobularity, and nuclear density. DNI = [the neutrophil subfraction and the eosinophil subfraction measured in the MPO channel by cytochemical MPO reaction] – [the polymorphnuclear leukocytes (PMN) subfraction measured in the nuclear lobularity channel by the reflected light beam]. The measurement of immature granulocytes included promyelocytes, myelocytes, metamyelocytes and band cells, but not blasts.Citation18
Initial arterial serum lactate level and arterial lactate after 6 h from admission were measured for lactate-6h-clearance calculation [(lactate start – lactate 6 h × 100)/lactate start]. Samples for lactate were centrifuged at low speed (3000 rpm) and serum was frozen at –80 °C until assayed. A positive value denotes a decrease or clearance of lactate, whereas a negative value denotes an increase in lactate after 6 h. Lactate levels were measured in arterial blood using point-of-care blood gas analyzers (Critical Care Xpress, NOVA biomedical, MA, and USA). All measurements were performed according to the manufacturers’ instructions. Duration of the study was 21 days from the admission day. Primary outcome measures were hospital mortality (negative outcome = non survivors) and discharge or transfer to a general medical ward (positive outcome = survivors).
2.1 Statistical analysis
Data were analyzed by using SPSSR software (Statistical package for social science for personal computers) using (t and chi-square X2 tests), data were expressed as mean ± SD and P < 0.05 considered significant.
3 Results
A total of 53 patients admitted to ICUs of Alexandria Main University Hospital were enrolled in the study. There was no significant relation between the admitting diagnosis and the patient's outcome. The predominant admission diagnosis was respiratory tract infection with 52.3% patients presenting in septic shock. Intubations were performed in the ICU in 54.2% of patients and mechanical ventilation was started.
Patients diagnosed as having severe sepsis/septic shock were classified as survivors (36 patients) and non-survivors (17 patients) according to their outcome. Mean time of mortality in non-survivors was 15.7 ± 2.4 days. There were no statistically significant differences between the survivors and non-survivors as regards demographic data; (age, weight, and sex), baseline APACHE II scoring system and GCS ().
Table 1 Baseline clinical characteristics of patients by survival.
As regards blood culture, it was positive in 47.2% in survivors and in 70.6% of non-survivors. A total of 5 species of microorganisms were detected from blood specimens, such as Staphylococcus species (n = 9), Klebsiella pneumoniae (n = 6), streptococcus species (n = 5), Escherichia coli (n = 4), Enterococcus species (n = 4) ().
There were no statistically significant differences between the survivors and nonsurvivors as regards baseline HR, MAP and temperature. Significantly higher SOFA scores were more frequent in non-survivors compared to survivors (P = 0.039) ().
Table 2 Comparisons between survivors and non-survivors as regards; SOFA scores and vital signs.
Hematologic and laboratory variables in relation to DNI and lactate-6h-clearance in patients with severe sepsis/septic shock are summarized in the , in which patients’ results of DNI and lactate-6h-clearance exhibited significant statistical differences in non-survivors compared to survivors more than other hematologic and laboratory variables. Lactate at baseline was not different between survivors and non-survivors but lactate-6h-clearance was significantly less in non-survivor patients compared to survivors (14.72 ± 7.11% vs 36.49 ± 12.11%, respectively; P = 0.001). DNI showed significantly higher values in non-survivors compared with survivors (19.0 ± 3.22% vs 5.2 ± 1.2%, respectively; P = 0.0001) with more significant P value than that of lactate-6h-clearance ().
Table 3 Hematologic and laboratory variables in relation to DNI and lactate-6h-clearance in patients with severe sepsis/septic shock.
DIC incidence was significantly higher in non-survivors compared with survivors (58.8% vs 30.5%, respectively; P = 0.005) with significant elevation of platelet count, prothrombin time and D-dimer ().
The results of the present study showed that the DNI index has implications for the prevalence of overt DIC and mortality in patients with severe sepsis/septic shock ().
