Abstract
Diabetic nephropathy (DNP) is a microvascular complication that occurs in 20–40% of patients with type 1 diabetes (T1D). The main modifiable DNP initiation and progression factors in susceptible individuals may be sustained hyperglycemia and hypertension. The aim of the present work was to study glycemic control in children with T1D and the risk of microalbuminuria (MA) expressed as the urinary albumin/creatinine ratio (ACR).
Subjects and methods
Forty children with T1D attending the diabetes clinic at the Alexandria University Children’s Hospital with a duration of diabetes of 3 years or more were included in the study and twenty apparently normal children were taken as controls. Clinical examination and blood pressure measurements were performed for all cases. Urine samples were collected within a 3–6 month period. The ACR in 2 of 3 specimens should be >30 mg/g before considering a patient to have microalbuminuria. HbA1c was measured and the mean of the last 4 readings was calculated.
Results
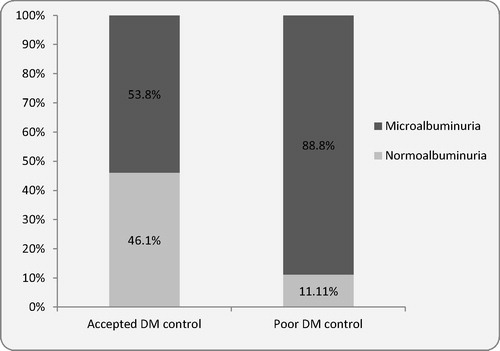
77.5% of patients had ACR >30 mg/g in two different samples. 88.8% of patients with poor glycemic control had MA compared to 53.8% with accepted glycemic control. The difference was more statistically significant among the adolescent age group (P = 0.001). MA was found in 77.2% of children with duration of T1D less than 5 years but the highest proportion was found when the disease duration was more than 10 years. There was no significant difference in systolic and diastolic blood pressure among diabetic children with and without MA (P = 0.556 and 0.781).
Conclusion
Microalbuminuria in children with T1 DM is not limited to those with disease duration of 5 years or more and it may occur earlier. MA is significantly associated with poor glycemic control especially in adolescents. Other factors that may contribute to MA are not yet fully understood, further research is needed to clarify these factors.
1 Introduction
The chronic hyperglycemia of diabetes is mostly associated with long-term damage, dysfunction, and failure of different organs, especially the eyes, kidneys, nerves, heart, and blood vessels.Citation1
Diabetic microvascular and macrovascular complications may have similar etiologic characteristics. Chronic hyperglycemia plays a major role in the initiation of diabetic vascular complications through many metabolic and structural derangements, including the production of advanced glycation end products (AGE), abnormal activation of signaling cascades such as protein kinase C, elevated production of reactive oxygen species (ROS, oxygen-containing molecules that can interact with other biomolecules and result in damage), and abnormal stimulation of hemodynamic regulation systems, such as the renin-angiotensin system [RAS].Citation2
Diabetic nephropathy (DNP) is a microvascular complication that occurs in 20–40% of patients with diabetes and is the single leading cause of end-stage renal disease (ESRD). The main potentially modifiable DNP initiation and progression factors in susceptible individuals may be sustained hyperglycemia and hypertension.Citation3
The earliest clinical evidence of nephropathy is the appearance of low but abnormal levels of albumin in the urine (>30 mg/day or 20 μg/min), referred to as microalbuminuria (MA), and patients with MA are referred to as having incipient nephropathy. Without specific interventions, 80% of subjects with type 1 diabetes who develop sustained MA have their urinary albumin excretion increase at a rate of 10–20% per year to the stage of overt nephropathy or clinical albuminuria (300 mg/24 h or 200 μg/min) over a period of 10–15 years, with hypertension also developing along the way. Once overt nephropathy occurs, without specific interventions, the glomerular filtration rate (GFR) gradually falls over a period of several years at a rate that is highly variable from individual to individual (2–20 ml min−1 year−1). Eventually, ESRD develops in 50% of type 1 diabetic individuals with overt nephropathy within 10 years and in >75% by 20 years.Citation3
The Diabetes Control and Complication Trial (DCCT), a prospective, randomized, controlled trial of intensive versus standard glycemic control in patients with T1D showed that improved glycemic control is associated with significantly decreased rates of microvascular complications (retinopathy, nephropathy and neuropathy).Citation4
However, fewer data exist on the relation between HbA1c and risk of MA in children with type 1 DM.Citation5
The aim of the present work was to study glycemic control in T1D expressed as the mean of the last 4 readings of glycated hemoglobin (HbA1c) and the risk of MA expressed as the urinary albumin/creatinine ratio (ACR).
