Abstract
Background
Monitoring the disease activity in Crohn’s disease (CD) may be challenging with endoscopic manoeuvers due to difficulties in reaching the affected areas and being restricted to mucosal lesions, so the existence of a more tolerable and reliable technique will be highly warranted.
Objectives
This study aims at detection of CD’s activity by computed tomography enterography (CTE) in correlation with ileocolonoscopy evaluation as well as detection of extra-enteric manifestations and complications of the disease.
Materials and methods
Twenty-four patients who were clinically and histopathologically proven as CD patients were retrospectively included in this study. Patients were divided into active and inactive groups according to ileocolonoscopic evaluation. All patients underwent CTE as clinically indicated within 1 week of ileocolonoscopy. Radiological parameters suggestive of Crohn’s disease activity at CTE were interpreted at the terminal ileum and correlated to the corresponding ileocolonoscopy reports for signs of CD activity. Extra-enteric findings and complications of CD were also reported if present.
Results
CTE was accurate in detecting CD activity in 15 out of 18 active cases (active group) and in detecting disease inactivity in 5 out of 6 inactive cases (inactive group) with sensitivity and specificity of 83.3%. Mural hyperenhancement was the most distinguished sign of CD activity in CTE.
Conclusion
CTE is a non invasive and reliable technique that has a significant value in assessment of CD activity in correlation with endoscopy, hence, it is useful in follow up and preoperative guidance.
1 Introduction
Endoscopic examination remains the gold standard in assessment of disease activity in Crohn’s disease (CD). However, the inflammatory process is commonly transmural and thus mucosal appearance only can underestimate its true severity.Citation1,Citation2
Moreover, the extra-enteric complications of CD are hard to detect with endoscopy, and as an invasive method, endoscopy might be intolerable for CD patients who require repeated examinations. Recently, capsule endoscopy has been introduced as an efficient tool and can provide clear images of the small bowel. However, the risk of retention is as high as 8% limiting its clinical applications.Citation3
Former conventional radiological imaging techniques using oral contrast as small bowel follow through and small bowel enteroclysis were not accurate in diagnosing active CD in the small bowel because the findings provided by both methods are limited and indirect as regards the bowel wall and the extra-luminal manifestations of CD. In addition, overlapping of bowel loops may hinder the effectiveness of these methods.Citation4
CT has become the modality of choice for detecting small bowel diseases. CTE unlike abdominopelvic CT better displays the small bowel wall as it depends on ingestion of large volumes of enteric contrast material which distend the small bowel lumen. The use of neutral enteric contrast agents like water, combined with intravenous administration of contrast material, allows excellent assessment of hypervascular lesions and hyperenhancing bowel segments. In addition, CTE displays thin section images and is capable of delineating both enteric and extra-enteric pathology unlike endoscopic or conventional barium studies.Citation5
As CD is a chronic disease characterized by remissions and relapses, multiple examinations may be required to monitor the disease status and the efficacy of treatment. Therefore, an easily performed technique that can be well tolerated by patients and reliable for comparison of multiple examinations needs to be established.
This study aims at detection of CD’s activity by computed tomography enterography (CTE) in correlation with ileocolonoscopy evaluation as well as detection of extra-enteric manifestations and complications of the disease.
2 Materials and methods
2.1 Patients’ selection
This study was conducted from November 2012 to December 2013 in Ain Shams University Specialized Hospital, Cairo, Egypt. We retrospectively studied 24 patients, who were clinically and histopathologically proven as CD, with terminal ileum involvement documented by ileocolonoscopy. Patients were 15 males and 9 females, (mean age: 37.3 ± 11.5 years, range 17–52 years). We included patients with CD who underwent CTE preceded or followed by ileocolonoscopy within 1 week period during their hospital stay, ileocolonoscopy reports were collected for the purpose of our study.
2.2 Ileocolonoscopy
Ileocolonoscopy was performed and reported by an experienced gastroenterologist in terms of the Simple Endoscopic Score for Crohn’s Disease (SES-CD) which states that a score between 0 and 2 suggests inactive disease and ⩾3 suggests active disease.Citation6
2.3 CTE examinations
2.3.1 CTE protocol
All patients who underwent CTE were asked to take nothing by mouth for 6 h before scanning. On the day of examination, patients were asked to come 60 min before exam time, in which patients were asked to ingest a total of 2000 mL of oral water as a neutral contrast material mixed with mannitol (250 mL hyperosmotic mannitol solution to 1750 mL water) over a 60-min period as follows: 0, 15, 30 and 40 min, the last ingestion is just before the scanning. Intramuscular buscopan 20 mg is administered prior to scanning. Intravenous contrast material (Omnipaque, 150 mg) was given at a rate of 4 mL/s then patients were scanned using 12-Multislice CT (Definition Flash, Siemens Medical Systems, Berlin, Germany) from the porta hepatis to the symphysis pubis through single enteric phase acquisition 30–40 s after IV contrast injection. Section thickness used was 1.0 mm and the reconstruction interval was 1 mm. The CT parameters are 280–320 mA, 120 kVp, a pitch of 1.0. CT scans were then transferred to Syngo.via work station for multiplanar reconstructions with section thickness 2 mm and interval 1 mm.
