Abstract
The aim of this work is to evaluate the role of Doppler US and MRI in the diagnosis of placenta accreta.
Patients and methods
During period between 2012 to 2013, 120 pregnant patients with previous cesarean section were investigated by ultrasound and Doppler and then in suspected cases MRI was obtained (10 cases). The Sonographic and MRI diagnoses were compared with the final pathologic or operative findings or with both.
Results
The mean age of this study group was 29 years ranging from 20 to 40. Among patients with confirmed placenta accreta, the mean age was 32.25 ranging from 25 to 40 years. The mean parity of patients ranged from 1 to 6 with a mean of 1.6. Among patients with placenta accreta, the mean parity ranged from 2 to 6 with a mean of 3.75. The total number of cases with placenta accreta in this study was 4, all of which were previa. This was out of a total of 25 cases of placenta previa. Transabdominal US features were the presence of intraplacental lacunae (sonolucencies), loss of retroplacental clear zone and disruption of bladder–uterine serosa interface with smallest myometrial thickness <1 mm over site of placental implantation by using color Doppler ultrasonography, the most prominent color Doppler feature in this study was the presence of intraplacental lacunar flow. Magnetic resonance imaging accurately predicted placenta accreta in 4 of 4 cases with placenta accreta and correctly ruled out placenta accreta in the rest six cases.
Conclusion
In conclusion, data of the present study show that the use of transabdominal color Doppler ultrasonography complemented by MRI in suspected cases improves the diagnostic accuracy in prediction of placenta accreta in patients with previous cesarean delivery.
1 Introduction
Placenta accreta occurs when there is an abnormal adherence of a part or entire of the placenta to the uterine wall with either partial or complete absence of the decidua basalis. The placenta may be abnormally adherent to the myometrium, or extend to invade other tissues (uterine serosa or urinary bladder).Citation1 One of the catastrophic complications of PA is massive hemorrhage at the time of placental separation which can lead to renal failure, adult respiratory distress syndrome, and even death. In severe cases hysterectomy may be required, also urinary bladder or ureteral injury, pulmonary embolism are other serious complications.Citation2 Incidence of placenta accreta is markedly increased with the number of previous cesarean sections, the risk of placenta accreta increased with woman who had one cesarean section than with those with an unscarred uterus about 8 folds and then increased 4-fold with woman who had 2 or more cesarean sections.Citation3
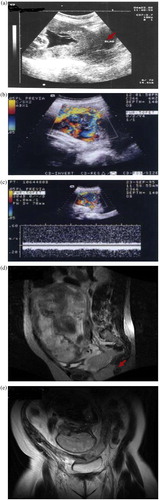
Case 1 Clinical history: a 25 year old female patient presented with vaginal bleeding with a history of four cesarean deliveries. US, color Doppler and MRI were performed and the diagnosis confirmed pathologically as placenta increta. US and color Doppler findings: (a) showing loss of retroplacental clear zone with SMT < 1 mm and placental bulge onto the bladder using grayscale U/S. (b) Using color Doppler an extensive hypervascularization pattern. (c) Pulsed Doppler interrogation of lacunae showing turbulent high-velocity (15 cm/s) venous-type flow, placental–bladder hypervascularization pattern was also observed. MRI findings: (d) sagittal T2 weighted image of the pelvis. The placental tissue is completely covering internal cervical OS with multiple irregular rounded hypointense areas. (e) Coronal T2 weighted MR image shows marked thinning of uterine wall seen at LT side of lower uterine segment with the invasion of placental tissue through uterine wall with still preservation of fat planes around bladder.
Case 2 Clinical history: a 38 year old female patient presented with pelvic pain and vaginal bleeding with a history of two cesarean deliveries. US, color Doppler and MRI were performed and placenta percreta was diagnosed and confirmed by pathology. US and color Doppler findings: (a, b) showing loss of retroplacental clear zone with SMT < 1 mm and placental bulge onto the bladder using grayscale U/S and using color Doppler, placental–bladder hypervascularization pattern was observed. (c) Coronal T2 weighted MR image of pelvis shows multiple tortuous signal voids seen in placenta representing hypervascularity. (d) Sagittal T2 weighted image shows the invasion of placental tissue to myometrium with the loss of tissue plane between placenta and bladder.
