Abstract
Background
Central nervous system involvement in SLE as a part of neuropsychiatric lupus is a complex diagnostic entity due to its multiple clinical presentations.
Objective
This study aimed to assess the value of susceptibility weighted imaging (SWI) and neurophysiological assessment on 30 patients with SLE in order to determine the value in the early diagnosis and management of neurological manifestation of lupus.
Materials and methods
Thirty patients with ACR criteria for SLE are involved in this study. Antiphospholipid antibodies, SWI, and evoked response studies were used to assess neurological involvement in SLE.
Results
Eighteen patients presented with clinical neurological manifestations attributed to neurological lupus. Abnormal SWI findings were found in 16 patients. 11 SLE patients were positive for antiphospholipid. 17 patients presented with abnormal neurophysiological parameters. No correlation between individual neurophysiological disorders (NPD) and specific neuropsychiatric symptoms was observed. There was no significant correlation between the electro physiologic findings and SLE related auto antibodies.
Conclusions
SWI and neurophysiological studies may provide a useful test in the evaluation and management of early neurological lupus.
Introduction
Systemic lupus erythematosus (SLE) is a chronic, autoimmune, multiorgan disease with a broad spectrum of clinical manifestations. SLE with involvement of the central nervous system (CNS), which is often called neuropsychiatric SLE (NP-SLE), is one of the most important manifestations of SLE.Citation1 The condition may be both neurological and psychological,Citation2,Citation3 and the reported prevalence of CNS involvement varies in different studies.Citation4–Citation8 This probably reflects differences in patient selection, different criteria for NP-SLE, differences in the neuropsychological tests used and the lack of standard diagnostic instruments for CNS manifestations.
The pathogenesis of CNS dysfunction in SLE is not well understood. The observation of both diffuse and focal CNS involvement in SLE has led to the hypothesis that there are several pathogenic mechanisms in NP-SLE, such as micro vascular damage, small-vessel vasculopathy and autoantibody-mediated neuronal cell injury.Citation9–Citation12
Many biochemical and immunological studies have been undertaken in an attempt to identify specific abnormalities which might be helpful to the clinician.Citation13 In addition, the value of imaging techniques has been investigated.Citation14 However, despite considerable research, the management of neurological lupus has not been facilitated by the emergence of sufficiently reliable or practical investigative techniques. Neurophysiological techniques have been of value in the assessment of neurological symptoms occurring in other diseases such as multiple sclerosis.Citation15,Citation16
The aim of the present study was to assess the value of susceptibility weighted imaging (SWI) and neurophysiological studies on thirty randomly selected patients with SLE in order to determine whether this form of assessment might be of value in the diagnosis and management of neuropsychiatric manifestations of SLE and to correlate the radiological and electrophysiological abnormalities with SLE related auto antibodies.
Methods and patients
Thirty SLE patients were randomly selected from a population attending the Department of Rheumatology. All patients fulfilled the American Rheumatism Association, 1982 revised criteria for SLE. A detailed history and clinical examination of all patients were performed. The study also included 15 age and sex matched healthy control subjects. The entire protocol was approved by Human Ethics Committee of the Faculty of Medicine, Alexandria University, Egypt and informed consent was obtained from each human subject prior to participation.
Several investigations like autoantibody batteries [antiphospholipid antibodies (PA), anticardiolipin antibodies (aCL) and lupus anticoagulant (LA)], susceptibility weighted imaging (SWI), and electro diagnostic studies [somatosensory evoked potential (SSEP), visual evoked potential (VEP) and brain stem auditory evoked response (BAEP)] were all used to study neuropsychiatric involvement in SLE.
