Abstract
We reported a Jordanian case of Cogan’s Syndrome (CS). A 22-year old male patient presented with interstitial keratitis. The patient was treated successfully with topical steroids but over the following months, he developed vertigo, sensorineural hearing loss (SNHL) and generalized vasculitis. This is the first reported case of CS in Jordanian population.
1 Introduction
Cogan’s Syndrome (CS) is a rare immune-mediated disease characterized by ocular inflammation and audiovestibular dysfunction with or without vasculitis or other systemic manifestations.Citation3,Citation4 The syndrome affects primarily young adults and gives a clinical picture of systemic disease or vasculitis in 1/3 of patients. The prognosis is dominated by the risk of definitive deafness and cardiovascular complications. We reported the clinical and audiological findings for a Jordanian patient with interstitial keratitis, vertigo and sensorineural hearing loss and vasculitis. The clinical picture suggests the diagnosis of Cogan’s Syndrome.
2 Case report
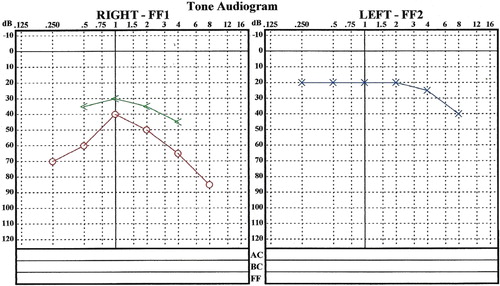
A 22-year-old Jordanian male university student was admitted to hospital in November 2010 complaining of burning sensation in his eyes and severe light sensitivity. Otherwise, the patient was not known to have any other illness. His medical and surgical history was positive for a previous history of uneventful keratoplasty seven years ago. The initial diagnosis was stromal keratitis. Therefore, topical steroids were used for the treatment. The patient improved but three months later, he had an attack of vertigo, vomiting, and he gradually developed hearing loss and tinnitus. Pure tone audiogram showed right moderate SNHL and left mild SNHL (). The attack lasted for two weeks.
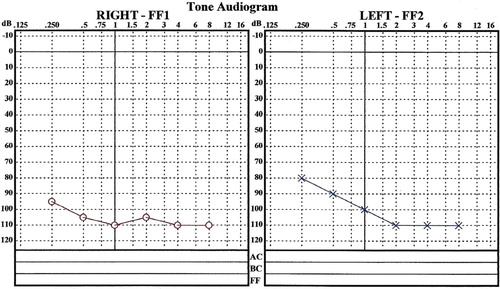
Three weeks later, a pure tone audiogram () revealed right moderate to severe SNHL mainly at low frequencies and left mild to moderate SNHL mainly at low frequencies (). Electrocochleography was conducted using click stimuli at 95 dB Normal Hearing Level (NHL). The results showed a high summating potential/action potential (SP/AP) ratio in the right ear of more than 60% and a mild elevation in the SP/AP ratio in the left ear of about 40%. The obtained results showed endolymphatic hydrops and were consistent with cochlear Meniere’s disease. CT and MRI of the brain and the internal auditory meatus showed no structural lesions. The patient was treated with betahistine dihydrochloride 16 mg three times daily. Although vertigo subsided after two weeks, the hearing loss continued (). Six months after the first presentation, the patient presented to hospital with fever, polyarthralgia, and recent weight loss. His echocardiography showed trace mitral and tricuspid regurgitations, normal pulmonary artery pressure, and mild to moderate left ventricular impairment (EF 40–45%). The laboratory investigations of the patient are shown in . Serological tests for syphilis and TB were negative (). Finally, the case was diagnosed as Cogan’s Syndrome. Therefore, the treatment consisted of methotrexate (six 2.5 mg tabs, one day a week) and folic acid for two months, and prednisolone 50 mg daily. Due to hematuria and renal impairment, methotrexate was replaced by azathioprine tablets 50 mg, three times daily. There was an improvement in the patient vision and the general symptoms of vasculitis but the hearing worsened.
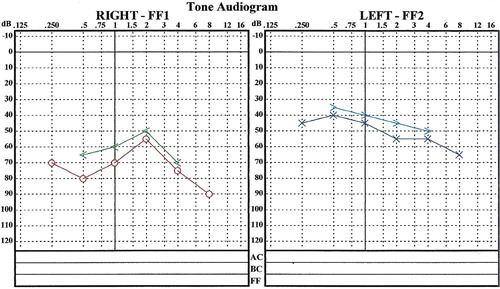
Table 1 Laboratory and radiological findings of the patient at the time of the initial presentation with vasculitis.
Table 2 Serological tests for syphilis and TB.
3 Discussion
Cogan’s Syndrome was first described by Dr. David G. Cogan (1908–1993) in 1945 as a non-syphilitic interstitial keratitis with vestibuloauditory symptoms.Citation9 CS is rare, with fewer than 250 reported cases in the literature, and is mostly described in young adult Caucasian patients of both sexes.Citation4 CS is an extremely rare disorder in Arabic and Middle Eastern countries.Citation1 The novelty of our case report is that it is the first reported in Jordan (estimated population in 2012 was 6,388,000).