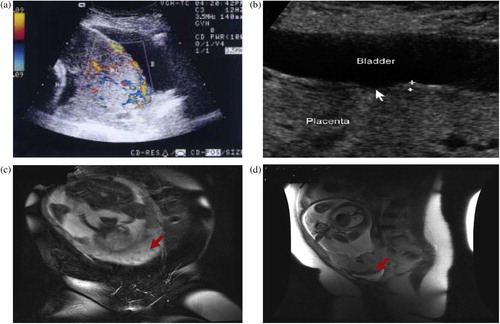
Case 3 Clinical history: a 31 year old female patient at 36 w of gestation presented with vaginal bleeding. US, color Doppler and MRI were performed and placenta increta was diagnosed. US, color Doppler findings: (a) sagittal trans abdominal US image showing placenta that completely covered the internal cervical os and bulging into urinary bladder and myometrial invasion was detected. MRI findings: (b) coronal T2 weighted images showing thinning of lower uterine segment with the invasion of whole myometrium with placenta tissue with abutting but no invasion into the bladder wall.
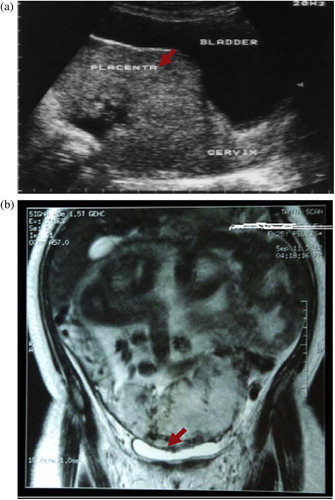
Table 4 MRI findings in selected ten cases.
Multiple sonographic findings are seen with placenta accrete such as decrease in myometrial thickness, placenta previa, placental lacunae, abnormal pattern of color Doppler, loss of the retroplacental clear zone and placenta percreta irregularities in wall of UB have been detected.Citation4 MR imaging is used in the diagnosis of placenta accreta when the sonographic findings are equivocal or when the placenta has a posterior location.Citation5 Many advantages are found for using MRI included excellent soft tissue contrast and non ionizing radiation in comparison with some limitations such as high cost, claustrophobia and limited availability.Citation6 The most MRI characteristic findings seen in placenta accrete are nodular thickening in the dark zone of placenta–uterine interface together with extensions of dark bands through the placenta, outer uterine bulge causing from the mass effect of the placenta and heterogeneous signal intensity of placenta on the T2-weighted HASTE sequences due to large placental lakes and vessels.Citation7 In spite of many studies having suggested the diagnostic accuracy of MRI in placenta accreta, some studies suggest that MRI is no more sensitive than ultrasound in the diagnosis of placenta accretaCitation8 The use of intravenous contrast enhancement (e.g. gadolinium) increases the specificity of MRI in the diagnosis of placenta accreta. Some still reluctant to use gadolinium because it crosses the placenta and is found in fetal tissues. However there are no reports of any side effects in human fetuses.Citation9
1.1 Aim of this study
Is to evaluate the role of using both ultrasound and MRI in the diagnosis of placenta accrete.
2 Patients and methods
In this study 120 pregnant women were referred from the Obstetric Department of Tanta University Hospital to the Department of Radio diagnosis to be investigated during the period from January 2012 to January 2013.
The patients included in the study were:
| • | Those have or gave history of third trimester bleeding. | ||||
| • | Those had repeated cesarean sections. | ||||
All cases were subjected to ultrasound and color Doppler examination.
