Abstract
Introduction
Meningioma is a common benign intracranial tumor. The most common histological subtypes are the transitional and mesothelial subtypes. It can be cured by adequate excision, which is mostly measured by the Simpson grading system. Meningioma can have a peritumoral edema seen in the preoperative computerized tomography as well as in magnetic resonance imaging. It is caused by the release of vasogenic factors that causes leak of fluid from the blood vessels into the brain parenchyma. Recurrence of meningioma has been linked to the presence of preoperative peritumoral brain edema.
Aim
The aim of this study is to predict the possibility of meningioma recurrence based on the extent of brain edema in the preoperative computerized scanning of the brain.
Methods
Twenty five patients with supratentorial meningioma were retrospectively studied for the relationship between preoperative peritumoral brain edema as measured by the brain edema index and the recurrence of meningioma.
Results
The age of the patients ranged from 26 to 69 years. Males and females had almost equal percentages. Most of the cases recurred within a period from 3 years to less than 6 years; while the least recurrence occurred within one year of the surgery. Most of the cases of recurrent meningioma had high brain edema index. The higher the brain edema index, the less average years required for recurrence. The higher the preoperative brain edema index, the higher the possibility of postoperative complications. Tumors at a maximum diameter of three to less than six cm represented the majority of cases. Peritumoral brain edema was present in all cases in sphenoid ridge and parasagittal site.
Conclusion
Preoperative brain edema as measured by brain edema index on the preoperative brain computerized tomography scan had an important impact on the postoperative complication rate as well as on the incidence of tumor recurrence.
Keywords:
1 Introduction
Meningioma is the most common benign intracranial tumor.Citation1 It is an extra-axial tumor that arises from the arachnoid cap cells. It has different locations including parasagittal, olfactory groove, convexity, falcine and posterior fossa locations.Citation2 Histologically, the most common types are the transitional and mesothelial subtypes. Other histological subtypes are the angiomatous, chordoid and anaplastic.Citation3 According to the WHO classification, meningioma can be of type I, which is the benign form, type II usually referred to as the atypical meningioma and type III, which is the malignant meningioma.Citation4 Meningioma is mostly a benign tumor that can be cured completely with surgical resection. The extent of surgical resection is classified according to the Simpson grading system.Citation5
Meningioma recurs in about 20–30% of cases.Citation6 Studying factors that cause tumor recurrence is important because meningioma can be cured with the proper surgical intervention. Factors that determine recurrence of meningioma include the extent of tumor resection according to the Simpson grading system; which is the most important factor, histology of the tumor, location of meningioma, age, gender, signal intensity in the T2-weighted image in the preoperative MRI, vascularity of the tumor, the shape of the tumor surface, the arachnoid plane between the tumor and the brain surface as well as the presence of preoperative peritumoral brain edema.Citation7–Citation9
Peritumoral brain edema was found to be present in almost 60% of supratentorial meningioma cases. Studies were done to determine factors that cause brain edema in meningioma.Citation10–Citation14 The pathophysiology of development of peritumoral brain edema was related to the secretion of vascular endothelial growth factor by the tumor into the adjacent parenchyma of the brain causing vasogenic brain edema. Also the presence of cortical-pial blood supply of the tumor was related to the presence of brain edema.Citation15–Citation17,Citation1
Studying the extent of preoperative peritumoral brain edema (PTBE) in meningioma is important since brain edema was found to have a correlation with tumor recurrence.Citation3,Citation5,Citation7,Citation10 In this study, we tried to find the relationship between the preoperative PTBE and the incidence of tumor recurrence by retrospectively studying cases of meningioma that recurred during the follow-up period.
2 Aim of the study
The aim of this study was to detect any correlation between the presence of preoperative brain edema in supratentorial meningioma and the incidence of recurrence of meningioma.
3 Materials and methods
This was a retrospective study where data were collected from the patients’ archives. This study included 25 patients diagnosed with supratentorial brain meningioma. Any age and both sexes were included in the study.