2.3.2 CTE image interpretation
CTE images were interpreted by experienced consultants of gastrointestinal tract radiology who were blinded to patients’ clinical and endoscopic evaluations. They were asked to evaluate the bowel especially the terminal ileum in each CTE exam for; mural thickness and report its value in millimetres (mural thickening is considered if the mural thickness >3 mm) and CT signs of active CD which include; mural hyperattenuation (hyperenhancement) which was detected visually and quantitatively by measuring the CT density at the wall of terminal ileum in Hounsefield Units (HU), mural hyperattenuation was defined as segmental hyperenhancement of the small bowel wall which exceeds the enhancement of the adjacent small bowel loop. Absolute ileal hyperenhancement >109 Hounsefield Units (HU) correlates with active disease,Citation7 mesenteric fat oedema defined as increased density and stranding in perienteric mesenteric fat compared to the perienteric fat adjacent to non-inflamed bowel loops, and comb’s sign which refers to segmental dilatation of the vasa recta supplying a bowel loop. Also CTE signs of inactive CD were interpreted as mural thickening of the bowel wall or bowel stricture in the absence of CTE signs of active disease. The extra-enteric manifestations and complications of CD were also reported with respect to the presence of abscesses, fistula or stricture.
2.4 Statistical analysis
Correlations between CT scan parameters of CD activity and endoscopic scoring were carried out. Comparison of percentages and mean values was done using Student’s t-test. Differences were considered highly statistically significant at a value of <0.001. Statistical analysis was done using SPSS for Windows release 20 (SPSS Inc, Chicago, IL, USA).
3 Results
Our study included retrospectively 24 CD patients; they were studied by CTE and ileocolonoscopy. Patients were divided into two groups according to endoscopy reports of CD activity: active group (18 patients) with SES-CD score ⩾3 and inactive group (6 patients) with SES-CD score <3.
Ileocolonoscopy detected mucosal oedema and erosions as the commonest findings in all 18 patients of the active group, followed by active mucosal ulcers in 14 patients. While in the inactive group, mucosal ulcer scars were the predominant findings.
In our study CTE findings in CD patients are demonstrated in . The most distinguished visual CT finding of active CD was the mural hyperenhancement, followed by mural thickening (–Citation2). Mural thickenings and CTE signs of CD activity were correlated to the reported ileocolonoscopic results and are shown in .
Figure 1 Male patient, 40 years old with 18 year history of Crohn’s disease. CTE (sagital a & b, coronal c & d) shows imaging findings of active Crohn’s disease in which there is multiple ileoileal fistulae. The distal ileum shows mural thickening and hyperenhancement (arrow), it forms a central pocket where the adjacent small bowel loops are sucked in and from which multiple fistulae originate (arrow heads). Engorged vasa rectae “comb sign” is also noted (thin arrows). Ileocolonoscopic examination of this case revealed multiple deep ulcers in edematous terminal ileum with an opening giving to a sinus tract.
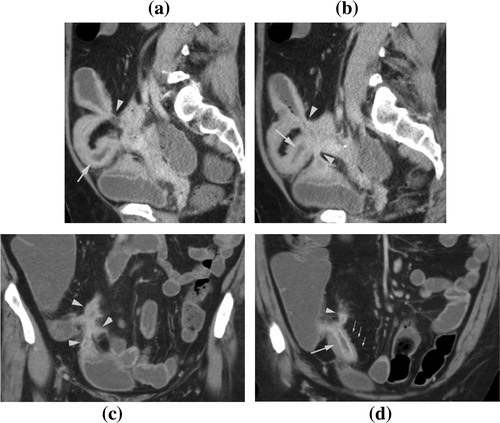
Figure 3 Female patient 45 years old, with 7 month history of Crohn’s disease. Coronal CT enterography (a & b) revealed active form of the disease with mural thickening, hyperenhancement (arrow) of the ileal loops and engorged vasa rectae “comb sign” (arrowheads) denoting increased vascularity. Ileocolonoscopy of this case revealed oedema and active ulceration of the terminal ileum.
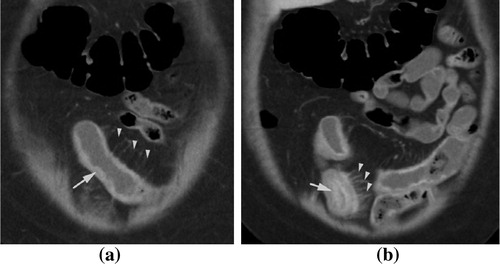
Table 1 CTE enteric and extra-enteric findings reported in CD patients of our study.