Table 4 Correlation between DNI and DIC parameters.
The odds ratio for impaired lactate-6h-clearance is highly significant for the negative outcome but DNI appears superior. The odds ratios of selected risk factors are displayed in ROC curves for DNI, lactate-6h-clearance and initial lactate value. It demonstrates the reliability of DNI and lactate-6h-clearance as predictors of negative outcome. Variables identified by the backward logistic regression model as significantly correlated with negative outcome were lactate-6h-clearance <15%; (sensitivity, 92.5%; specificity, 85.0%; positive predictive value, 90.0%; and negative predictive value, 88.0%) and DNI value >5.2; (sensitivity, 95.0%; specificity, 90.0%; positive predictive value, 92.0%; and negative predictive value, 95.0%) () ().
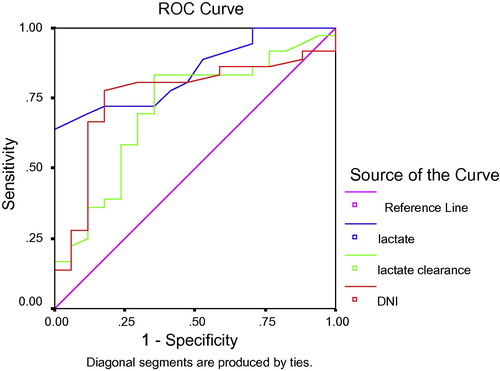
Table 5 Sensitivity and specificity of DNI, lactate and lactate-6h-clearance.
4 Discussion
The pathogenic link between global tissue hypoxia, morbidity, and mortality in sepsis has been thoroughly documented. Lactate represents a useful and clinically obtainable marker of tissue hypoxia and disease severity. Among septic shock patients, only survivors had a significant decrease in lactate concentrations over the course of the disease. In contrast, non-survivors had significantly higher lactate concentrations during both the initial and final phases of shock. The present study extends the concept of lactate normalization during early therapeutic intervention. Our findings suggest that lactate clearance, as defined by the percentage of lactate cleared over the first 6-h period of disease presentation, is an independent variable associated with decreased mortality rate. Patients with high lactate clearance had decreased mortality rates. During resuscitation, a lactate clearance of >15% from its baseline value in as brief a period as 6 h is achievable, when this clearance occurs during the most proximal stages of disease presentation suggests decreased mortality rate.
In this study, a new index of DN was determined using parameters of leukocyte subfractions that were provided by an automated cell analyzer (ADVIA 2120). The DNI, which reflects the number of granulocyte precursors in blood, was obtained by subtracting the fraction of mature polymorphonuclear leukocytes from the sum of MPO-reactive cells. The results of this study showed that DNI was significantly correlated with SOFA score and mortality incidence, DNI values were higher in non-survivors (patients) compared to survivors (patients), the diagnostic value of DNI for severe sepsis/septic shock was superior to lactate, lactate clearance or other laboratory markers. Our results revealed that patients with high DNI >5.2% displayed significant differences in PT, platelet counts, and D-dimer, compared to those with low DNI. These findings suggest that increased DNI may be linked to PT, platelet counts in patients with suspected sever sepsis. These findings suggest that careful attention should be paid not only to overt DIC patients, but also to non-overt DIC subjects, especially those with increased DNI. The optimal cut-off value of DNI for predicting severe sepsis/septic shock was 5.2%. These findings suggest the process of granular leukocyte differentiation starts from immature granulocyte formation, the change in DNI may have preceded the change in absolute numbers of WBC or neutrophil, thus contributing to predicting the development of severe sepsis/septic shock. Thus careful attention may be required in patients with suspected infection for possible concomitant DIC and/or severe sepsis/septic shock if DNI value increases up to 5–6% or more.
