Abstract
Lateral mass cervical fixation is the technique of choice for posterior cervical stabilization of the lower cervical spine in the cases of cervical spondylotic myelopathy. It is used for patients who had extensive, multiple-level laminectomies with reversed cervical lordosis.
Objective
The aim of this study was to evaluate the outcome of decompressive laminectomy of cervical spondylotic myelopathy with lateral mass fixation compared with decompressive laminectomy only without fixation.
Patients and methods
The study was conducted on 32 patients operated for cervical decompressive laminectomy with lateral mass fixation using polyaxial screws and rods at different levels of the subaxial cervical spine named group I, compared with 30 patients operated for cervical decompressive laminectomy only without lateral mass fixation named group II.
Results
Group I comprised 22 males (68.8%) and 10 females (31.2%), the age ranged from 36 to 63 years. Group II comprised 18 males (60%) and 12 females (40%), the age ranged from 40 to 66 years with a mean of 51 ± 7.73. In group I, the mean operative time was 110 ± 14.16 min, the mean hospital stay was 4 ± 1.76 days and the mean blood loss was 480 ± 193.04 ml. In group II, the mean operative time was 75 ± 24.38 min, the mean hospital stay was 3 ± 1.57 days, and the mean blood loss was 220 ± 111.22 ml. There was a clinically significant difference as regards neck pain and brachialgia. In group I, neck pain improved in 68.8% and brachialgia improved in 83.3% but in group II, neck pain improved in 46.7% and brachialgia improved in 61.5%. Myelopathy and sphincteric disturbance showed clinical improvement but without clinically significant difference of both groups.
Conclusions
Lateral mass fixation of the cervical spine after cervical laminectomy is safe and reliable with few complications. It also improves neck pain and brachialgia.
1 Introduction
Lateral mass cervical fixation is the technique of choice for posterior cervical stabilization for treating instability of the lower cervical spine after extensive multiple-level cervical laminectomies with reversed lordosis.Citation2,Citation14 It is safe and reliable, but it is difficult to be used in patients with abnormal cervical anatomy as it may lead to injury of the spinal nerves or the vertebral arteries during the insertion of lateral mass screws.Citation2,Citation22 Roy-Camille was the first to insert screws into the lateral mass of the cervical spine in 1964 in France followed by Louis and Magerl in Switzerland.Citation15,Citation17
There are many different techniques of posterior cervical fixation as posterior wiring,Citation3 Halifax clamps,Citation1 posterior plate and screws,Citation9 and finally fixation using polyaxial screws and rods .Citation23 Wiring is rarely used as it is used only if the lamina and spinous process of the posterior element of the subaxial spine are intact and it could not be used in cases where laminectomies have been required for the decompression or exposure of target lesions.Citation3,Citation12 The main disadvantage of wiring is that it provides less fixation strength in comparison with other rigid instrumentations.Citation3 Halifax clamps may provide better fixation strength than wiring but are still not optimal.Citation1 Lateral mass screws with plate fixation require precise contour tailoring for each patient and are thus extremely difficult for practical application.Citation9 Recently, the technique of using polyaxial screws in conjunction with rod systems for the fixation of the lateral mass was greatly increased as it can avoid the above-mentioned disadvantages.Citation16–Citation17Citation18Citation19
2 Patients and methods
The study was conducted on 2 groups. 32 patients operated for cervical decompressive laminectomy with lateral mass fixation using the modified Magerl technique at various levels from C3 to C7 according to the patient’s requirements named group I, compared with another 30 patients operated for cervical decompressive laminectomy only without lateral mass fixation named group II. All the patients were operated in the Neurosurgery Department of the Main Alexandria University Hospital and the classification of the patients into group I and group II was random and the 2 groups were nearly the same as regards the clinical presentations, the cord signal, and the number of levels affected. Informed consent was obtained from all the patients before study.