Table 2 Mural thickening and CTE signs of CD activity in correlation with ileocolonoscopic results.
Statistical analysis of CTE signs of activity in both active and inactive groups of patients revealed a highly significant difference in the mural hyperenhancement sign (P < 0.001) followed by comb sign (P < 0.05) between the two groups (). No statistically significant difference was found between the two groups concerning the mesenteric fat oedema sign. As regards the mucosal thickening sign, there was a highly statistical significant difference in terms of mean values between the two groups denoting much higher thickening values of bowel wall in the active group, while no significant difference was detected in terms of percentage values.
In correlation with ileocolonoscopic results, CTE correctly diagnosed CD activity in 15 out of 18 patients of the active group with 3 false negative cases. CTE correctly diagnosed 5 out of 6 cases with CD inactivity () with one false positive case. Ileocolonoscopy as the reference standard revealed mild active bowel inflammation in the 3 false negative cases which was not detected by CTE while it revealed disease inactivity in the false positive case by CTE, this was due to collapsed bowel lumen giving the appearance of mural thickening. Our study revealed equal sensitivity and specificity (83.3%) of CTE in detecting CD activity and the positive predictive value (PPV) was 93.7% and negative predictive value (NPV) was 62.5%.
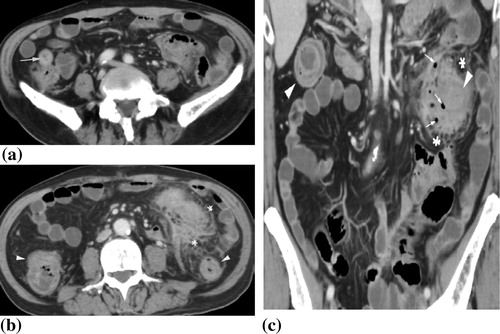
Figure 4 Female patient, 31 years old with 4 year history of Crohn’s disease. (a & b) CT enterography (axial a, coronal b) showing circumferential mural thickening of the terminal ileum with no hyperenhancement (arrow) and narrowing of its lumen and dilatation of the proximal ileal loops (arrowhead), mild ascites is also seen (asterisk). This was an inactive case of Crohn’s disease by CTE which coincides with ileocolonoscopic findings of multiple mucosal ulcer scars.

4 Discussion
CTE has been one of the primary diagnostic tools in the evaluation of patients with Crohn’s disease.Citation8
In reference to ileocolonoscopy, CTE in our study correctly diagnosed active cases of CD in 15 out of 18 patients of the active group and 5 out of 6 cases of the inactive group with PPV of 93.7% and NPV of 62.5%. The sensitivity and specificity of CTE in diagnosing CD activity were 83.3%. There was a highly statistically significant difference with respect to mural hyperenhancement as a sign of CD activity between the active and inactive groups of patients (P < 0.001) while a statistically significant difference (P < 0.05) was found between comb sign as a second sign of CD activity and the mural thickening between the two groups. No statistically significant difference was found between the two groups as regards the mesenteric fat oedema sign.
Larger studies have also shown that findings of CD at CTE correlate highly with endoscopy. For example, in a study carried out by Hashimoto et al.Citation9 in which they compared findings from CTE with those from the mucosal surface in patients with CD, they revealed a strong correlation between CTE findings and mucosal surface findings. Siddiki et al.Citation10 studied 33 patients with CD, they reported CTE sensitivity of 95.2% in detecting active small-bowel CD while in a study of 96 patients who underwent CTE and ileoscopy, bowel wall thickening and hyperenhancement on CTE correlated significantly (p < 0.001) with ileoscopic and histologic findings of active CD.Citation11 In a study comparing CTE, capsule endoscopy, small bowel follow through, and ileocolonoscopy, researchers reported sensitivity of 82% for CTE compared to 74% for ileocolonoscopy and reported that CTE had specificity of 89% compared to 100% for ileoconoscopy.Citation12 Hara and his colleaguesCitation13 observed that CTE findings positively correlated with CD disease progression or regression.
We found mural hyperenhancement sign to be the most visually distinguishable CT finding of CD disease activity followed by terminal ileal thickening.Citation14 Terminal ileal mural hyperenhancement was highly significant in patients with active CD than in patients with inactive CD (p < 0.001) in respect to both percentages and mean value correlation denoting the significant incidence and quantitative value of mural hyperenhancement in the active CD patients. This quantitative finding correlated with visual estimates of disease activity by the reporting radiologists.
Terminal ileal thickening was the second significant CTE sign after mural hyperenhancement between patients of the active and inactive groups. There was a highly statistical significant difference in terms of mean values only between the two groups (p < 0.001) denoting much higher thickening values of bowel wall in the active group, while no significant difference was detected in terms of percentage values revealing the existing incidence of mural thickening in inactive CD.