3.1 All patients were submitted to the following
3.1.1 Preoperatively
Complete history taking.
Complete general and neurological examination.
Investigations; laboratory and radiological in the form of computerized tomography scanning and magnetic resonance imaging of the brain both with and without contrast.
Preoperative computerized tomography scan was used to determine the extent of peritumoral brain edema using the brain edema index. The brain edema index was calculated by dividing the diameter of the parenchymal edema at the axial cut where the maximal tumor diameter was present by the maximal tumor diameter.
Patients who had their meningioma invading and obstructing the draining veins or sinuses radiologically or observed during surgery were excluded from the study to avoid the confusion whether the brain edema was caused by vascular outflow obstruction or by tumor cells invading the brain parenchyma.
Intraoperatively, patients had craniotomy to remove the meningioma totally. No significant vascular injury occurred in the study cases intraoperatively.
Postoperatively, biopsy was sent for histopathological analysis and patients were followed-up clinically for up to five years with follow-up computerized scanning of the brain with contrast every six -months.
The confidentiality of patients’ data was kept.
Statistical analysis: Numbers and percentages were used to describe the results.
4 Results
The age of the patients ranged from 26 to 69 years. The age range from 40 to less than 60 years represented the majority of patients. This is shown in .
Table 1 The age category of patients under study.
As regards the gender of patients, males and females were almost equal as shown in .
Table 2 The gender of patients under study.
Most of the cases (52%) recurred within a period from 3 years to less than 6 years after the surgery; while the least recurrence occurred within one year of the surgery (12%). This is shown in
Table 3 The number of years since surgery till recurrence in patients under study.
Most of cases of recurrent meningioma had a high preoperative brain edema index as shown in .
Table 4 The brain edema index in patients.
The higher the brain edema index, the less average years required for recurrence as shown in .
Table 5 The relationship between the preoperative brain edema index and the average years since surgery to recurrence.
The higher the preoperative brain edema index, the higher the possibility of postoperative complications as shown in .
Table 6 The relationship between the preoperative brain edema index and the number of patients with postoperative complications.
Postoperative weakness (71.4%) followed by transient deterioration of consciousness (50%) were the most common postoperative complications as shown in .
Table 7 The most common postoperative complications reported in patients under study.
Tumors at a maximum diameter of three to less than six cm represented the majority of cases and it was found that the larger the tumor size, the higher the incidence of peritumoral brain edema as shown in .
Table 8 The relationship between the maximum diameter of the tumor and the surrounding brain edema.
Sphenoid ridge meningiomas were the most common of the recurrent meningiomas. Peritumoral brain edema was present in all cases under study in sphenoid ridge ( and ) and parasagittal sites as shown in followed by convexity meningioma (, and ).
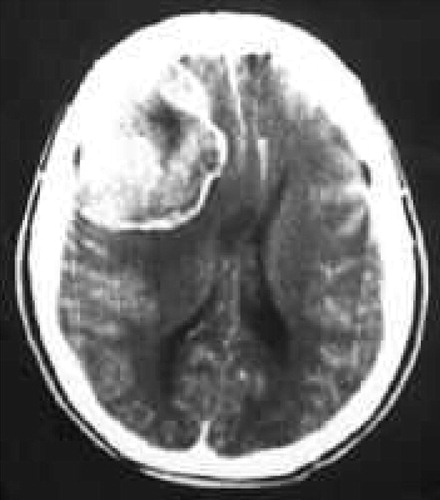
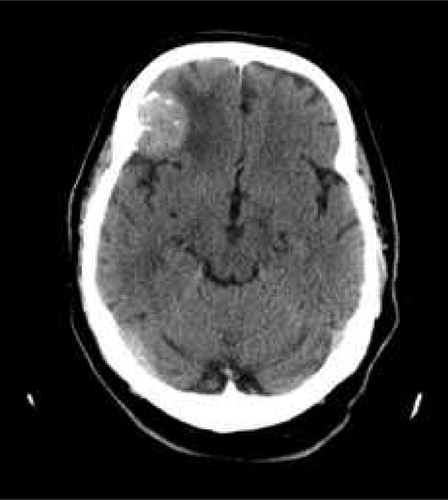



Table 9 The relationship between the site of the tumor and the number of cases with brain edema.