Patients were evaluated with routine MRI sequences; namely axial and sagittal T1-weighted images, axial and coronal T2-weighted images and coronal T2-weighted images as well as FLAIR sequences, in addition to susceptibility weighted imaging. Studies were performed on a 1.5 T MRI scanner (General Electric Medical Systems). T1-weighted images were acquired utilizing 500/20/2 TR, TE, excitations, 256 × 256 matrixes, FOV of 20 cm, 6 mm slice thickness, and 0.6 mm inter-slice gap. The T2-weighted images were acquired utilizing 4000/100/2 TR, TE, excitations, 256 × 256 matrixes, FOV of 22 cm, 5 mm slice thickness and 0.5 mm inter-slice gap. The SWI sequence parameters were TR/TE 500/30, number of excitations 2, flip angle 20°, 5 mm contiguous slices.Citation17
Statistical analysis
The data were collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 20) software.
Arithmetic mean, standard deviation, for more than two groups ANOVA test was used. The level of significance was 0.05.
Results
The study included thirty SLE patients, the patient characteristics are summarized in . The mean age of the patients was 31.3 ± 9.9 years (range: 9–49).
Table 1 Patient characteristics and neuropsychiatric manifestations in SLE.
Twenty-eight patients were females (93.3%), while two patients were males (6.7%). The duration of SLE ranged between 1 and 20 years with a mean of 6.7 ± 4.9.
Hypertension was found in 11 patients (36.7%) and nephritis was found in 6 patients (20%).
There were 18 (60%) patients who presented with definite neuropsychiatric events and twelve (40%) patients were neurologically free. Stroke was the most frequent neurological manifestation (7 patients), another 6 patients presented with headache mostly migraines, 3 patients with psychosis, 3 patients with epilepsy, two patients with mood disorder like depression, and 3 patients with polyneuropathy. Six SLE patients had more than one neuropsychiatric symptom. Seizures can occur at any time during the course of the disease. Psychosis was found in the younger age group (ranged between 12 and 29 years) while patients with polyneuropathy were about 45 years of age. Neuropsychiatric signs were significantly present in patients with hypertension (p = 0.02) and nephritis (p = 0.03).
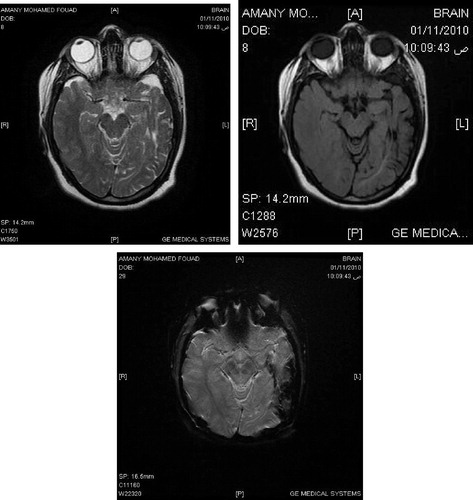
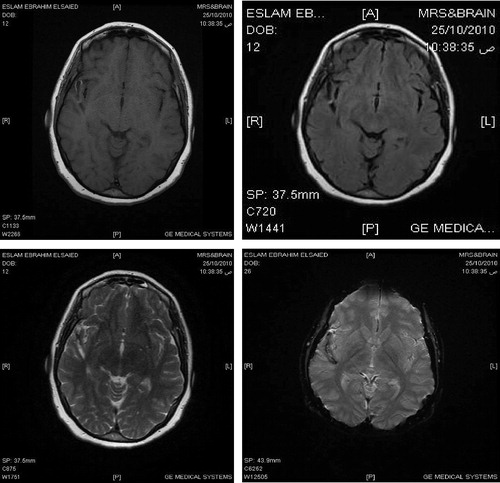
The routine MR imaging sequences were relatively insensitive for small micro hemorrhages resulting from underlying vasculopathy and only detecting the residual area of encephalomalacia; however the SWI was sensitive for detection of areas of old micro hemorrhages and abnormal vasculopathy resulting in the formation of hemosiderin that causes local magnetic field in homogeneity.
Abnormal SWI findings were found in 16 patients. Patients with abnormal SWI were divided into 14 patients with focal parenchyma lesions, 2 patients with brain atrophy. Patients with focal parenchyma lesions were subdivided into 9 patients with multiple lesions <1 cm located in the sub cortical white matter (SSCL) and 5 cases with lesion >1 cm (infarcts). One of these patients had mixed small sub cortical lesions and infarct. There was no statistical significant difference between the age of the patients and the abnormal SWI findings (p = 0.36). Moreover, the duration of the disease did not differ significantly among those with normal or abnormal SWI (p = 0.51).