All the patients were operated in prone position with the head slightly flexed. Posterior midline approach was done followed by dissection of the paravertebral muscles with exposure of the lamina extending from C1 to C7. In group I the dissection extended laterally till full exposure of the lateral mass and facets. The lateral border of each lateral mass was dissected which is a very important step for placing of the screws. The screws were placed into lateral mass of the affected levels of the subaxial cervical spine before laminectomies so that the bony landmarks can be used for better orientation. The entry point of the screw was identified 2 mm inferior and 2 mm medial to the center of the lateral mass using a high speed drill with a trajectory 30 mm lateral and 30–45 mm superior more or less parallel to the spinous process. The spinous processes should be fixed during the process of drilling and screw placement. Fluoroscopy was not necessary during the placement of the screws, but required whenever we felt not confident enough or after the screws were inserted. The patient then underwent laminectomy for decompression, then the rod was inserted and the screw nuts were tightened. Finally the posterior lateral aspects of the lateral mass and the facet joint underwent decortication for bony fusion using bone grafts. Drainage catheters were placed before the closure of the wound.
The patients were followed up for at least 6 months. Plain X-ray cervical spine was done in AP and lateral study before discharge from the hospital and at 2 months interval later on. The patients were recommended to wear hard cervical collar for at least 6 weeks postoperative, bony fusion recorded within this period of follow up.
3 Results
The 2 groups were operated, group I comprised 32 patients (100%) operated with decompressive laminectomy with lateral mass fixation. It comprised 22 males (68.8%) and 10 females (31.2%), the age ranged from 36 to 63 years with a mean of 48.0 ± 8.68. Group II comprised 30 patients (100%) operated upon by decompressive laminectomy only without fixation, it comprised 18 males (60%) and 12 females (40%), the age ranged from 40 to 66 years with a mean of 51 ± 7.73 ().
Table 1 Age and gender of the patients.
In group I, neck pain was the most commonly present in all the 32 patients (100%) followed by brachialgia in 18 patients (56.3%). Myelopathy was present in 26 patients (81.3%) according to the JOA-score, grade 1 myelopathy in 16 patients (61.6%), grade 2 myelopathy in 7 patients (26.9%) and only 3 patients (11.5%) with grade 3 myelopathy. Sphincteric disturbance was present in 11 patients (34.4%). In group II, neck pain was present in 30 patients (100%) followed by brachialgia in 26 patients (86.7%). Myelopathy was present in 28 patients (93.3%), grade 1 myelopathy in 10 patients (35.7%), grade 2 myelopathy in 14 patients (50%) and 4 patients (14.3%) with grade 3 myelopathy. Sphincteric disturbance was present in 10 patients (33.3%) ().
Table 2 The clinical presentation of the patients.
In group I, the operative time ranged from 90 to 140 min with a mean of 110 ± 14.16 min, the hospital stay ranged from 2 to 7 days with a mean of 4 ± 1.76 days and the blood loss ranged from 250 to 800 ml with a mean of 480 ± 193.04 ml. In group II, the operative time ranged from 45 to 120 min with a mean of 75 ± 24.38 min, the hospital stay ranged from 1 to 6 days with a mean of 3 ± 1.57 days and the blood loss ranged from 100 to 450 ml with a mean of 220 ± 111.22 ml ().
Table 3 Operative data of the two groups.
In group I, 18 patients (56.3%) were operated from C3 to C6 levels followed by C3–7 in 8 patients (25%), 4 patients (12.5%) from C4 to C7 and lastly 2 patients (6.2%) from C4 to C6 ().
Table 4 Laminectomy levels and fixation in group I.
A total of 268 screws were used most of them (252 screws)(94%) were 3.5 mm in thickness and 16 screws (6%) were 4 mm as revision screws. 6 screws were used in 2 patients (6.3%), 8 screws were used in 22 patients (68.7%), and 10 screws were used in 8 patients (25%). The length of screws varied from patient to patient and according to the level of fixation we found that 14 screws (5.2%) were 12 mm in length, 70 screws (26.1) 14 mm, 160 screws (59.7%) 16 mm and finally 24 screws (9%) 18 mm ().
Table 5 Instrument profile.
As regards the complications, we found no recorded cases of spinal cord injury or spinal nerve root injury in both groups. In group I screw pullout occurred in 4 screws of 268 screws used in 4 different patients that were managed conservatively as there was no complaint from them (12.5%). Dural tear was present in 2 patients (6.3%) in group I and 1 patient (3.3%) in group II. Postoperative neurological deficit occurred in 2 patients in group I (6.3%) and 3 patients (10%) in group II in comparison with the preoperative condition of the patients. In group I, we found that 2 patients (6.3%) complained of posterior circulation ischemia as vertigo, dizziness and vomiting mostly due to excessive epidural hemorrhage during dissection and screw insertion. No wrong level was detected in postoperative radiography. In group I, we recorded 3 patients (9.4%) complained of superficial wound infection that was treated medically in comparison with 2 patients (6.7%) in group II. No recorded cases of vertebral artery injury were found ().