The classical form of ocular involvement in CS is characterized by the interstitial keratitis. However, iritis or uveitis, scleritis or episcleritis, and conjunctivitis have been also described, and the atypical CS exists in the absence of interstitial keratitis.Citation4 Some systemic manifestations have been reported in association with CS, including vasculitis of the aorta leading to aortic aneurysm and/or aortic valve regurgitation, fever, arthralgia (or arthritis), lymphadenopathy, splenomegaly, skin rash, and peripheral or central nervous system involvement.Citation3,Citation4
The ocular involvement in CS usually gives a good response to topical corticosteroid therapy, while, systemic corticosteroids are reserved for unresponsive cases or those with posterior uveitis, it was reported that poor long term ophthalmologic outcomes due to CS are unusual in contrast to vestibuloauditory affection.Citation3,Citation7
Deafness is the most common serious outcome of CS and systemic corticosteroid therapy is warranted as soon as possible after the onset of hearing loss,Citation5,Citation6,Citation12,Citation14 with the recommendation of an initial dose therapy of 1 mg/kg (0.5–2) per day of prednisone.Citation4 If an improvement in hearing is observed (objectively and subjectively), corticosteroids are gradually tapered over 2–6 months.Citation14 However, reductions in the corticosteroid dose are contingent upon stable auditory acuity and vestibular function.Citation11 Certain patients may require long-term corticosteroid therapy because of the recurrent hearing loss during attempts to taper the prednisone dose,Citation1 so, azathioprine, cyclophosphamide, cyclosporine, methotrexate, and tumor necrosis factor (TNF)-alpha blockers have been recommended.Citation4,Citation12,Citation13 Some patients may show unresponsiveness to such a therapy, thereby resulting in severe hearing loss as in our case.
In the presented case, as the others reported in the literature, the patient showed only leukocytosis and elevated erythrocyte sedimentation rate (ESR). Sometimes, there is an elevation in the level of C-reactive protein (CRP), but often no alteration in inflammation parameters is observed, therefore, no specific diagnostic test is performed.Citation2
The results of radiographic studies of CS cases, such as cranial CT and MRI, are often normal; which could be useful in the exclusion of other causes of vestibuloauditory symptoms such as stroke or neoplasm.Citation5
CS is a cause of progressive deafness; it is assumed to be an “autoimmune disease”.Citation8,Citation10 However, this disease needs to be accurately documented and described in order to offer a better understanding of the pathogenesis and to contribute toward developing efficacious early treatment. Follow-up of patients presenting sudden or rapidly progressive hearing loss, with or without vestibular symptoms, is also crucial, because these symptoms could represent the initial manifestation of CS. Since about two thirds of patients meet the classic diagnostic criteria for CS,Citation5 the follow-up of patients who present only vestibuloauditory symptoms should be guaranteed for at least two years.
Conflict of interest
The authors do not report any conflict of interest.
Acknowledgement
We would like to thank Dr. Jameel Hijazeen for his help in typing and formatting the manuscript.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 5 September 2014
References
- A.Al-RashidiA.A.MareyM.O.HegaziCogan’s Syndrome: a case reportIran J Immunol52008222225
- R.BovoC.AimoniA.MartiniImmune-mediated inner ear diseaseActa Otolaryngol126200610121021
- M.B.GluthK.H.BaratzE.L.Eric L MattesonC.L.DriscollCogan Syndrome: a retrospective review of 60 patients throughout a half centuryMayo clinic proceedings2006Elsevierp.483–8.
- A.GraslandJ.PouchotE.HachullaO.BletryT.PapoP.VinceneuxTypical and atypical Cogan’s Syndrome: 32 cases and review of the literatureRheumatology (Oxford)43200410071015
- B.F.HaynesM.I.Kaiser-KupferP.MasonA.S.FauciCogan Syndrome: studies in thirteen patients, long-term follow-up, and a review of the literatureMedicine (Baltimore)591980426441
- B.F.HaynesA.PikusM.Kaiser-KupferA.S.FauciSuccessful treatment of sudden hearing loss in Cogan’s Syndrome with corticosteroidsArthritis Rheum241981501503
- A.KesselZ.VadaszE.ToubiCogan Syndrome—pathogenesis, clinical variants and treatment approachesAutoimmun Rev134–52014351354
- C.LunardiC.BasonM.LeandriR.NavoneM.LestaniE.MilloAutoantibodies to inner ear and endothelial antigens in Cogan’s SyndromeThe Lancet3602002915921
- E.W.NortonD.G.CoganSyndrome of nonsyphilitic interstitial keratitis and vestibuloauditory symptoms: a long-term follow-upAMA Arch Ophthalmol611959695697
- U.PleyerH.E.BaykalJ.M.RohrbachM.BohndorfP.RieckJ.ReimannCogan I Syndrome: too often detected too late? A Contribution to early diagnosis of Cogan I SyndromeKlin Monbl Augenheilkd2071995310
- R.M.McCallumCogan’s SyndromeF.T.FranunfelderR.HamptonCurrent ocular therapy1993WB Saunders CompanyPhiladelphiap.410
- O.E.Tayer-ShifmanO.IlanH.ToviY.TalCogan’s Syndrome—clinical guidelines and novel therapeutic approachesClin Rev Allergy Immunol20141810.1007/s12016-013-8406-7
- Z.ToumaR.NawwarU.HadiM.HouraniT.ArayssiThe use of Tnf-A blockers in Cogan’s SyndromeRheumatol Int272007995996
- R.VollertsenT.J.McDonaldB.R.YoungeP.M.BanksA.W.StansonD.M.IlstrupCogan’s Syndrome: 18 cases and a review of the literatureMayo clinic proceedings1986Elsevierp.344–61