2 Subjects and methods
This study was conducted on 40 patients diagnosed with T1D attending the diabetes clinic at the Alexandria University Children’s Hospital. The inclusion criteria were: type 1 DM, age: 5–18 years and duration of DM 3 years or more. Patients with evident organ system disease like hemolytic anemia and patients receiving drugs known to affect urinary albumin excretion e.g. corticosteroids, were excluded.
Ethical approval was obtained from the Ethics Committee of the Alexandria Faculty of Medicine and an informed consent was obtained from parents.
All cases were subjected to complete history taking and clinical examination. Arterial blood pressure was measured on the right arm with a standard clinical sphygmomanometer after the patient had been sitting for 10 min. Cases with blood pressure values ⩾90th centile for age were considered prehypertensive while cases ⩾95th centile were considered hypertensive.Citation6
Quantitative determination of microalbumin (μALB) was done by urinary microalbumin–turbilatex which is a quantitative turbidimetric test for measurement of μALB in human urine. Urinary creatinine was measured using an automated colorimetric determination based on a modified Jaffe reaction.Citation7 The albumin/creatinine ratio was obtained by dividing microalbumin (mg/L) by creatinine (g/L). Because of variability in urinary albumin excretion (UAE), two of three specimens collected within a 3–6 month period should be abnormal before considering a patient to have abnormal albumin/creatinine ratio.Citation8
HbA1c was measured by Nyco Card and the mean of the last 4 readings was calculated. The age was considered when setting glycemic goals in children and adolescents with type 1 diabetes i.e. for toddlers, 8.5% was considered accepted, school age <8% and in adolescents <7.5%.Citation9
Data were fed to the computer using SPSS software package version 20. Qualitative data were described using number and percent. Comparison between different groups regarding categorical variables was tested using Chi-square test. Quantitative data were described using mean and standard deviation. Significance was determined as P < 0.05.
3 Results
shows that both cases and controls were comparable as regards age and sex but showed a significant difference in family history of DM (P = <0.001). The mean duration of DM in the cases was 6.77 ± 3.1 years. It shows also that in 31 out of 40 cases (77.5%) ACR was >30 mg/g in two different samples collected within a 3–6 month period. None of the controls had ACR >30 mg/g.
Table 1 Patients with T1 DM and controls according to some socio-demographic characteristics and the prevalence of Microalbuminuria.
shows the age and duration of T1 DM in patients with accepted glucose control versus poor control. The statistical comparison among different groups revealed no statistically significant difference.
Table 2 The age and duration of T1 DM in patients with accepted glucose control versus poor control.
shows that poor glycemic control was associated with higher proportion of MA. Twenty-four out of the 27 cases (88.8%) with poor glycemic control had MA, compared to 7 out of the 13 cases (53.8%) with good glycemic control. The difference was statistically significant (P = 0.013).
shows that 15 out of the 19 school age diabetic children had MA (78.9%), whereas, in adolescents, 16 out of 20 had MA (80%). However, the difference was not statistically significant (P = 0.170).
Table 3 Factors that may affect the occurrence of MA in patients with T1 DM.
There was no significant sex predominance as 78.5% of females were found to have MA compared to 75% of males (P = 0.804).
shows that MA was found in 77.2% of children with a duration of diabetes mellitus less than 5 years but the highest proportion was found when the disease duration was more than 10 years (7 out of 8 cases; 87.5%). However, the differences among the groups were not statistically significant.
also shows that poor glycemic control was generally associated with higher proportion of MA. Fourteen out of the 15 cases with poor glycemic control (93.3%) while only 1 out of the 5 (20%) among those with accepted glycemic control had MA. The difference was only significant among the adolescent group (13–19 years) P = 0.001. There was no significant difference in systolic and diastolic blood pressure among diabetic children with and without MA (P = 0.556 and 0.781, respectively).
