Abstract
Introduction
Endometrial cancer is the commonest gynecological cancer mostly affecting women in the postmenopausal age group. There is a debate regarding the need of pelvic lymphadenectomy in managing stage 1A diagnosed preoperatively, we try to evaluate this need.
Objective
To evaluate the role of pelvic lymphadenectomy in stage 1A endometrial carcinoma diagnosed preoperatively by pelvic ultrasonography and CT scan as microscopic invasion of pelvic lymph nodes will not be seen by this imaging technique.
Methods
60 Cases of endometrial carcinoma diagnosed by fractional curettage and proved to be stage 1A preoperatively by clinical examination, vaginal US and CT scan (negative myometrial invasion, ascites, LN spread and local spread) underwent total abdominal hysterectomy with salpingo-oopherectomy, peritoneal wash for cytology, omentectomy and pelvic lymphadenectomy (external iliac and obturator groups) after written informed consent. Histopathology of the uterus, tubes, ovaries, omentum and cytology of peritoneal wash were done for surgical staging, in addition histopathology of pelvic LN was done.
Results
Histopathology of the cases revealed the following: 52 cases were endometrioid adenocarcinoma distributed as follows: 10 patients were grade 1, 35 patients were grade 2 and 7 patients were grade 3. Eight cases were serous papillary adenocarcinoma, 3 of them were grade 1 and 5 cases were grade 2. As regards myometrial invasion 9 cases of endometrioid carcinoma show invasion, 1 of grade 1, 3 of grade 2 and 5 of grade 3 in comparison to 4 cases of papillary serous adenocarcinoma 1 of grade 1 and 3 of grade 2, so 13 cases have been proved by histopathology to have myometrial invasion.
Conclusion
There is no need for lymphadenectomy in stage 1A diagnosed preoperatively using CT scan and vaginal US, preventing high risk surgical intervention in this early stage.
1 Introduction
Endometrial cancer is the commonest gynecological cancer mostly affecting women in the postmenopausal age group. Rates vary around the world but are highest in white women in Western populations.Citation1
While in Africa, south Asia and developing countries, it ranks the second after cervix cancer.Citation2 Risk factors for corpus cancer can be classified as endogenous, with prolonged high estrogen levels, and exogenous.
Endogenous risk factors include obesity, early menarche, late menopause, low parity, polycystic ovary syndrome, estrogen secreting tumors, and family history, particularly the Lynch type II syndrome. The data are inconclusive for diabetes mellitus and immune deficiency.Citation3 Exogenous risk factors include noncyclical estrogen replacement therapy, tamoxifen therapy, sequential oral contraception, diet, and previous radiation therapy.Citation4 The median age for diagnosis of endometrial carcinoma is about 60 years. Abnormal bleeding is the most common presenting symptom, but a few patients are asymptomatic.Citation5 Because there is no adequate screening test for endometrial cancer, it is common practice to sample the endometrium of postmenopausal women who experience abnormal bleeding.Citation6 Endometrial carcinoma is divided into numerous histologic categories based on cell type. The most common cell type, endometrioid, accounts for 75% to 80% of cases.Citation7 Other types include papillary serous adenocarcinoma and the less common clear cell types.Citation8 The International Federation of Obstetricians and Gynecologists 1988 staging system for tumors of the uterine corpus is as follows:
IA G123 Invasion confined to the endometrium
IB G123 Invasion confined to the inner half of the myometrium
IC G123 Invasion to outer half of the myometrium
IIA Endocervical glandular involvement only
IIB Cervical stromal invasion
IIIA Tumor invades uterine serosa, adnexa, and/or positive peritoneal cytology
IIIB Vaginal metastasis
IIIC Metastasis to pelvic or paraaortic lymph nodes
IVA Tumor invasion of the bladder and/or bowel mucosa
IVB Distant metastasis including intra-abdominal or inguinal node metastases.Citation9
Preoperative staging includes vaginal US and CT scan to detect local spread and pelvic and paraaortic LN spread. There is a debate regarding the need of pelvic lymphadenectomy in managing stage 1A diagnosed preoperatively, we try to evaluate this need.
2 Aim
The aim was to evaluate the role of pelvic lymphadenectomy in stage 1A endometrial carcinoma diagnosed preoperatively by pelvic ultrasonography and CT scan.
