Abstract
Aim of the work
The purpose of this study is to describe the MRI features of some uncommon causes of knee pain.
Materials and methods
This is a retrospective study. We reviewed our database including the last 1000 knee MRI examinations done within the period from January 2012 till June 2013. This revision revealed 12 cases with reported variable uncommon diagnoses explaining knee pain. Unenhanced MRI of the knee was performed and included sagittal T1, T2, T2∗ and proton density fat suppression (PDFS), axial T2 and coronal PDFS. Some cases had complementary CT assessment.
Results
The selected 12 cases included the following; three cases of supero-lateral Hoffa’s pad of fat edema expressing edema signal at the superolateral aspect of the Hoffa’s pad of fat. Three cases with fabella syndrome with chondral and subchondral edema signal at the posterior aspect of the lateral femoral condyle. Two cases with symptomatic bipartite patella showing marrow edema around the patellar synostosis. One case with proximal tibio-fibular synostosis evident on MRI as bony fusion. Two cases with quadriceps (suprapatellar) fat-pad impingement syndrome manifested as edema signal within the supra-patellar fat-pad and lastly one case with lipoma arborescence seen as frond like projections with fat signal protruding into the supra-patellar bursa.
Conclusion
MRI is a useful tool in evaluation of some uncommon causes of painful knee.
1 Introduction
Many patients are referred for MRI because they have painful knees. It is not difficult to diagnose most of the common causes of knee pain by MRI including internal derangement, arthritis, synovitis as well as osseous, chondral and muscular lesions. However some uncommon causes of knee pain may be overlooked inspite of the patient’s significant complaint. This usually misleads the treating physician who may proceed for arthroscopy to clarify the hidden cause of the knee pain in these patients.
The purpose of this retrospective study is to describe the MRI features of some uncommon causes of knee pain.
2 Materials and methods
This is a retrospective study. With approval of the institutional review board and committee of ethics in our university, we reviewed the database in a private radiology center including the last 1000 knee MRI examinations done within the period from January 2012 till June 2013. This revision revealed 12 cases with reported variable uncommon diagnoses explaining knee pain. These 12 cases will be the core of this work. The privacy of these records was respected according to the instructions of the ethics committee in our university.
Inclusion criteria were painful knee with no age or sex predilection. Exclusion criteria were: any history of trauma, surgery or reported MRI findings of internal derangements, synovitis, arthritis, osteoarthrosis as well as bone or synovial tumors. Also cases with insufficient clinical data were excluded.
Unenhanced MRI of the knee was performed using multiple machines; 1.5-T closed MR unit (Avanto, Siemens) and 0.35-T open MR unit (Magnetom C, Siemens) with a knee dedicated coil. The MRI examinations included sagittal T1, T2, T2∗ and proton density fat suppression (PDFS), axial T2 and coronal PDFS or T2 fat suppressed sequences. Some cases had complementary CT assessment.
3 Results
The selected 12 cases included three cases of supero-lateral Hoffa‘s fat pad edema, three cases with fabella syndrome, two cases with symptomatic bipartite patella, one case with proximal tibio-fibular synostosis, two cases with quadriceps (suprapatellar) fat pad impingement syndrome and lastly one case with lipoma arborescence.
All these 12 patients had accessible medical records with no clinical evidence of trauma or surgery. They included 7 males and 5 females with their ages ranging from 16 to 45 years. Some patients complained of diffuse knee pain while some complained of localized knee pain i.e. anterior, posterior, medial or lateral knee pains. Some patients also complained of limitation of the knee flexion or extension, knee swelling or pseudo-locking. provides a summary of the demographic and clinical data as well as MRI findings.
Table 1 Summary of the demographic, clinical and MRI features of the cases included in this study.