Only 10 cases were suspected of having placenta accreta according to ultrasound and color Doppler findings in the Radio diagnosis department and all of them underwent MRI of the placenta. All ten cases had a history of multiple previous cesarean sections either with or without concomitant placenta previa. The indications for the MRI evaluation of the placenta in patients without placenta previa were posterior location of the placenta with a lack of good visualization of the placenta on ultrasound examination also anterior placenta with poor visualization of the scar of the cesarean section on ultrasound; partial or total loss of the retroplacental zone on ultrasound examination.
2.1 Ultrasound examination
Ultrasound examination was done in a high resolution B-mode with a Doppler flow imager apparatus (Siemens Acuson X300) using a transabdominal (3.5 MHz) curvilinear probe. Gray-scale B-mode trans abdominal ultrasound examination was first underwent to screen the placenta with careful examination for homogencity.
Ultrasound examination was preferred to undergo when the bladder was partially filled for optimal examination of the uterine serosa at the bladder wall interface. Measurement of the smallest myometrial thickness was obtained at the site of placental implantation.
All cases were subjected to transabdominal color Doppler evaluation where color signals were used to evaluate the variable uteroplacental vascular morphological patterns. With careful attention to the placental–myometrial interface and the placenta, in cases with placenta previa, we also evaluate the presence of abnormal intra placental lakes.
2.2 MRI examination
All cases underwent MRI examination in the radiodiagnosis department using a machine (GE signa 1.5 T) with an abdominal surface coil. All patients were positioned supine. The following sequences are used, axial, sagittal and coronal T2WI were taken. Axial cuts with fat saturated fast spin-echo T2WI and TIWI were obtained. Women were asked to follow Breath-holding techniques as possible as can be tolerated.
3 Results
The mean age among this study group was 29 years ranging from 20 to 40. While among patients with confirmed placenta accreta, the mean age was 32.25 ranging from 25 to 40 years. The mean parity of patients ranged from 1 to 6 with a mean of 1.6. Among patients with placenta accreta, the mean parity ranged from 2 to 6 with a mean of 3.75. The mean number of CS among the study group was 1.6 ranging from 1 to 5. The mean number of CS among patients confirmed to have placenta accreta: 2.75 ranged from 2 to 5.
Half of the cases with placenta accreta have 4 or 5 prior cesarean deliveries. No cases of placenta accreta were diagnosed among the 70 cases with prior 1 CS. So we found that the number of accreta cases increases in patients with increased number of previous CS. ().
Table 1 Distribution of accreta and non-accreta cases among previous cesarean sections according to the number of previous CS.
The total number of cases with placenta accreta in this study was 4, all of which were previa. This was out of a total of 25 cases of placenta previa. Placenta previa was classified into four grades, Grade I: low-lying placenta Grade II: marginal anterior, Grade III: partial placenta previa centralis and Grade IV: total placenta previa centralis. Placenta accrete was found in one case with partial placenta previa centralis and in three cases with total placenta previa centralis not found in placenta low lying or in placenta previa marginalis ().
Table 2 Distribution of accreta cases among previa cases.
3.1 Assessment of ultrasound feature in placenta accrete
| (1) | Loss of retro placental clear zone (RPZ): this was found to be statistically non significant in prediction of placenta accrete, only 50% of cases show loss of RPZ as the placenta villi invade the decidua basalis and penetrate the myometrium and the other two cases no loss of RPZ occurs due to presence of hypertrophied subplacental complex as compensating mechanism due to abnormal vascularity also idiopathic obliteration of RPZ occurs in normal cases this lead to decrease specificity. | ||||
| (2) | Intraplacental lacunae: intraplacental lacunae are seen in all cases of placenta accrete this was found to be statistically significant in predicting placenta accrete and color Doppler was done to differentiate whether the lakes were vascular or cystic spaces. | ||||
| (3) | Disruption of the bladder–uterine serosal interface: disruption of the bladder–uterine serosal interface was evident in all cases of placenta accrete, so it is statistically significant in predicting placenta accreta. | ||||
| (4) | Smallest myometrium thickness (SMT): over the site of placental implementation using the ultrasound, it was found that SMT < 1 mm was highly predictive of placenta accrete, this was statistically significant. Mean SMT among non accrete was 3.26 mm (range 2–6 mm). | ||||
| (5) | Sub placental venous complex: the presence of color flow in the subplacental venous plexus was found to be statically significant in predicting placenta accrete. | ||||
| (6) | Placental–bladder interface hyper vascularity: using color Doppler ultrasound revealed placental–bladder hyper vascularity as diagnostic significant in predicting placenta accrete (). | ||||
Table 3 Ultrasound and color Doppler findings in accreta cases.