Table 6 Complications in the 2 groups.
In group I, plain X-ray was done in A–P and lateral positions for all the patients immediately postoperative and after 2 month interval till bony fusion was detected. Bony fusion was achieved in all the patients after 6 month follow up. Stability of the fixation was confirmed in postoperative X-ray in flexion and extension films in all the patients.
As regards the outcome of the patients according to the clinical conditions determined by the visual analog scale VAS we found that in group I, neck pain improved in 22 patients (68.8%) and 8 patients (25%) remained stationary without improvement and only 2 patients (6.2%) deteriorated mostly due to wound infection, but in group II we found that neck pain improved in 14 patients (46.7%) and 7 patients (23.3%) remained stationary without improvement and 9 patients (30%) deteriorated mostly due to increased kyphosis. This indicates that neck pain improved much better in group I in comparison with group II with positive clinical significance test.
As regards brachialgia, determined by the visual analog scale VAS, we found in group I, brachialgia improved in 15 patients (83.3%) and 2 patients (11.1%) remained stationary without improvement and only 1 patient (5.6%) deteriorated mostly due to dural tear intraoperative, but in group II we found that brachialgia improved in 16 patients (61.5%) and 7 patients (29.9%) remained stationary without improvement and 3 patients (11.5%) deteriorated mostly due to foraminal stenosis. This indicates that brachialgia improved much better in group I in comparison with group II with positive clinical significance test.
As regards the myelopathy and sphincteric disturbance, we found that both group I and group II showed improvement of the 3 grades but without any clinically significant difference ( and ).
Figure 1 (A) Preoperative plain X-ray cervical spine lateral view of a male patient 57 years old presented with quadromyelopathy, operated with cervical laminectomy with lateral mass fixation, (B) Preoperative multislice CT cervical spine, (C, D) Sagittal MRI T2 weighted image of the cervical spine of the same patient before surgery, (E, F) fluoroscopic photo of the cervical spine after the insertion of the screws in lateral view of the same patient, (G) operative photo of the same patient after fixation.
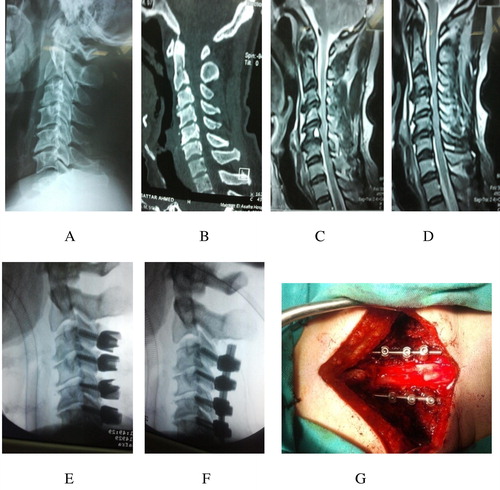
Table 7 Outcome as regards the clinical presentation of the patients.
4 Discussion
Lateral mass cervical fixation is good technique for posterior cervical stabilization for treating instability of the lower cervical spine after extensive multiple-level cervical laminectomies with reversed lordosis.Citation2–Citation3Citation4Citation5Citation6Citation7Citation8Citation9Citation10Citation11Citation12Citation13Citation14 It is safe and reliable, but it is difficult to be used in patients with abnormal cervical anatomy. In this study, 2 groups were operated, group I comprised 32 patients (100%) operated with decompressive laminectomy with lateral mass fixation. It comprised 22 males (68.8%) and 10 females (31.2%). Group II comprised 30 patients (100%) operated upon by decompressive laminectomy only without fixation, it comprised 18 males (60%) and 12 females (40%). In both groups we found that males are more affected than females as they were more exposed to trauma but there were no significant statistical differences between both groups as regards the sex. This was matched with other studies by Watter and LevinthalCitation21 who showed that males were more affected than females (61% males and 39% females) in a similar study and also Olaorie and ThomasCitation13 who found that males are commonly affected than females (65 males to 35 females) in another study.