The presence of abnormal radiological findings and the distribution of the different SWI categories were significantly more frequent in the hypertensive patients (p = 0.004, p = 0.00, respectively). There were twelve (40%) patients without neuropsychiatric manifestations but the SWI was abnormal in 5 of them, 3 of them had small sub cortical lesions and 2 had cortical cerebral atrophy ( and ).
Assessment of SLE related auto antibodies revealed, eleven SLE patients (37%) were PA positive. Of the patients with PA positive, 5 (17%) had positive aCL and 3 (10%) had positive LA and another 3 (10%) had both aCL and LA. The mean age of patients with or without positive PA was not significantly different. The frequency of positive auto antibodies in patients with vascular insults was higher than those without but with no statistical significant difference. The distribution of immunoserological findings was different among the different SWI categories ().
Table 2 Radiological changes associated with phospholipid antibodies.
As shown in , the mean evoked potential study parameters were significantly altered in SLE patients compared to controls. Evoked potential abnormalities were detected in seventeen patients (57%). In SLE patients with neuropsychiatric symptoms, 12 patients out of 18 had neurophysiological abnormalities as shown in the prolonged latencies and diminished amplitudes in SSEP and VEP. Also, altered BAEP as manifested by prolonged wave L1 absolute latency and prolonged interpeak interval 111-V.
Table 3 Comparison between SLE patients and controls regarding evoked potential parameters.
Abnormalities in the peripheral nerve conduction were found in two patients. In patients with no neuropsychiatric symptoms, five (42%) had abnormalities in SSEP, VEP and BAEP.
Abnormal BAEP was significantly more frequent in the older age group as shown in prolonged wave L2 latency (p = 0.4) and prolonged interpeak intervals 1-V and 111-V (p = 0.00, p = 0.01, respectively). Moreover, BAEP wave L4 latency was significantly more prolonged in patients with longer disease duration (p = 0.015).
There was no statistical significant correlation between individual neurophysiological disorders and specific neuropsychiatric symptoms. Moreover, there was no significant correlation between abnormal electrophysiologic findings and SLE related auto antibodies.
Discussion
In the present study, there was no statistical significant correlation between abnormal radiological findings in SWI and the age of the patients and the duration of the disease. Csepany et al.Citation18 reported that no correlation was found between the MRI findings and age of the patient at the time of the diagnosis and the duration of SLE which means that involvement of the CNS may occur any time during the course of SLE. In contrast, GonzalesCitation19 reported that CNS lesions in patients with SLE were associated with patient age and with disease duration, but the patients in their study were younger, the duration of SLE was shorter. With the progress of the disease, the effect of risk factors as age and hypertension might have more significant influence on the MRI findings.
SWI is a three dimensional velocity-compensated gradient echo sequence that combines both magnitude information (used in conventional MR images, including T2∗ GE with phase information to accentuate the visibility of susceptible foci such small veins and hemorrhage. Micro-hemorrhages contain hemosiderin, which is paramagnetic relative to normal tissue and leads to large variations in local magnetic fields and a local reduction in T2∗. The signal intensity loss is proportional to the amount of hemosiderin present. SWI, with its unique sensitivity to blood products and hemorrhage, is well-suited to detect imaging changes consistent with cerebral angiopathy.Citation14–Citation17
In the current study, abnormal radiological findings detected by SWI in SLE are more common in patients with neurological deficits than those without and these abnormalities are significantly more frequent in the hypertensive patients. Moreover, the distribution of the different SWI findings especially infarcts differed significantly between hypertensive and normotensive patients. The American College of Rheumatology for NP-SLE provided case definitions for 19 neuropsychiatric syndromes seen in SLE.Citation1 Some authors consider that stroke is one of the most important complications of SLE.Citation20,Citation21
Various auto antibodies have been implicated in pathogenesis of NP-SLE including aCL and LA. In this study, 37% of patients with SLE were PA positive. Abnormal aCL and LA were more frequent in patients of cerebrovascular insult. However, there was no statistically significant difference in the percentage of the patients with or without positive PA subtypes and neuropsychiatric involvement.