3.1 Fabella syndrome
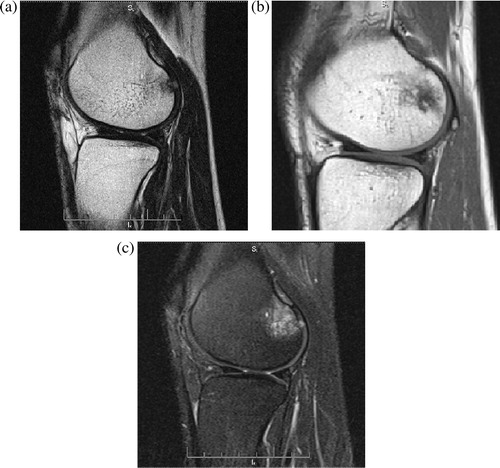
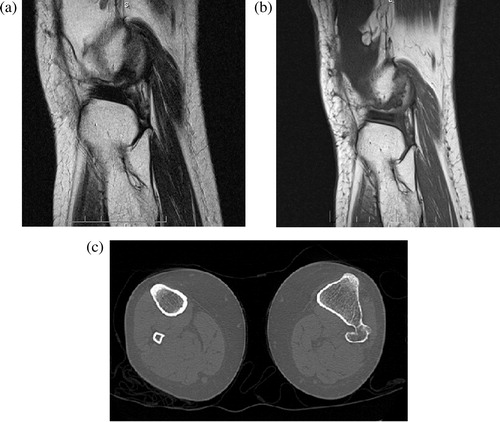
Three patients (two females 18 and 30 years and one male 25 years) had fabella syndrome. They complained of pain at the lateral posterior aspect of the knee with clinically elicited tenderness at the posterior aspect of the lateral femoral condyles with suggested diagnosis of chondral ulcers. MR edema signals were noted at hyaline cartilage and sub-chondral marrow at the posterior aspect of lateral femoral condyles, being more evident on PDFS without definite chondral ulcers, reflecting fabella syndrome. Some of these patients revealed fabellar enlargement and edematous changes on MRI. ().
3.2 Symptomatic bipartite patella
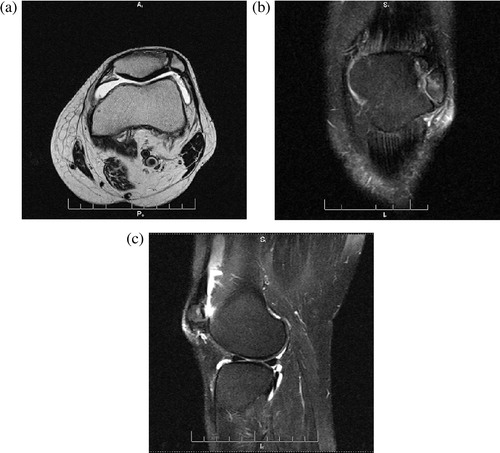
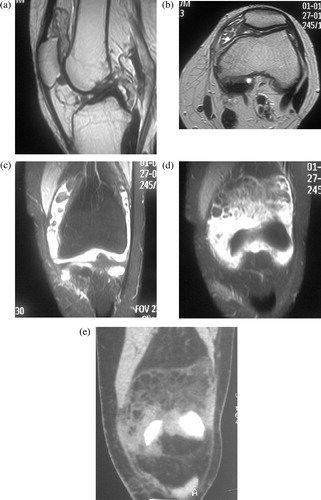
Two male patients aged 17 and 21 years had symptomatic bipartite patella. They were athletes and complained of chronic pain at the anterior aspect of the knee especially during knee flexion with clinically elicited tenderness at the patella. No frank history of trauma was reported. MRI revealed bipartite patella with well corticated margins of the accessory patella with marrow edema around the junction of the accessory and main patellae. Complementary CT confirmed the absence of patellar fractures and bipartite configuration. ().
3.3 Quadriceps fat pad impingement syndrome
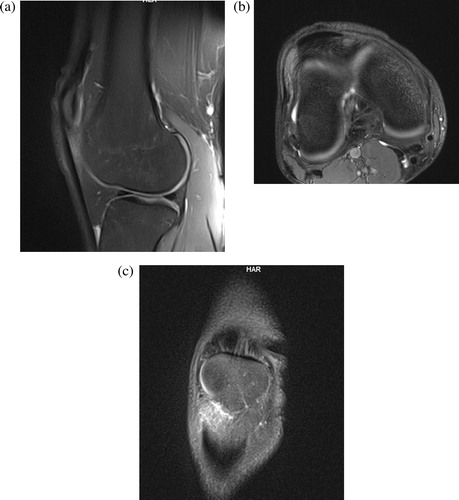
A male patient aged 25 years and a female patient aged 27 years had quadriceps pad of fat impingement syndrome. They complained of chronic pain at the anterior aspect of the knee especially during walking with clinically elicited tenderness just above the patella. MRI revealed low T1 and intermediate T2 signal at the small supra-patellar pad of fat with high signal on the PDFS sequences while the infra-patellar pad of fat and the subcutaneous fat showed drop of signal. The overlying quadriceps tendons as well as the patella were unremarkable. ().