In group I, the age ranged from 36 to 63 years with a mean of 48.0 ± 8.68, and in group II, the age ranged from 40 to 66 years with a mean of 51 ± 7.73. These are mostly because decompressive laminectomy is usually done in the old age group but there was no significantly statistical differences between both groups as regards the age which are matched with many studies as in Watter and LevinthalCitation21 study who showed that the average age was 46 years and Olaorie and ThomasCitation13 showed that the average age was 47 years, and finally JankowitzCitation8 showed that the average age was 50–60 years in a large series.
In group I, neck pain was most commonly present in all the patients (100%) followed by brachialgia in 56.3%. Myelopathy was present in 81.3%, grade 1 myelopathy in 61.6% and grade 2 myelopathy in 26.9% and 11.5% with grade 3 myelopathy. Sphincteric disturbance was present in 34.4%. In group II, neck pain was present in 100% of patients followed by brachialgia in 86.7%. Myelopathy was present in 93.3%, grade 1 myelopathy in 35.7% and grade 2 myelopathy in 50% and 14.3% with grade 3 myelopathy. Sphincteric disturbance was present in 33.3%.
There was a significant difference as regards the improvement of neck pain and brachialgia between both groups. We found that the improvement of neck pain in group I was 68.8% in comparison with 46.7% in group II and also brachialgia improved in group I (83.3%) in relation to group II (61.5%). The improvement was mostly due to the stability of the cervical spine after fixation and widening of the intervertebral foramen to decompress the nerve root in group I. This was matched with other studies as Epstein and JaninCitation4 recorded 85% improvement after cervical laminectomy with fixation in comparison with other posterior laminectomy. This improvement is much better if we removed the anterior osteophytes through poster lateral approach. HerkowitzCitation7 found that the incidence of postoperative kyphosis after cervical laminectomy with partial medial facetectomy was 25% after 2 year follow up period leading to recurrent neck pain and brachialgia, also Symon and LavenderCitation17 recorded 70% improvement in patients operated with cervical laminectomy only without fixation in comparison with 85% improvement after fixation.
As regards the myelopathy and sphincteric disturbance, we found that both group I and group II showed improvement of 3 grades of myelopathy but without any clinically significant difference. The improvement of grade 1 myelopathy was 75% in group I in relation to 70% in group II and grade 2 improvement was 57.1% in both groups and in grade 3 the improvement was 33.3% in group I to 50% in group II, and finally the sphincteric disturbance improved in both groups to 45.5% in group I and to 40% in group II. This was mostly due to the same decompression of the cord without clinical difference in both groups. Kumar et al.Citation11 recorded 80% improvement with good outcome and 76% improvement in myelopathy score after cervical laminectomy with lateral mass fixation.
There was a significant difference between both groups as regards the operative time, blood loss and the hospital stay. We found that in group I, the mean operative time was 110 ± 14.16 min but in group II, was 75 ± 24.38 min, and p value < 0.001∗. The mean hospital stay in group I was 4 ± 1.76 days and in group II, was 3 ± 1.57 days with p value < 0.046∗. Finally, the mean blood loss in group I, was 480 ± 193.04 ml and in group II, was 220 ± 111.22 ml, with p value < 0.001∗. The blood loss in group I is more than that in group II due to long operative time and lateral dissection during surgery with the injury of the epidural and paravertebral venous plexuses.
There was no significant difference between both groups as regards the post operative complications; there were no cases of spinal cord or nerve root or vertebral artery injury in both groups. Dural tear occurred in 6.3% in group I and 3.3% in group II. Superficial wound infection occurred in 9.4% in group I and 6.7% in group II. Screw loosening and pullout occurred in 4 screws of 268 screws used in 4 different patients. Heller et al. Citation6 and Kast et al. Citation10 found in a series of patients operated for decompressive laminectomy with lateral mass fixation that the incidence of nerve root injury was 0.69%, screw loosening was 1.17%, infection was 1.3%, facet breakout was 0.2%, and 0% vertebral artery injury was very rare. Graham et al.Citation5 in a series of patients with lateral mass fixation reported 6.1% incidence of screw malposition and 1.8% incidence of radiculopathy per screw with no vertebral artery injury. TraynelisCitation20 found that decompressive laminectomy with lateral mass fixation results in successful arthrodesis in 98% of patients and less than 1% neurovascular injury.
Bony fusion was achieved in all the patients after 6 month follow up. Stability of the fixation was confirmed in postoperative X-ray in flexion and extension films in all the patients of group I. Swank et al.Citation18 found that the incidence of fusion with lateral mass fixation was 98%.