4 Discussion
Diabetes mellitus is the most common endocrine metabolic disorder in childhood and adolescence. During the last decade, pediatricians have become increasingly interested in long term complications of diabetes; this is because of the recent scientific developments that allow the detection of minor abnormalities in asymptomatic diabetic patients, and allow early preventive interventions.Citation10
MA is considered to be an early sign of diabetic renal disease. It precedes persistent proteinuria and represents a potentially reversible stage of diabetic nephropathy.Citation11,Citation12 The risk of DNP is highest in those who develop type 1 diabetes in childhood.Citation13 It has been linked to increased levels of advanced glycation end products, disturbed lipid metabolism and abnormalities in hemostasis evidenced by the hypercoagulability due to increased coagulation factors and/or diminished fibrinolytic activity.Citation14,Citation15
The prevalence of early nephropathy as evidenced by elevated ACR, among children and adolescents with type 1 diabetes varies much between different studies. The present study showed that 31 out of 40 diabetic children (77.5%) had early nephropathy which is higher than the average reported by the ADA (20–40%).Citation8 In a Danish study the prevalence was 13%.Citation16 In the United Kingdom, Gizmecioglu et al.Citation17 showed that elevated ACR occurred in 9%, however, less developed countries reported higher figures. In a study in Iraq, MA occurred in 41.4% of patients which is higher than those of the previous two studies but still lower than figures in the present study.Citation18 In an Iranian study MA occurred in 34.6% of 81 diabetic children and adolescents.Citation19 As the previous figures show, the variation is wide and may be related mainly to the degree of diabetes control as it is affected by education, socioeconomic status and the influence of race/ethnicity. Improper collection and storage of urine samples may affect measured levels of MA, as urine proteins are significantly but variably underestimated after storage at −20 °C.Citation20 DNP due to T1D remains a disease involving a heavy burden of morbi-mortality and is difficult to manage in a developing country because of the low socioeconomic level of patients and the lack of reliable epidemiological data.Citation21
In the present study, the relation of glycemic control, expressed as the mean of the last 4 readings of HbA1c, with sex, patient’s age, and the duration of DM was examined. More than two thirds of patients (67.5%) had poor glycemic control according to age-adjusted HbA1c targets. This was higher than previously reported from Egypt. Mohamed et al, reported that children with poor glycemic control occurred in 45.8%, but it was still lower than that reported in other developing countries like Iran, where abnormal HbA1c occurred in 82.7% of patients.Citation3,Citation19
The degree of glycemic control among the different age groups revealed no statistically significant difference; Mohamed et al., reported that children with poor glycemic control had significantly higher mean age.Citation13 Similarly, Vanelli et al.Citation22 reported that increasing age was associated with a higher mean HbA1c and a decreased likelihood of attaining HbA1c in the target range regardless of the insulin regimen. It has been argued that poor glycemic control in adolescents is directly proportional to increasing age. This may be related to physiologic insulin resistance because of increased sex steroids, growth hormone and diminished free Insulin-like growth factor 1 (IGF1). Furthermore, pubertal development and the transition to adulthood are associated with problems in adapting to lifestyle that requires self management of dietary practices, exercise behavior, insulin adjustment and adherence to treatment management.Citation8 The present results showed that poor glycemic control was associated with higher proportion of nephropathy as 88.8% of cases with poor glycemic control had increased ACR, compared to 53.8% with good glycemic control (P = 0.013). This was more evident in the adolescent age group as 93.3% with poor glycemic control had abnormal albumin/creatinine ratio compared to 20% with good glycemic control (P = 0.001). These results show a significant relationship between the degree of glycemic control and the occurrence of nephropathy and are in agreement with the epidemiological analysis of the DCCT and the United Kingdom Prospective Diabetes Study (UKPDS) where a curvilinear relationship between HbA1c and microvascular complication was demonstrated.Citation4
In an Iranian study it was shown that poor glycemic control was observed in 82.7%; however, there was no correlation between MA and HbA1c.Citation19 Chae et al. showed that the mean HbA1c levels were significantly higher in the MA group than in the normoalbuminuria group suggesting that the incidence of DNP increases according to the degree of glycemic control.Citation23
The present work showed that the highest proportion of cases with nephropathy was found if the duration of diabetes was more than 10 years (7 out of 8 cases, 87.5%). However, the differences among the groups were not statistically significant. Chae et al.Citation23 observed that the duration of diabetes was significantly higher in the microalbuminuria group while Basiratnia et al.Citation19observed there was no significant correlation between the duration and microalbuminuria. This insignificant correlation between MA and the duration of DM may be explained by the fact that the mean duration of DM in this study was 6.77 ± 3.1 years, which may be considered a short time to develop nephropathy. Surprisingly, MA was found in 77.2% of children with a duration of diabetes mellitus less than 5 years. It was concluded by Alleyn et al.Citation24 that microalbuminuria in older children with type 1 diabetes is likely to be clinically significant. In younger children, it may reflect functional, reversible renal changes.