3.4 Proximal tibiofibular synostosis
A male patient aged 22 years complained of chronic pain at the lateral aspect of the knee and upper leg. MRI revealed evidence of bony over growth and communication was noted to partially involve the proximal tibiofibular articulation as well as the upper shafts of the fibula and tibia with deformed shape of the fibular head, reflecting synostosis which was clearly evident on complementary CT. ().
3.5 Lipoma arborescence
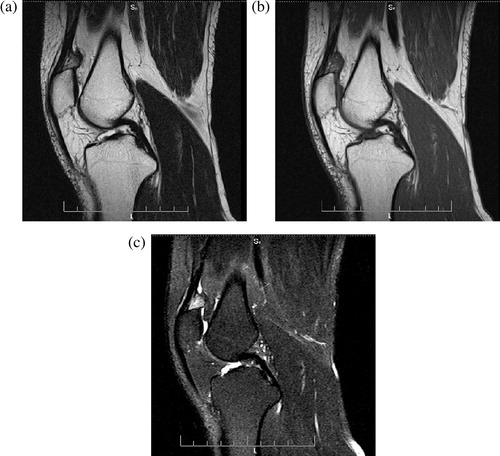
A 42 year male patient was complaining of left knee supra-patellar swelling and anterior mild pain that was lasting for years ago. The clinical examination raised the possibility of synovial mass. His knee MRI demonstrated a villous like synovial lesions protruding into the supra-patellar bursa and effusion. These lesions express fat signal intensity (T1 and T2 high signal that dropped on PDFS). CT proved the fatty nature of the lesion. ().
3.6 Superolateral Hoffa’s fat pad edema
Two female patients aged 42 and 36 years as well as a male patient aged 38 years had superolateral Hoffa’s fat pad edema. They complained of chronic pain at the anterior aspect of the knee with clinically elicited tenderness just lateral to the patella. MRI revealed low T1 and high T2 signal at the superior lateral portion of the infra-patellar fat pad with high signal on the PDFS sequences while the rest of the infra-patellar pad of fat and the supra-patellar pad of fat showed drop of signal. Two of these cases had patella alta (patellar tendon/patella = 1.4) while the third had shallow femoral trochlear groove with the overlying lateral patellar retinacula which showed subtle T2 high signal ().
4 Discussion
The fabella, which means little bean is a sesamoid bone located in the lateral head of the gastrocnemius muscle. It is present in 10 to 30 percent of population, and is seen bilaterally in more than 50% of the adult population.Citation1 The salient features of the fabellar syndrome include intermittent pain in the posterolateral aspect of the knee, accentuated by knee extension and localized tendemess caused by compression against the femoral condyle. The syndrome is most common in early adolescence (it may be seen in all ages) and most likely is the result of repetitive friction of the fabella over the posterolateral femoral condyle. Proximity of the fabella to the femoral condyle has been implicated in causing synovial irritation and roughening of the articular surfaces.Citation2,Citation3 Radiographically, fabella may be big and demonstrates irregular shape and abnormal density. This finding may be associated with chondral or subchondral change in the posterior portion of lateral femoral condyle. Irregular appearance of fabella may be confused with foreign body but MRI helps to locate it within the muscle. Abnormality in the posterior portion of femoral condyle may look like osteochondral defect or osteochondritis dissecans, MRI combined with CT can clearly exclude these lesions.Citation4
Bipartite patella has an incidence of 3% and is usually asymptomatic. Painful bipartite patella is rarely seen in adolescents or young athletic adults under 20 years of age. Painful bipartite patella in a non-athletic adult is rather very rare. A posttraumatic etiology is assumed by most authors as a cause of painful bipartite patella. Repetitive micro-traumata disrupting the integrity of the fibro-cartilaginous zone between the patella and the accessory bipartite fragment can explain the pathogenesis of painful bipartite patella. These patients show bone marrow edema on MRI within the bipartite fragment with or without abnormal signal across the synchondrosis or pseudarthrosis.Citation5,Citation6 Similar findings are noted in our cases.