The higher the histological grade of the meningioma, the more the preoperative brain edema index, the more difficult the tumor excision and the more the postoperative complications as shown in .
Table 10 The correlation between the histopathological subtype of meningioma, preoperative brain edema index, ease of tumor excision and postoperative complications.
5 Discussion
This was a retrospective study of 25 patients having recurrent meningioma that tried to correlate the presence of preoperative peritumoral brain edema before the first surgery to the incidence of tumor recurrence. All cases included in the study had Simpson gradeCitation6 one or two of tumor excision at the first operation.
Meningioma is mostly a benign tumor that can be cured by total surgical excision.Citation11,Citation13 However, recurrence occurs in almost 20% of cases.Citation14,Citation18 Many factors were linked to recurrence including gender, age, shape of the tumor surface, peritumoral brain edema and before all, the extent of tumor excision according to the Simpson grading system.Citation17,Citation19,Citation20 Peritumoral brain edema is present in almost 60% of cases of supratentorial meningioma. It is caused by the secretion of vascular endothelial growth factor by the tumor and is closely associated with the presence of cortical pial blood supply of the tumor.Citation21–Citation23 Some reports imply the role of tumor cell invasion of the adjacent brain parenchyma, and this is associated with loss of the arachnoid plane between the tumor and the brain.Citation24–Citation26
In this study, most of the patients (72%) were in the age category of 40–60 years which correlated with most other studies.Citation27 Females were more than males in our study, which also correlates with other statistics.Citation28 Our study showed that the more the number of years since surgery, the higher the incidence of meningioma recurrence. Three to less than six years since surgery represented the highest category (52%) of cases; while the least recurrence was less than one year of surgery. We used the brain edema index in this study which was calculated by dividing the diameter of the brain edema in the preoperative computerized tomography scan at the cut that showed the largest tumor diameter by the tumor diameter at the same scan. We found that the more the brain edema index, the higher the incidence of recurrence (. Also the average years since surgery till recurrence decreased significantly with the increase in brain edema index ().
Brain edema had also an important impact on the incidence of occurrence of postoperative complications. Patients with preoperative brain edema index of two and more had an almost 73% complications rate as compared to 33% complications rate in patients who had brain edema index of less than one (). This was probably due to the loss of arachnoid plane due to tumor invasion of the brain parenchyma in patients with high preoperative brain edema index. The loss of arachnoid plane during tumor dissection from the brain tissue caused brain injury and hence postoperative complications. These results correlate with most other studies.Citation29
Post operative complications were mainly weakness in 71% of cases, transient deterioration of consciousness in 50% of cases and seizures in almost 29% of cases ().
Our study showed that most of the cases had a maximum tumor size of 3 to less than 6 cm (48%) and that the larger the tumor size, the higher the incidence of preoperative peritumoral brain edema (). This was probably caused by the deeper invasion of tumor cells in the brain parenchyma in larger tumors which had a longer duration of growth, hence more time for tumor cells invading the brain. The deeper tumor cell invasion caused more secretion of vascular endothelial growth factor that caused more parenchymal brain edema. This correlated with other studies that indicated a higher incidence of peritumoral brain edema with larger tumor size.Citation30–Citation32
Sphenoid ridge meningioma (44%), followed by parasagittal meningioma (24%) represented the most common locations for recurrent meningioma in our study and both of them had preoperative peritumoral brain edema in all cases (). This corresponds with other studies that indicate that most cases of meningioma that had peritumoral brain edema were in the sphenoid ridge location.Citation33,Citation34
The higher the histological grade of the meningioma, the more the preoperative brain edema index, the more difficult the tumor excision and the more the postoperative complications as shown in . As expected, the more malignant the histopathological subtype of the tumor, the more the tumor invasion of the brain parenchyma and therefore, loss of the arachnoid plane surrounding the meningioma results in more difficult tumor excision and therefore, more postoperative complications.Citation12,Citation1,Citation29
At six months postoperatively, CT follow-up of the brain with contrast was done, and the brain edema was reported. Three cases in this study did not have preoperative peritumoral brain edema and remained so six months postoperatively. All the other cases that had preoperative peritumoral brain edema still had the edema 6 months postoperatively though to a lesser extent. This indicates the still persistent secretion of vasogenic brain edema factor by the remaining tumor cells in the brain parenchyma.