Hypertension is another modifiable risk factor that accelerates the progression of micro- and macrovascular complications.Citation8 Gross and coworkers suggested that the development and progression of MA is closely linked to hypertension.Citation25 Other studies suggest that impairment of blood pressure regulation begins at nighttime with a higher prevalence than microalbuminuria. However, office blood pressure measurement did not rise before the onset of microalbuminuria.Citation26 In the present study, systolic and diastolic blood pressure did not significantly differ among cases with and without MA. Various studies have revealed conflicting results; some of these studies did not show any significant role of blood pressure on MA,Citation22 while others have revealed that high blood pressure, especially diastolic pressure, is one of the important predictors of developing MA. It is possible that blood pressure only increases in relation to the onset of microalbuminuria, either shortly before or after, and thus only is a short term risk factor. Another possibility is that the changes in blood pressure initially are so small that they are not detectable with baseline office measurements and that 24-h ambulatory blood pressure measurement is necessary to demonstrate their presence.Citation27,Citation28 However, the relationship between MA and blood pressure is still controversial. It may be claimed that blood pressure is not an important initiating factor for MA in children with type 1 diabetes.Citation29,Citation30 Conflicting results may be related also to the different methods used in measuring blood pressure especially in children.
In conclusion, microalbuminuria in children with T1 DM is not limited to those with disease duration 5 years or more and it may occur earlier. MA is significantly associated with poor glycemic control especially in adolescents. Other factors that may contribute to MA are not yet fully understood, further research is needed to clarify these factors.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 2 June 2014
References
- American Diabetes AssociationDiagnosis and classification of diabetes mellitusDiabetes Care33Suppl. 12010S62S69
- W.T.CadeDiabetes-related microvascular and macrovascular diseases in the physical therapy settingPhys Ther8811200813221335
- American Diabetes AssociationNephropathy in diabetesDiabetes CareSuppl. 12004S79S83
- D.M.NathanP.A.ClearyJ.Y.BacklundS.M.GenuthDiabetes control and complications trial/epidemiology of diabetes interventions and complications (DCCT/EDIC) study research group, intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetesN Engl Med353200526432653
- American Diabetes AssociationStandards of medical care in diabetesDiabetes Care3420111161
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and AdolescentsThe fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescentsPediatrics1142 Suppl. 4th Report2004555576
- E.LambC.P.PriceKidney function testsC.A.BurtisE.R.AshwoodD.E.BrunsTietz textbook of clinical chemistry and molecular diagnostics4th ed.2006St Louis: Elsevier, Saunders Company 797–783
- American Diabetes AssociationStandards of medical care in diabetesDiabetes Care35Suppl. 12012s11s63
- J.SilversteinG.KlingensmithK.CopelandL.PlotnickF.KaufmanL.LaffelCare of children and adolescents with type 1 diabetes: a statement of the American Diabetes AssociationDiabetes Care282005186212
- P.Cavallo-PerinE.LupiaG.GrudenC.OlivettiA.De MartinoM.CassaderIncreasing blood levels of platelet-activating factor in insulin-dependent diabetic patients with microalbuminuriaNephrol Dial Transplant152000994999