Three normal fat pads are located about the anterior knee: the quadriceps (anterior suprapatellar), the prefemoral (posterior suprapatellar or supratrochlear), and Hoffa (infrapatellar) fat pads. The quadriceps fat pad is the normal fat pad between the suprapatellar recess posteriorly and quadriceps tendon anteriorly. Pain in the front of knee has many causes. Numerous traumatic and non-traumatic processes may be encountered including fat pad impingement syndrome. The term “quadriceps fat pad impingement” has been used to describe an inflammatory process within the anterior supra-patellar fat, manifested on MRI as high T2 signal, low T1 signal and with enlargement causing some mass effect on the quadriceps tendon. The cause is usually due to either developmental cause related to the anatomy of the extensor mechanism, or may be related to abnormal mechanics. In this syndrome the posterior border of the fat pad is convex with mass effect upon supra-patellar recess.Citation7,Citation8 Similar findings were seen in our cases but without evident enlargement and mass effect on the quadriceps tendon. This may be due to earlier stages of the disease in our cases.
Synostosis of the proximal tibiofibular joint is rare. It may occur in children, adolescents, or adults. It may be caused by the coalescence of osteochondromata in patients with multiple hereditary exostoses, or may be associated with other syndromes.Citation9 Clinically, it may present with peroneal paralysis due to peroneal nerve entrapment but it may present with lateral knee and ankle pain.Citation10
O’Dwyer kJ et al.Citation11 described three types of proximal tibio-fibular synostosis; type I that shows a straight fibula with proximal synostosis, type II has mild bowing of the fibula with widening of the interosseous distance in the proximal half only. Type III shows marked bowing of the fibula with widening of the interosseous distance in the distal half with synostosis occurring at a distal level compared to type II. Our case is matching with type I with proximal synostosis, deformed fibular head and rather straight fibula. MRI easily detects the fused bony portions with marrow signal at the fusion site and excluded edema that may be due to marrow contusion or degenerative changes.
Lipoma arborescens is a “lipoma-like” lesion and not a tumor in which the sub-synovial connective tissue is infiltrated by mature adipocytes, often associated with scattered inflammatory cells. Lipoma arborescens is frequently a secondary reactive process associated with degenerative joint disease, chronic rheumatoid arthritis, or prior trauma. However, primary cases without underlying chronic intra-articular pathologic conditions have been reported. Patients range in age from 9 to 66 years, with males affected much more commonly than females. They are usually present as painless swelling with intermittent pains due to effusions.Citation12
MR imaging demonstrates large villous, frond like masses with an associated joint effusion. The signal intensity of the frond like projections exhibits the signal characteristics of fat, regardless of pulse sequence. Enhancement following intravenous administration of contrast material may be seen in the overlying inflamed synovium. Lesions have been mistaken for liposarcoma, and the key to diagnosis is recognition of the diffuse synovial (joint or bursal) origin, as well as the multilobulated frond like contour. CT also shows a frond like mass of fat attenuation, although the villous nature may be more difficult to recognize at CT, compared with MR imaging.Citation13,Citation14
HoffaCitation15 described chronic impingement of the fat pad between the femur and tibia in 1904. The impingement manifests on MRI as fat pad enlargement and increased T2 signal. Another form of impingement, which is radiologically more subtle, occurs at the supero-lateral portion of the fat pad between the patellar tendon and lateral femoral condyle and results in high T2 signal intensity on MRI due to edema.Citation16
Superolateral Hoffa’s fat pad edema is a frequent finding in patellar maltracking or impingement disorders.Citation17
Chung et al.Citation18 described the typical MR-findings of high signal on T2- and low SI on T1- weighted images in the lateral portion of the infra-patellar fat pad due to impingement of the lateral portion of Hoffa’s fat pad between the lateral femoral condyle and the lateral patellar border with consequent contusion and reactive inflammatory changes within the fat. This may or may not be associated with retro-patellar cartilage damage, bone marrow edema and patellar tendon abnormalities.