From this study, we concluded that preoperative brain edema as measured by brain edema index on the preoperative brain computerized tomography scan had an important impact on the postoperative complication rate as well as on the incidence of tumor recurrence. The more the preoperative peritumoral brain edema, the more the postoperative complication rate, the more the incidence of tumor recurrence and the less the duration needed for the tumor to recur. We recommend a careful surgical technique in removing meningiomas having high brain edema index and close follow-up postoperatively for these cases especially those in sphenoid ridge or parasagittal locations for early detection of tumor recurrence.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 28 July 2012
References
- T.AbeP.M.BlackR.G.OjemannW.E.HedleyCerebral edema in intracranial meningiomas: evidence for local and diffuse patterns and factors associated with its occurrenceSurg Neurol421994471475
- H.H.SchmidekMeningiomas and their surgical management1991WB SaundersPhiladelphiap.56–62
- A.MahmoodD.V.CaccamoF.J.TomecekG.M.MalikAtypical and malignant meningiomas: a clinicopathological reviewNeurosurgery331993955963
- A.MahmoodN.H.QureshiG.M.MalikIntracranial meningiomas: analysis of recurrence after surgical treatmentActa Neurochir (Wien)12619945358
- T.InamuraS.NishioI.TakeshitaS.FujiwaraM.FukuiPeritumoral brain edema in meningiomas-influence of vascular supply on its developmentNeurosurgery311992179185
- H.HiyamaO.KuboY.TajikaT.TohyamaK.TakakuraMeningiomas associated with peritumoural venous stasis: three types on cerebral angiogramActa Neurochir (Wien)12919943138
- M.IdeM.JimboM.YamamotoY.UmebaraS.HagiwaraO.KuboMIB-1 staining index and peritumoral brain edema of meningiomasCancer781996133143
- F.M.SalpietroC.AlafaciS.LucernaD.G.IacopinoC.TodaroF.TomaselloPeritumoral edema in meningiomas: microsurgical observations of different brain tumor interfaces related to computed tomographyNeurosurgery351994638641
- M.SindouM.AlaywanRole of pia mater vascularization of the tumor in the surgical outcome of intracranial meningiomasActa Neurochir (Wien)13019949093
- M.BitzerL.WockelA.R.LuftA.K.WakhlooD.PetersenH.OpitzThe importance of pial blood supply to the development of peritumoral brain edema in meningiomasJ Neurosurg871997368373
- C.K.GoldmanS.BhararaC.A.PalmerJ.VitekJ.C.TsaiH.L.WeissBrain edema in meningiomas is associated with increased vascular endothelial growth factor expressionNeurosurgery40199712691277
- S.N.KalkanisR.S.CarrollJ.ZhangA.A.ZamaniP.M.BlackCorrelation of vascular endothelial growth factor messenger RNA expression with peritumoral vasogenic cerebral edema in meningiomasJ Neurosurg85199610951101
- J.ProviasK.ClaffeyL.DelAguilaN.LauM.FeldkampA.GuhaMeningiomas: role of vascular endothelial growth factor/vascular permeability factor in angiogenesis and peritumoral edemaNeurosurgery40199710161026
- K.SamotoK.IkezakiM.OnoT.ShonoK.KohnoM.KuwanoExpression of vascular endothelial growth factor and its possible relation with neovascularization in human brain tumorsCancer Res55199511891193
- D.R.SengerL.Van de WaterL.F.BrownJ.A.NagyK.T.YeoT.K.YeoVascular permeability factor (VPF, VEGF) in tumor biologyCancer Metastasis Rev121993303324