- American Diabetes AssociationClinical practice recommendations nephropathy screening and treatmentDiabetes Care2812005s18s19
- H.H.ParvingH.HommelE.MathiesenPrevalence of microalbuminuria, arterial hypertension, retinopathy and neuropathy in patients with insulin dependent diabetesBMJ2961988156160
- H.A.MohammadH.S.FarghalyK.A.MetwalleyE.M.MonazeaH.A.Abd El-HafeezPredictors of glycemic control in children with type 1 diabetes mellitus in Assiut-Egypt. IndianJ Endocrinol Metab162012796802
- M.SmallG.D.O.LoweA.C.MaccuishC.D.ForbesThrombin and plasmin activity in diabetes mellitus and their association with glycemic controlQJ Med65198710251031
- A.R.AndersonJ.S.ChristiansenJ.K.AndersonS.KriennreT.DeckertDiabetic nephropathy in type 1 (insulin-dependent) diabetes: an epidemiological studyDiabetologia251983496501
- H.B.MortensenP.HougaardK.K.IbsenH.H.ParvingDanish study group of diabetes in childhood, relationship between blood pressure and urinary albumin excretion rate in young Danish type 1 diabetic patients: comparison to non diabetic childrenDiabetic Med111994155161
- F.M.GizmeciogluK.NoyesL.BathC.KelnarAudit of microalbumin excretion in children with type 1 diabetesJCRPE132009136143
- J.K.AtiyaM.K.HassanL.M.Al-NaamaMicroalbuminuria in children and adolescents with type 1 diabetes mellitusMJBU2522007511
- M.BasiratniaS.F.AbadiG.H.AmirhakimiAmbulatory blood pressure monitoring in children and adolescents with type-1 diabetes mellitus and its relation to diabetic control and microalbuminuriaSaudi J Kidney Dis Transplant2322012311315
- C.J.SchultzR.N.DaltonC.TurnerH.A.NeilD.B.DungerFreezing method affects the concentration and variability of urine proteins and the interpretation of data on microalbuminuriaDiabetic Med1712000714
- Y.BentataI.HaddiyaH.LatrechK.SerrajR.AbouqalProgression of diabetic nephropathy, risk of end-stage renal disease and mortality in patients with type-1 diabetesSaudi J Kidney Dis Transplant2422013392402
- M.VanelliF.CeruttiR.LoriniF.MeschiMCDC-Italy Group. Nationwide cross sectional survey of 3560 children and adolescents with diabetes in ItalyJ Endocrinol Invest282005692699
- H.W.ChaeJ.I.I.ShinH.S.KimD.H.KimSpot urine albumin to creatinine ratio and serum cystatin C are effective for detection of diabetic nephropathy in childhood diabetic patientsJ Korean Med Sci272012784787
- C.R.AlleynL.K.VolkeningJ.WolfsonA.Rodriguez-VenturaJ.R.WoodL.M.LaffelOccurrence of microalbuminuria in young people with type 1 diabetes: importance of age and diabetes durationDiabetic Med2752010532537
- J.L.GrossM.J.De-AzevedoS.P.SilveiroL.H.CananiM.L.CaramoriT.ZelmanovitzDiabetic nephropathy: diagnosis, prevention and treatmentDiabetes Care2812005164176
- A.DostC.KlinkertT.KapellentArterial hypertension determined by ambulatory blood pressure profiles: contribution to microalbuminuria risk in multicenter investigation in 2105 children and adolescent with diabetes mellitus type 1Diabetes Care312008720725
- S.DarcanD.GoksenS.MirAlteration of blood pressure in type 1 diabetic children and adolescentsPediatr Nephrol212006672676
- P.RossingP.HougaardH.H.ParvingRisk factors for development of incipient and overt diabetic nephropathy in type 1 diabetic patients: a 10-year prospective observational studyDiabetes Care2552002859864
- C.J.SchultzH.A.W.NeilR.N.DaltonT.Konopelska BahuD.B.DungerBlood pressure does not rise before the onset of microalbuminuria in children followed from diagnosis of type 1 diabetes. Oxford Regional Prospective Study GroupDiabetes Care242001555560
- J.IncertiT.ZelmanovitzJ.L.CamargoJ.L.GrossM.J.de AzevedoEvaluation of tests for microalbuminuria screening in patients with diabetesNephrol Dial Transplant20200524022407