In the present study, small sub cortical lesions <1 cm detected in SWI were more frequent (10 out of 30) than larger lesions (5 out of 30), and the presence of these lesions did not significantly correlate with the immunological status of the patients. In this context, several studies found that the frequency of increased serum level of aCL was higher in patients with active NP-SLE compared to those without CNS affection.Citation22,Citation23
Case studies of patients with antiphospholipid syndrome and lupus have demonstrated microscopic infarcts of the cortical gray matter and fresh and recanalized thrombi with fibro muscular webs of the leptomeningeal arteries.Citation24 This type of CNS involvement might remain unrecognized by MRI because of limited resolution of the examination. The small sub cortical lesions might be related to vessel wall changes caused by either SLE itself or hypertension whereas the larger infarcts associated with PA of thrombotic origin result in unique vascuolopathy.Citation25,Citation26 Many studies suggest that this unique vasculopathy seen in SLE is highly associated with PA antibodies.Citation27,Citation28
In the present study, 19 patients (63%) had within normal serum PA although the majority of them had abnormal evoked potential parameters implying that these SLE related auto antibodies may not be involved in the pathogenesis of abnormal electrophysiological findings in the subclinical NP-SLE. Mowaffak et al.Citation29 studied 20 patients with SLE and they reported that almost all patients with SLE (except two) had within normal serum aCL level although all except one had abnormal motor evoked potential parameters. Also, they concluded that the normal levels of the assessed antibodies in the study pointed out to their negligible pathogenic contribution to the motor evoked potential changes in neurologically asymptomatic patients.
Similarly, Ainiala et al.Citation30 stated that the motor evoked potential abnormalities are most probably related to brain ischemia due to small vessel vasculopathy not mediated by SLE related auto antibodies.
From the current study, it can be concluded that electrophysiological studies can be a useful tool to detect subtle CNS involvement in neurologically asymptomatic patients. However, to confirm its efficiency and reliability as a screening tool, it should be compared with one of the MRI techniques that detects CNS involvement at the microscopic level. Detecting electrophysiological abnormalities in neurologically asymptomatic SLE patients should improve treatment decisions and management.
Therefore, we suggest performing the SWI and electrophysiological studies in SLE patients, even in the asymptomatic ones, early in the course of the disease in order to detect the CNS involvement.
In our study, the presence of neurophysiological and radiological abnormalities in neurologically asymptomatic patients may have a value in early detection of the neuropsychiatric manifestations. If these observations are extended and confirmed, SWI and neurophysiological studies may provide a useful test to the clinician in the evaluation and management of neurological lupus.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 13 January 2014
References
- American College Rheumatology (ACR) Ad Hoc committee on Neuropsychiatric Lupus NomenclatureThe American college of rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromesArthritis Rheum421999599608
- D.EstesC.L.ChristianThe natural history of systemic lupus erythematosus by prospective analysisMedicine5019718595
- T.AbelD.D.GladmanM.B.UrowitzNeuropsychiatric lupusJ Rheumatol71980325333
- W.J.McCuneJ.GolbusNeuropsychiatric lupusRheum Dis Clin North Am141988149167
- R.OmdalB.SelsethN.E.KløwG.HusbyS.I.MellgrenClinical neurological, electrophysiological, and cerebral CT scan findings in systemic lupus erythematosusScand J Rheumatol181989283289