- K.J.KimB.LiJ.WinerM.ArmaniniN.GillettH.S.PhillipsInhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumor growth in vivoNature3621993841844
- S.TakanoY.YoshiiS.KondoH.SuzukiT.MarunoS.ShiraiConcentration of vascular endothelial growth factor in the serum and tumor tissue of brain tumor patientsCancer Res56199621852190
- W.G.RobertsG.E.PaladeIncreased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factorJ Cell Sci108199523692379
- J.L.D.AtkinsonJ.I.LaneFrontal sagittal meningioma: tumor parasitization of cortical vasculature as the etiology of peritumoral edema. Case ReportJ Neurosurg811994924926
- J.De VriesA.K.WakhlooCerebral edema associated with WHO-I, WHO-II, and WHO-III-Meningiomas: correlation of clinical, computed tomographic, operative and histological findingsActa Neurochir12519933440
- M.IdeM.JimboO.KuboPeritumoral brain edema and cortical damage by meningiomaActa Neurochir Suppl601994369372
- F.M.SalpietroC.AlafaciS.LucernaPeritumoral edema in meningiomas: microsurgical observations of different tumor interfaces related to computed tomographyNeurosurgery351994638642
- AndreSimisPaulo Henrique.Pires de AguiarClaudia.C.LeitePedro AugusttoSantanaJr.Manoel JacobsenTeixeiraPeritumoral brain edema in benign meningiomas: correlation with clinical, radiologic, and surgical factors and possible role on recurrenceNeurosurgery7052008471477
- WalterStummerMechanisms of tumor-related brain edemaNeurosurgery225200717
- S.OlearyW.AdamsR.ParrishW.MukonoweshuroAtypical imaging appearances of intracranial meningiomasNeurosurgery62120071017
- Jorge.E.AlverniaMarc.P.SindouPreoperative neuroimaging findings as a predictor of the surgical plane of cleavage: prospective study of 100 consecutive cases of intracranial meningiomaNeurosurgery10032004422430
- M.A.KampK.BeseogluS.EickerH.SteigerD.HAnggiSecretory meningiomas: systematic analysis of epidemiological, clinical, and radiological featuresNeurosurgery15332011457465
- Fumiyuki.YamasakiHiroyuki.YoshiokaSeiji.HamaKazuhiko.SugiyamaKazunori.AritaKaoru.KurisuRecurrence of meningiomasNeurosurgery895200011021110
- R.E.MantleB.LachM.R.DelgadoS.BaeesaG.BélangerPredicting the probability of meningioma recurrence based on the quantity of peritumoral brain edema on computerized tomography scanningNeurosurgery9131999375383
- T.TamiyaY.OnoK.MatsumotoT.OhmotoPeritumoral brain edema in intracranial meningiomas: effects of radiological and histological factorsNeurosurgery49200110461052
- S.NakasuY.NakasuM.NakajimaM.MatsudaJ.HandaPreoperative identification of meningiomas that are highly likely to recurJ Neurosurg901999455462
- F.IldanM.TunaA.I.GoçerCorrelation of the relationships of brain-tumor interfaces, magnetic resonance imaging, and angiographic findings to predict cleavage of meningiomasJ Neurosurg911999384390
- FarukIldanTahsinErmanA.iskender GoçerMetinTunaHuseyinBagdatogluRefikBurgutPredicting the Probability of meningioma recurrence in the preoperative and early postoperative period: a multivariate analysis in the midterm follow-upSkull Base1732007157171
- R.E.MantleB.LachM.R.DelgadoS.BaeesaG.BelangerPredicting the probability of meningioma recurrence based on the quantity of peritumoral brain edema on computerized tomography scanningJ Neurosurg9131999375383