Subhawong et al.Citation17 reported that they found that female sex and several markers of patellar instability appear to be associated with superolateral Hoffa’s fat pad edema in patients with knee pain, these markers included increase in the patellar tendon–patellar length ratio and trends toward increased lateral patellar tilt and a shallower trochlear sulcus. They postulated that these factors positively influence excessive friction or pressure of the lateral patellar facet over the lateral femoral condyle, resulting in edema in the intervening supero-lateral portion of Hoffa’s fat pad.Citation17 Some authors described similar MRI features and gave the name of patellar tendon-lateral femoral condyle friction syndrome which is also related to the clinical entity of fat pad impingement.Citation19 Our 3 cases exhibit high T2 signal in the super-lateral portions of the infra-patellar pad of fat, two of them had patella alta while the third had shallow femoral trochlear groove the overlying lateral patellar retinacula which showed subtle T2 high signal.
We have described MRI signs of some of the uncommon causes of knee pain which appear simple if the radiologist is aware of their significance. These signs would not be missed if fat suppression sequences are used routinely in knee examination and meticulously analyzed.
5 Conclusion
MRI is a useful tool in the evaluation of some uncommon causes of painful knee that can be easily over-looked if the radiologist is unaware of these entities.
Conflict of interest
None.
Grant support
None.
Notes
This work was not presented anywhere.
Available online 20 February 2014
References
- T.T.H.KawashimaS.YoshitomiAnatomical study of the fabella complex and its clinical implicationsSurg Radiol Anat2982007611616
- D.S.WeinerI.MacnabThe, “fabella syndrome”: an updateJ Pediatr Orthop241982405408
- A.J.S.RobertsonR.PaesThe fabella: a forgotten source of knee pain?Knee1132004243245
- J.T.ZippleR.L.HammerP.V.LoubertTreatment of fabella syndrome with manual therapy: a case reportJ Orthop Sports Phys Ther33120033339
- F.M.VanhoenackerA.BernaertsS.Van de PerreA.M.De SchepperMRI of painful bipartite patellaJBR-BTR8542002219
- E.C.Z.A.KavanaghI.OmarS.FordM.SchweitzerS.EustaceMRI findings in bipartite patellaSkeletal Radiol3632007209214
- A.BasO.TutarI.YanikC.SamanciQuadriceps fat-pad impingement syndrome: MRI findingsBMJ Case Rep 20122012
- C.J.J.RothD.JamadarE.CaoiliY.MoragJ.HousnerQuadriceps fat pad signal intensity and enlargement on MRI: prevalence and associated findingsAJR Am J Roentgenol1826200413831387
- N.K.SferopoulosSynostosis of the proximal tibiofibular jointCase Rep Med 20102010
- K.J.O’DwyerProximal tibio-fibular synostosis. A rare congenital anomalyActa Orthopaedica Belgica5721991204208
- K.J.ODProximal tibio-fibular synostosis: a rare congenital anomalyActa Orthop Belg571991204208
- S.J.W.I.ArmstrongLipoma arborescens of the kneeBr J Radiol621989178180
- M.D.MurpheyJ.F.CarrollD.J.FlemmingT.L.PopeF.H.GannonM.J.KransdorfFrom the Archives of the AFIP: benign Musculoskeletal Lipomatous Lesions1Radiographics 2004245200414331466
- J.C.B.J.VilanovaM.VillalonJ.AldomaE.DelgadoZapater I MR imaging of lipoma arborescens and the associated lesionsSkeletal Radiol322003504509
- A.HoffaThe influence of adipose tissue with regard to pathology of the knee jointJAMA431904795796
- D.SaddikE.G.McNallyM.RichardsonMRI of Hoffa’s fat padSkeletal Radiol3382004433444
- T.K.SubhawongJ.EngJ.A.CarrinoA.ChhabraSuperolateral Hoffa’s fat pad edema: association with patellofemoral maltracking and impingementAJR Am J Roentgenol1956201013671373
- C.B.ChungA.SkafB.RogerPatellar tendon-lateral femoral condyle friction syndrome:MR-imaging in 42 patientsSkeletal Radiol302001694697
- D.De VuystF.VanhoenackerA.BernaertsPatellar tendon-lateral femoral condyle friction syndromeJBR-BTR87200430131