5 Conclusions
Lateral mass fixation of the cervical spine after multilevel cervical laminectomy is safe and reliable. It has undergone rapid evolution with many new techniques for fixation. It allows excellent decompressions of the cervical canal with few complications and also restores cervical lordosis with rigid fixation and prevents further kyphosis. It also improves neck pain and brachialgia.
Conflict of interest
The authors have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 11 October 2014
References
- M.M.Al BarbarawiZ.A.AudatM.M.ObeidatDecompressive cervical laminectomy and lateral mass screw-rod arthrodesis. Surgical analysis and outcomeScoliosis6201110
- A.M.AndrewR.A.PaulM.SameerAnatomic considerations for standard and modified techniques of cervical lateral mass screw placementSpine J22002430435
- W.L.DavidJ.L.ThomasR.PawanComparison of tension band wiring and lateral mass plating for subaxial posterior cervical fusionSurg Neurol501998323332
- J.A.EpsteinY.JaninR.CarrasA comparative study of the treatment of cervical spondylotic myeloradiculopathy: experience with 50 cases treated by means of extensive laminectomy, foraminotomy, and excision of osteophytes during the past 10 yearsActa Neurochir (Wien)61198289104
- A.W.GrahamM.L.SwankR.E.KinardPosterior cervical arthrodesis and stabilization with a lateral mass plate: clinical and computed tomographic evaluation of lateral mass screw placement and associated complicationsSpine J211996323329
- J.G.HellerH.SilcoxC.E.SutterlinComplications of posterior cervical platingSpine J20199524422448
- H.N.HerkowitzA comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for surgical management of multiple level spondylotic radiculopathySpine J131988774780
- B.JankowitzP.GerstzenDecompression for cervical myelopathySpine J62006317322
- W.Jau-ChingH.Wen-ChengC.Yu-ChunStabilization of subaxial cervical spines by lateral mass screw fixation with modified Magerl’s techniqueSurgical Neurol7020082533
- E.KastK.MohrH.P.RichterComplications of Transpedicular screw fixation in the cervical spineEur Spine J1532006327334
- V.G.KumarG.L.ReaL.J.MervisCervical spondylotic myelopathy: functional and radiographic long term outcome after laminectomy and posterior fusionNeurosurgery441999771777
- H.LiuA.PloumisJ.D.SchwenderPosterior cervical lateral mass screw fixation and fusion to treat pseudarthrosis of anterior cervical fusionJ Spinal Disord Tech2532012138141
- S.A.OlaroieD.G.ThomasSpinal cord compression due to prolapsed of cervical intervertebral discJ Neurosurg591983847853
- L.X.RenW.DuP.ZhangW.Y.DingEnlarged laminectomy and lateral mass fixation for multilevel cervical degenerative myelopathy associated with kyphosisSpine J14120145764
- R.Roy-CamilleG.SaillantC.MazelInternal fixation of the unstable cervical spine by a posterior osteosynthesis with plates and screwsH.H.SherkH.J.DunnF.J.EismontThe Cervical Spine2nd ed.1989J.B. Lippincott CompanyPhiladelphia, PA390403
- L.H.SekhonPosterior cervical decompression and fusion for circumferential spondylotic cervical stenosis: review of 50 consecutive casesJ Clin Neurosci13120062330
- L.SymonP.LavenderThe surgical treatment of cervical spondylotic myelopathyNeurology171967117127
- M.L.SwankC.E.SutterlinIIIC.R.BossonsRigid internal fixation with lateral mass plates in multilevel anterior and posterior reconstruction of the cervical spineSpine221997274282
- H.TakayamaH.MuratsuM.DoitaProprioceptive recovery of patients with cervical myelopathy after surgical decompressionSpine J30200510391044
- V.C.TraynelisAnterior and posterior plate stabilization of the cervical spineNeurosurgery19925976
- W.C.WattersR.LevinthalAnterior cervical discectomy with and without fusion: results, complications, and long term follow upSpine J1920199423432347
- R.XuS.P.HamanN.A.EbraheimThe anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and Ann techniquesSpine J2419199920572061
- Y.YukawaF.KatoH.YoshiharaCervical pedicle screw fixation in 100 cases of unstable cervical injuries: pedicle axis views obtained using fluoroscopyJ Neurosurg Spine J52006488493