Several studies investigated serum lactate level and its association with mortality in patients admitted to the emergency department with severe sepsis.Citation4,Citation10,Citation19–Citation22 The interpretation of single lactate measurement has several limitations, a sepsis patient with hepatic dysfunction may have a higher lactate, also increased lactate concentration may indicate mechanisms other than cellular hypoxia, such as up-regulation in epinephrine-stimulated Na/K-adenosine triphosphatase activity in skeletal muscle and inhibition of pyruvate metabolism or an increase in its production.Citation5 Given these limitations, serial lactate measurements may be more important as an outcome prognostic indicator than a single lactate measurement.Citation23
Bakker et al.Citation24 defined “lactime” as the time during which lactate remains >2 mmol/L and observed that this duration of lactic acidosis was predictive of organ failure and survival. Persistent lactate elevation >6 h is associated with increased mortality rate.Citation5 The present study extends the concept of lactate normalization during early therapeutic intervention. Our findings suggest that lactate clearance, as defined by the percentage of lactate cleared over the first 6-h period of disease presentation, is an independent variable associated with decreased mortality rate.
Nguyen et al.Citation5 concluded that, higher Lactate clearance in the most proximal presentation of severe sepsis and septic shock is associated with improved morbidity and mortality rates, which is consistent with current efforts that emphasize the importance of identifying and treating tissue hypoperfusion during the first 6 h of resuscitation.Citation5
Sean et al.Citation25 concluded that, the systematic monitoring of lactate clearance at 2 h should be clinically useful in cases of acute cardiac or respiratory insufficiency to identify patients at high risk of negative outcome and, potentially, to increase the intensity of the therapeutic approach and finally suggested that, a 2-h lactate clearance >15% is highly predictive of positive outcome and may reassure clinicians that the therapeutic approach is appropriate.
Nguyen et al.Citation26 studied 6 h lactate clearance as a surrogate for the resolution of global tissue hypoxia in sepsis, there was a significant decreased in-hospital, 28-day, and 60-day mortality in the higher lactate clearance quartiles (P < 0.01), It was significantly associated with decreased levels of biomarkers, improvement in organ dysfunction and outcome in severe sepsis and septic shock.
Otero et al.Citation27 compared early lactate clearance with serum biomarkers for outcome prediction in septic shock, there was a statistically significant inverse relationship between patients’ lactate clearance and the mean levels of each biomarker (TNF-α, IL-1 receptor antagonist and caspase-3) over the first 72 h of hospitalization (P < 0.035). There was also statistically significantly higher hospital 28-day and 60-day mortality with decreasing lactate clearance (P < 0.010).
Similar to the results of the present study, Park et al.Citation1 study demonstrated that DNI, which reflects the proportion of immature granulocytes in circulating blood, correlates with disease severity of sepsis in critically ill patients admitted to the medical ICU. For assessing the risk of mortality in severe sepsis/septic shock, DNI may be a better predictive marker than lactate and other leukocyte derived parameters. DNI elevation had 81.3% sensitivity, 91% specificity, 88.6% +ve predictive value and 84.7% −ve predictive value for outcome prediction, while lactate level elevation had 76.7% sensitivity, 57.1% specificity, 61.1 +ve predictive value and 73.7% as a −ve predictive value.
Nahm et al.Citation2 investigated the relationship between calculated immature granulocyte (IG) counts and the severity of sepsis. DNI was strongly correlated with manual IG counts (r = 0.75, P < 0.05). The mortality rate of patients with DNI >40% markedly exceeded the mortality rate of patients with DNI of 5–10% (79% versus 15%, P < 0.05).Their study demonstrated a significant relationship between DNI and DIC-related parameters, including platelet count, PT, PTT, and antithrombin, these findings suggest that DNI may be linked to a hypercoagulable state which is associated with sepsis. Thus they concluded that, DNI has implications for the severity of sepsis and may be valuable to assess the prognosis of patients with suspected sepsis, although the estimation of DNI is limited to the users of one type of cell analyzer.