The commonest extra-enteric complications reported in our study included peri-enteric abscesses and phlegmons () followed by strictures and fistula ().
Figure 2 Male patient 28 years old, with 2 year history of Crohn’s disease. CT enterography (axial a & b, coronal c) revealed active Crohn’s disease with mural thickening and hyperenhancement involving the terminal ileum (arrow) and most of the large bowel (arrowheads). The splenic flexure is the seat of pericolic inflammatory process with stranding of the pericolic fat (asterisk) and multiple air locules (thin arrow) are noted, consistent of a “phlegmon”. Ileoconoscopy of this case revealed colonic and terminal ileum mucosal severe oedema and acute ulcerations consistent with active CD.
Booya et al.Citation15 demonstrated that CT enterography correctly identifies the presence or absence of fistulae in 94% of patients and early adhesions, resulting in changes in the treatment regimen in 61% of patients.
In correlation with ileocolonoscopy, CTE in our study provided a significant correlation in both the active and inactive groups. CT criteria for active disease especially mucosal hyperenhancement and comb sign were good predictors of active CD. In addition, CTE findings aided to assess extra-enteric manifestations of CD and its complications.
5 Conclusions
In conclusion, CTE is a non invasive and reliable technique that has a significant value in assessment of CD activity in correlation with endoscopy, hence, it is useful in follow up and preoperative guidance.
Conflicts of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 2 June 2014
References
- G.D’HaensS.Van DeventerR.Van HogezandD.ChalmersC.KotheF.BaertEndoscopic and histological healing with infliximab anti-tumor necrosis factor antibodies in Crohn’s disease: a European multicenter trialGastroenterology1165199910291034
- P.RutgeertsK.GeboesG.VantrappenJ.BeylsR.KerremansM.HielePredictability of the postoperative course of Crohn’s diseaseGastroenterology9941990956963
- F.LiS.R.GuruduG.De PetrisV.K.SharmaA.D.ShiffR.I.HeighRetention of the capsule endoscope: a single-center experience of 1000 capsule endoscopy proceduresGastrointest Endosc6812008174180
- C.N.BernsteinH.GreenbergI.BoultS.ChubeyC.LeblancL.RynerA prospective comparison study of MRI versus small bowel follow-through in recurrent Crohn’s diseaseAm J Gastroenterol10011200524932502
- S.R.PaulsenJ.E.HuprichJ.G.FletcherF.BooyaB.M.YoungJ.L.FidlerCT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over s700 casesRadiographics2632006641657
- D.N.MoskovitzM.DapernoG.Van AsscheDefining and validating cut-offs for the Simple Endocopic Score for Crohn’s DiseaseGastroenterology1322007S1097
- K.D.BodilyJ.G.FletcherC.A.SolemC.D.JohnsonJ.L.FidlerJ.M.BarlowCrohn disease: mural attenuation and thickness at contrast-enhanced ct enterography—correlation with endoscopic and histologic findings of inflammationRadiology23822006505516
- M.M.Al-HawaryR.K.KazaJ.F.PlattCT enterography: concepts and advances in Crohn’s disease imagingRadiol Clin North Am5112013116
- S.HashimotoK.ShimizuH.ShibataS.KanayamaR.TanabeH.OnodaUtility of computed tomographic enteroclysis/enterography for the assessment of mucosal healing in Crohn’s diseaseGastroenterol Res Pract20132013984916
- H.A.SiddikiJ.L.FidlerJ.G.FletcherS.S.BurtonJ.E.HuprichD.M.HoughProspective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohn’s diseaseAm J Roentgenol19312009 Jul113121
- E.F.StangeS.P.TravisS.VermeireC.BeglingerL.KupcinkasK.GeboesEuropean evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosisGUT5512006115
- C.A.SolemE.V.LoftusJr.J.G.FletcherT.H.BaronC.J.GostoutB.T.PetersenSmall-bowel imaging in Crohn’s disease: a prospective, blinded, 4-way comparison trialGastrointest Endosc6822008255266
- A.K.HaraS.AlamR.I.HeighS.R.GuruduJ.G.HentzJ.A.LeightonUsing CT enterography to monitor Crohn’s disease activity: a preliminary studyAJR1906200815121516
- F.BooyaJ.G.FletcherJ.E.HuorichJ.M.BarlowC.D.JohnsonJ.L.FidlerActive crohn’s disease: CT findings and interobserver agreement for enteric phase CT enterographyRadiology24132006787795
- F.BooyaS.AkramJ.G.FletcherJ.E.HuprichC.D.JohnsonJ.L.FidlerCT enterography and fistulizing Crohn’s disease: clinical benefit and radiographic findingsAbdom Imaging3442009467475