3.2 Assessment of MRI feature in placenta accrete ()
Ten pregnant patients were referred for MRI studies to further evaluate the positive ultrasound study or when the ultrasound findings suggestive but not conclusive for placenta accrete.
MRI was a confirming tool for all cases suspected to have placenta accrete by US and Doppler study.
All of the patients with invasive placentas had myometrial thinning and indistinctness at the site of placental invasion, loss of retroplacental hypo echoic zone and uterine bulging in the lower segment.
Abnormal thick intraplacental dark band on T2, heterogenous signal intensity within the placenta and loss of myometrial interface were detected but not in all cases ().
4 Discussion
Placenta accreta is relatively rare but it is one of the life-threatening complications for pregnancy due to massive obstetric hemorrhage.Citation5 The incidence of placenta previa and placenta accreta was increased as regards to increase in the rate of cesarean sections.Citation10,Citation11
Incidence of placenta accreta in the presence of placenta previa increasing from 24% after one cesarean section to about 67% after four or more cesarean sections.Citation10
This agrees with our study which shows the mean number of C.S among patients confirmed to have placenta accreta: 2.75 ranged from 2 to 5. Half of the cases with placenta accreta have 4 or 5 prior cesarean deliveries. No cases of placenta accreta were diagnosed among the 70 cases with prior 1 CS. So we found that the number of accreta cases increases in patients with increased number of previous CS.
It is very important to obtain perfect diagnosis of placenta accreta prenatally, this gives optimal management planning to decrease morbidity.Citation12 Ultrasound examination with color Doppler imaging and MRI have all been used in the diagnosis of placenta accreta with varying specificity and sensitivity.
Ultrasound and color Doppler examination are the first-step for the diagnosis of placenta accreta. MRI is used as a complementary tool when ultrasound examination is equivocal or when the placenta hardly visualized on ultrasound examination.Citation13
In the current study, the uteroplacental vascular zone and the abnormal site of placenta were evaluated with the use of transabdominal ultrasound and color Doppler examination and MRI done for 10 cases and then results were correlated with the clinical outcome in patients with prior cesarean delivery.
In this study, the most common ultrasound features in predicting placenta accreta were the presence of a smallest myometrial thickness less than 1 mm, disruption of urinary bladder–uterine interface and the presence of multiple placental sonolucent area, which was present in all 4 confirmed accrete cases. This is in concordance with the study done by Twickler et al.Citation14 that reported that the presence of SMT < 1 mm or large intraplacental lucencies using color Doppler was present in all cases of myometrial invasion with 100% sensitivity, 72% specificity, both PPV and NPV were 72% and 100%, respectively.
This agrees also with a study done by Japaraj et al.Citation10 that reported the main ultrasound finding was the presence of multiple placental lakes which was seen in 6 out of 7 patients confirmed of having placenta accreta. However, myometrium thinning or focal disruption of uterine serosa was detected in only 4 out of 7 cases of placenta accreta.Citation5,Citation15
According to Japaraj et al.Citation10 ultrasound examination had 85% and 100% sensitivity and specificity, respectively in the diagnosis of placenta accreta.
In this study, thinning of myometrium less than 1 mm or disruption of uterine serosa showed 100% sensitivity and specificity. In all cases in which the uterine serosa–bladder interface was abnormal or interrupted, and confirmed to be placenta accreta. This agrees with ComstockCitation16 where interruption of bladder uterine interface showed 93% sensitivity and 84% specificity.
The most dominant color Doppler finding in the current study was the presence of intraplacental lacunar flow.