Kim et al.Citation28 evaluated the clinical significance of DNI in sepsis. DNI values in bacteremic patients were significantly higher in non-survivor (n = 7) than survivor (n = 38) (14.2 ± 12.1% versus 6.7 ± 7.5%, P = 0.03), which indicate that DNI may be useful prognostic marker of bacteremic sepsis.
Lee et al.Citation29 studied the usefulness of DNI as a prognostic marker of sepsis, higher DNI values than that of the present study were observed, patients with DNI >20% showed higher mortality compared to those with DNI <20% (90% versus 33% P = 0.001), 90% +ve predictive value and 67% −ve predictive value for mortality.
Seok et al.Citation30 studied the role of DNI in differential diagnosis and prognosis prediction of patients with sepsis. The best cut-off value for DN for predicting sepsis was 2.7%. DNI was significantly higher in those who died than in the survivors and was identified to be an independent predictor for 28-day mortality in patients with sepsis .They concluded that, DNI may serve as a facile and useful marker for early diagnosis and prognostic assessment of patients with sepsis.
Hye et al.Citation31 investigated DNI as a prognostic marker in patients with bacteremia. The DNI was measured at the onset of bacteremia, at 24 and 72 h later. A total of 102 patients were included in the analysis, and 24 patients died within 28 days. DNI at 72 h after the onset of bacteremia and platelet count at the onset of bacteremia were significantly associated with survival and may be valuable to assess the prognosis of patients with bacteremia.
5 Conclusion
Monitoring of lactate clearance at 6 h can be used to identify critically ill patients with severe sepsis at high risk of mortality. DNI may serve as a more useful diagnostic and prognostic marker for early diagnosis of disease severity in patients with severe sepsis. High levels of DNI may help to identify patients with an impending risk of mortality, it is suggested that, the finding of an increased DNI value should alert clinicians to apply more aggressive therapy.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 29 June 2012
References
- H.B.ParkK.Young AeS.P.MooJ.Won JaiHwanSuK.L.SangDelta neutrophil index as an early marker of disease severity in critically ill patients with sepsisMBC infect dis112011299308
- C.H.NahmJ.W.ChoiJ.LeeDelta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsisAnn Clin Lab Sci3832008241246
- M.A.Ansari-LariT.S.KicklerM.J.BorowitzImmature granulocyte measurement using the Sysmex XE-2100: Relationship to infection and sepsisAm J Clin Pathol12052003795799
- Tim C, Jasper Van B, Jeanette SF, Steven JS, Johan M, Alex P, Sten P, Willemsen, Jan B. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Resp & Crit Care Med 2010;182:752–61.
- B.H.NguyenP.EmanuelRivers, Bernhard P, Knoblich, Gordon J, Alexandria M, Julie A, Ressler A, Michael C. Early lactate clearance is associated with improved outcome in severe sepsis and septic shockCrit Care Med328200416371642
- S.TrzeciakR.P.DellingerM.E.ChanskyR.C.ArnoldC.SchorrB.MilcarekSerum lactate as a predictor of mortality in patients with infectionInt Care Med3362007970977
- A.KarimovaD.J.PinskyThe endothelial response to oxygen deprivation: biology and clinical implicationsInt Care Med2720011931
- C.E.HackS.ZeerlederThe endothelium in sepsis: Source of and a target for inflammationCrit Care Med2920012127
- D.W.LandryJ.A.OliverThe pathogens are of vasodilatory shockN Engl J Med3452001588595
- A.D.NicholE.G.MoritokiP.VilleB.RinaldoB.MichaelC.MichaelRelative hyperlactaemia and hospital mortality in critically ill patients: a retrospective multicentre studyCrit Care120101425
- R.D.PhillipM.L.MitchellM.C.JeanB.JulianM.P.MargaretJ.D.RomanSurviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008Crit Care Med362008296327
- F.ValenzaG.AlettiT.FossaliLactate as a marker of energy failure in critically ill patients: hypothesisCrit Care962005588593
- B.LevyS.GibotP.FranckA.CravoisyP.E.BollaertRelation between muscle Na+K+ ATPase activity and raised lactate concentrations in septic shock: a prospective studyLancet36594622005871875
- Richard Atenion RN, Terri Kress RN. Diagnostic Update Measuring serum lactate Nursing, Crit Care 2009;4(5):56.