3 Patients and methods
Following approval by our institutional ethics committee, 60 cases of endometrial carcinoma diagnosed by fractional curettage and proved to be stage 1A preoperatively by clinical examination, vaginal US and CT scan (negative myometrial invasion, ascites, LN spread and local spread) underwent total abdominal hysterectomy with salpingo-oopherectomy, peritoneal wash for cytology, omentectomy and pelvic lymphadenectomy (external iliac and obturator groups) after written informed consent. Histopathology of the uterus, tubes, ovaries, omentum and cytology of peritoneal wash were done for surgical staging, in addition to histopathology of pelvic LN to show percentage of microscopic LN spread or macroscopic spread not detected by CT.
4 Results
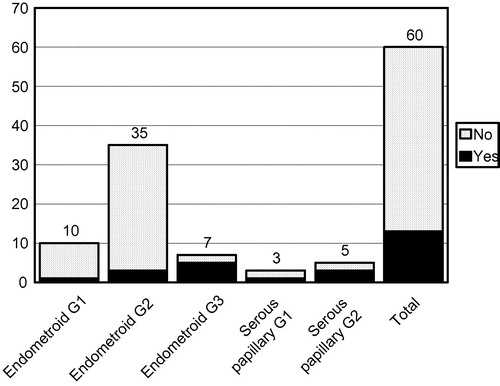
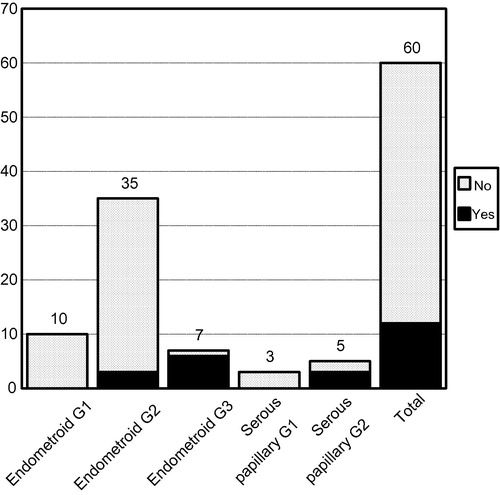
Histopathology of the cases revealed the following: 52 cases were endometrioid adenocarcinoma distributed as follows: 10 were grade 1, 35 grade 2 and 7 were grade 3. 8 cases were serous papillary adenocarcinoma, 3 of them were grade 1 and 5 were grade 2. As regards myometrial invasion 9 cases of endometrioid carcinoma show invasion, 1 of grade 1, 3 of grade 2 and 5 of grade 3 in comparison to 4 cases of papillary serous adenocarcinoma 1 of grade 1 and 3 of grade 2, so 13 cases have been proved by histopathology to have myometrial invasion. As regards histopathology of pelvic LN 12 cases out of 60 have been proved to have metastatic lesion 3 of them were serous papillary adenocarcinoma grade 2 and 9 were endometrioid, 3 grade 2 and 6 grade 3. As regards cytology of peritoneal fluid all cases were negative for atypical cells. Also all cases showed neither spread to tubes and ovaries nor omental affection.
4.1 Statistical analysis
The Data were collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 17) software.
Arithmetic mean, standard deviation, number and percent, ANOV-test were used to compare between different types of endometrial cancer group regarding age. For categorized parameters, chai square test was used to compare between the positive and negative in the same diagnosis, while Z test was used to compare between the positive cases in each type of endometrial cancer. The level of significance was 0.05.
There is no significant difference between different histological grades of pathological types of endometrial carcinoma and age (p = 0.107) ().
Table 1 Relation between pathological types of endometrial carcinoma and age, myometrial invasion and metastatic affection of pelvic lymph nodes.
There was a significant difference as regards myometrial invasion between cases with myometrial invasion and cases without (p = 0.0074) (), also there was a significant difference as regards lymph node metastasis between cases that show positive lymph node affection and cases without (p = 0.0012), while there was no significant difference between the different histological grades of the different pathological types in cases with myometrial invasion (p = 0.215) (), also no significant difference between the different histological grades of the different pathological types in cases with lymph nodes metastasis was found (p = 0.265). ( and ).
Table 2 Relation between pathological types of endometrial carcinoma and age.
Table 3 Relation between pathological types of endometrial carcinoma and myometrial invasion and metastatic affection of pelvic lymph nodes.