- N.FutrellL.R.SchultzC.MillikanCentral nervous system disease in patients with systemic lupus erythematosusNeurology42199216491657
- M.R.TolaE.GranieriL.CaniattiSystemic lupus erythematosus presenting with neurological disordersJ Neurol23919926164
- E.M.WeckingPsychiatric symptoms in systemic lupus erythematosus: an updatePsychosom Med551993219228
- O.D.DevinskyC.K.PetitoD.R.AlonsoClinical and neuropathological findings in systemic lupus erythematosus: the role of vasculitis, heart emboli, and thrombotic thrombocytopenic purpuraAnn Neurol231988380384
- J.G.HanlyN.M.WalshV.SangalangBrain pathology in systemic lupus erythematosusJ Rheumatol191992732741
- J.A.DenburgS.A.BehmannLymphocyte and neuronal antigens in neuropsychiatric lupusAnn Rheum Dis531994304308
- J.A.DenburgR.M.CarbotteS.D.DenburgNeuronal antibodies and cognitive function in systemic lupus erythematosusNeurology371987464467
- Lr.BeryDiagnosis and management of patients with neuropsychiatric systemic lupus erythematosus (NSSLE). Best practice and researchClin Rheum16202002229244
- V.SehgalZ.Del PropostoE.M.HaackeClinical applications of neuroimaging with susceptibility–weighted imagingJ Magn Reson Imaging222005439450
- Ab.MonegeyM.HutchinsonB.BresnihanClinical neurophysiology in the assessment of neurological symptoms in systemic lupus erythematosusRheumatol Int7219874952
- L.T.L.CostallatE.M.QuagliatoV.A.ZanardiEvoked potentials in the assessment of neuropsychiatric manifestations in systemic lupus erythematosusClin Rheumatol1621997217221
- J.R.ReichenbachL.Jonetz-MentzelC.FitzekE.M.HaackeD.K.KidoB.C.P.LeeHigh-resolution blood oxygen-level dependant MR venography (HRBV): a new techniqueNeuroradiology432001364369
- T.CsepanyD.BereczkiJ.KollarJ.SikulaMRI findings in central nervous systemic systemic lupus erythematosus are associated with immunoserological parameters and hypertensionJ Neurol250200313481354
- M.R.GonzalezF.J.BlancoA.RamosE.CirueloMagnetic resonance imaging of the brain in systemic lupus erythematosusBr J Rheumatol34199510551060
- N.FutrellC.MillikanFrequency, etiology, and prevention of stroke in patients with systemic lupus erythematosusStroke201989583591
- W.L.SibbittR.R.SibbittW.M.BrooksNeuroimaging in neuropsychiatric systemic lupus erythematosusArthritis Rheum42199920262038
- M.RovarisB.VitiG.CiboddoS.GereviniR.CapraG.GomiBrain involvement in systemic immune mediated diseases; magnetic resonance and magnetization transfer imaging studyJ Neurol Neurosur Psychiatry682000170177
- S.C.SteenG.P.BosmaG.M.Steup-BeckmanS.Le CessieT.W.HuizingaAssociation between microscopic brain damage as indicated by magnetization transfer imaging and anticardiolipin antibodies in neuropsychiatric lupusArthritis Res Ther822006R38
- M.D.HughsonG.A.Mc CartyC.M.ShlerR.A.BrumbackThrombotic cerebral arteriopathy in patients with antiphospholipid syndromeMod Pathol61993644653
- M.GreavesAntiphospholipid antibodies and thrombosisLancet353199913481353
- D.FerroS.BasiliS.RoccaforteDeterminants of enhanced thromboxane biosynthesis in patients with systemic lupus erythematosusArthritis Rheum42199926892697
- S.D.AlarconM.CardielE.ReyesAntiphospholipid arterial vasculopathyJ Rheumatol161989762767
- J.T.LieVasculopathy in the antiphospholipid syndrome: thrombosis or vasculitis or both?J Rheumatol161989713715
- M.S.MowaffakA.S.NohaA.Z.AshrafW.A.MonaMotor evoked potentials and autoantibodies in neurologically asymptomatic systemic lupus erythematosus patientsEgypt Rhematol Rehabil3732010403416
- H.AinialaA.hietaharjuP.DastidarJ.loukkolaJ.lehtimakiIncreased serum matrix metalloproteinase 9 levels in systemic lupus erythematosus patients with neuropsychiatric manifestations and brain magnetic resonance imaging abnormalitiesArthritis Rheum5032004858865