- M.M.LevyM.P.FinkJ.C.MarshallE.AbrahamD.AngusD.CookInternational sepsis definitions conferenceCrit Care Med314200312501256
- W.A.KnausE.A.DraperD.P.WagnerAPACHE II: A severity of disease classification systemCrit Care Med131985818829
- Y.B.XingL.M.DaiZ.H.ZhaoZ.W.LiC.LiDiagnostic and prognostic value of procalcitonin and common inflammatory markers combining SOFA score in patients with sepsis in early stageZhongguo Wei Zhong Bing Ji Jiu Yi Xue20120082328
- N.HarrisJ.KunickaA.KratzThe ADVIA 2120 hematology system: flow cytometry-based analysis of blood and body fluids in the routine hematology laboratoryLab Hematol11120054761
- N.I.ShapiroM.D.HowellD.TalmorSerum lactate as a predictor of mortality in emergency department patients with infectionAnn Emerg Med452008524528
- M.A.HermansP.LeffersM.L.JansenY.C.KeulemansM.P.StassenThe value of the mortality in emergency department sepsis (MEDS) score, C reactive protein and lactate in predicting 28-day mortality of sepsis in a Dutch emergency departmentMed J10201011361142
- M.E.MikkelsenA.N.MiltiadesD.F.GaieskiM.GoyalB.D.FuchsC.V.ShahSerum lactate is associated with mortality in severe sepsis independent of organ failure and shockCrit Care Med375200916701677
- R.K.YehJ.J.EunW.U.SangY.S.JiP.J.ManJ.K.HoK.O.JungM.J.KyongInitial lactate level and mortality in septic shock patients with hepatic dysfunctionChest13842010392398
- J.LevrautC.IchaiI.PetitLow exogenous lactate clearance as an early indicator of mortality in normolactatemic critically ill septic patientsCrit Care Med312003705710
- J.BakkerP.GrisM.CoffernilsSerial blood lactate levels can predict the development of multiple organ failure following septic shockAm J Surg1711996221226
- S.SeanA.VittorioG.GiovannaP.FiorellaS.FernandoTwo-hour lactate clearance predicts negative outcome in patients with cardiorespiratory insufficiencyCrit Care Res & Pract10201011551161
- H.B.NguyenM.LoombaJ.J.YangG.JacobsenK.ShahH.ParekhEarly lactate clearance is associated with biomarkers of inflammation, coagulation, apoptosis, organ dysfunction and mortality in severe sepsis and septic shockJ Inflamm (Lond).28201067
- R.OteroE.RiversH.NguyenM.LoombaG.JacobsenThe association of early lactate clearance with inflammatory biomarkers in severe sepsis and septic shockCrit Care Med10200683
- H.Y.KimN.S.LeeO.KwonY.K.KimY.UhJ.LeeClinical significance of delta neutrophil index in patients with sepsisEur Soc of Clin Micro & Infect Dis7Suppl2011
- S.J.LeeS.N.LeeM.K.LeeJ.H.KimS.J.YougK.C.ShinDelta neutrophil index and disease severity of patients with sepsisEur Soc of Int Care Med16Suppl2010
- Y.SeokJ.R.ChoiJ.KimY.K.KimJ.LeeJ.SongDelta Neutrophil Index (DN): A Promising Diagnostic and Prognostic Marker for SepsisShock3732012242246
- W.K.HyeJ.J.SungH.H.SangY.C.JunM.K.JuneG.S.YoungDelta neutrophil index: Could it predict mortality in patients with bacteraemia?Scand J Infect Dis2012 Feb19