5 Discussion
The strongest argument for routine staging is the avoidance of pelvic radiation therapy following thorough nodal assessment and confirmation of node-negative disease and low risk status. In the absence of nodal disease, recurrence risk is low and overall survival is high, with no radiation or with the substitution of vaginal vault brachytherapy. This has encouraged many gynecologic oncologists to move toward performing routine surgical staging including pelvic and para-aortic lymphadenectomy for nearly all patients with endometrial cancer, so we select positive nodal cases for adjuvant radiotherapy.Citation10
It is suggested that lymphadenectomy improves the carcinoma-related survival and the recurrence-free survival in high-risk endometrioid adenocarcinoma patients.Citation11,Citation12 Conversely, lymphadenectomy does not appear to benefit patients with grade 1 and 2 endometrioid lesions with myometrial invasion <50% and primary tumor diameter <2 cm.Citation13
However, lymphadenectomy is a highly risky surgical intervention that needs skilled surgeon and has many serious complications as great vessel injury, so we study the need of this procedure in stage 1a which was diagnosed preoperatively using fractional curettage, vaginal US to detect myometrial invasion and CT scan to detect lymph node affection, abdominal and pelvic metastasis, but some cases may have microscopic or macroscopic LN affection which is not seen in CT scan and so we cannot assess the need of lymphadenectomy in these cases without doing sampling of LN and fresh frozen biopsy in this early stage.
Although our results showed that there was no significant lymph node affection in this early stage diagnosed preoperatively using CT scan and vaginal US, 12 cases out of 60 are missed so we need to do pelvic lymph node sampling and fresh frozen biopsy should be taken from all cases and proceed to pelvic lymphadenectomy if lymph nodes are affected, also there was no significant myometrial invasion. In addition our results showed that there was no specific histological grade in the different pathological types that is associated with lymph node metastasis or myometrial invasion.
From this study, we can conclude that pelvic lymphadenectomy is not needed in stages 1A endometrial carcinoma diagnosed preoperatively using CT scan, vaginal US and confirmed intraoperatively by lymph node sampling and fresh frozen biopsy to prevent missing cases with lymph node affection.
6 Conclusion
Pelvic lymphadenectomy is not needed in stages 1A endometrial carcinoma diagnosed preoperatively using CT scan, vaginal US and confirmed intraoperatively by lymph node sampling and fresh frozen biopsy.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 31 October 2013
References
- David M.PurdieAdèle C.GreenEpidemiology of endometrial cancerBest Pract Res Clin Obstet Gynaecol3152001341354
- Parkin D.M., Whelan S.L., Ferlay J., Teppo L., (Eds). Cancer incidence in five continents, vol. VIII. IARC Scientific Publication No. 155, International Agency for Research on Cancer, Lyon, France, 2002.
- V.BeralE.BanksG.ReevesP.ApplebyUse of HRT and the subsequent risk of cancerJ Epidemiol Biostat41999191210
- K.BakkenE.AlsakerA.E.EggenE.LundHormone replacement therapy and incidence of hormone-dependent cancers in the Norwegian Women and Cancer studyInt J Cancer1122004130134
- M.SmithJ.McCartneyOccult high-risk endometrial cancerGynecol Oncol221985154161
- L.G.KossK.ScheiberS.OberlanderDetection of endometrial carcinoma and hyperplasia in asymptomatic womenObstet Gynecol641984111
- J.FanningM.C.EvansA.J.PetersEndometrial adenocarcinoma histologic subtypes: clinical and pathologic profilesGynecol Oncol321989288291
- M.HendricksonJ.RossP.EifelUterine papillary serous carcinoma: a highly malignant form of endometrial adenocarcinomaAm J Surg Pathol6198293108
- F.I.G.O. AnnouncementsStages-1988 revisionGynecol Oncol351989125
- MarianiS.C.DowdyW.A.ClibyEfficacy of systematic lymphadenectomy and adjuvant radiotherapy in node-positive endometrial cancer patientsGynecol Oncol10122006200208
- C.V.LutmanL.J.HavrileskyJ.M.CragunPelvic lymph node count is an important prognostic variable for FIGO stage I and II endometrial carcinoma with high-risk histologyGynecol Oncol102120069297
- K.ChanM.K.CheungW.K.HuhTherapeutic role of lymph node resection in endometrioid corpus cancer: a study of 12,333 patientsCancer1078200618231830
- P.B.PaniciS.BasileF.ManeschiSystematic pelvic lymphadenectomy vs no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trialJ Natl Cancer Inst10023200817071716