These results agree with Lerner et al.Citation17 who reported that the presence of color flow within intraplacental lacunae alone showed sensitivity 100% and 83% PPV in diagnosing placenta accreta and so he said that color Doppler results can be added to the intraplacental lacunae diagnosed by ultrasound to improve the accuracy of diagnosis.
In the current study we used MR imaging for ten patients and 4 of them were diagnosed as placenta accreta, in two cases hysterectomy was performed and in the other two bleeding was controlled and confirmed post operatively. We found that the addition of MR imaging to US increases the sensitivity to 100%.
MRI findings in the diagnosis of placenta accreta were included at first direct invasion of the placenta into the uterus which appears as thinning or indistinctness of the myometrium, loss of T2 dark uteroplacental interface or even direct visualization of the placental tissue either within or outside the myometrium.Citation18
Taipale et al.Citation8 recommended the use of color Doppler imaging when gray-scale ultrasound findings were typical of placenta accreta. In addition, they used MRI to complement ultrasonography.
Maldajian reported that the early MRI findings in the diagnosis of placenta accreta were the identification of direct invasion of the placenta into the uterus by direct visualization of placental tissue either within or outside the myometrium.Citation19
However, Lax et al.Citation20 described that three secondary signs detected in MRI in cases with placenta accreta included irregular thick T2 dark bands intraplacental, placental heterogeneity, and bulging seen at the lower uterine segment.
In another study, Teo et al.Citation21 reported that MRI findings seen in all patients diagnosis placenta accreta were three main MRI criteria described by Lax et al.Citation20
Both of the studies reported that there were no definite MRI criteria to accurately define the degree of invasion of placenta into the uterine wall. MRI is better than ultrasound in diagnosing patients with placenta accreta with 88% sensitivity and 100% specificity.Citation17
In this study MRI confirmed the diagnosis made by US but we cannot statistically evaluate the sensitivity and specificity of MRI due to small sample size but Warshak et al.Citation22 found in a study of 42 patients the MR imaging for PA shows sensitivity of 88% and specificity of 100%Citation20 on the other hand a retrospective study done by Garret lam et al. showed that the MRI sensitivity was 38% and US sensitivity was 33%.Citation4
Some authors reported that MR imaging is mostly indicated when there is a posterior location of placenta or when there were inconclusive US findings. MR imaging was a excellent tool for the detection of abnormal location of placenta, degree of myometrium invasion and hence the optimal surgical management and so it should be used routinely.Citation7
However there are several obstacles that limit the use of MRI especially in obstetrics such as fetal movements, unclear safety considerations for the fetus and its expenses.Citation23
It should be noted that the sensitivity of US with color Doppler examination increased in anterior placenta accreta while MRI was best in placenta accreta when the placenta posterior, because the placenta is hardly visualized by ultrasound.
5 Conclusion
Both gray scale ultrasound and color Doppler examination are highly accurate in predicting the radiological patterns of placenta accrete.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 19 October 2014
References
- G.KayemC.DavyConservative versus extirpative management in cases of placenta accretaObstet Gynecol1042004531536
- Baughman W.ChristopherE.Corteville JaneR.Shah RajivPlacenta accreta: Spectrum of US and MR Imaging Findings1Radiographics28200819051916
- R.M.SilverThe MFMU Cesarean Section Registry: maternal morbidity associated with multiple repeat cesarean deliveryAm J Obstet Gynecol1912004S17
- G.LamUse of magnetic resonance imaging and ultrasound in the antenatal diagnosis of placenta accretaJ Soc Gynecol Invest920023740
- D.LevineC.A.HulkaJ.LudmirW.LiR.R.EdelmanPlacenta accreta: evaluation with color Doppler US, power Doppler US and MR imagingRadiology2051997773776
- F.G.ShellockJ.V.CruesMRI procedures: biologic effects, safety and patient careRadiology2322004635
- Y.OyeleseJ.C.SmulianPlacenta previa, placenta accreta and vasa previaObstet Gynecol1072006927941
- P.TaipaleM.R.OrdenM.BergH.Manninen AlafuzofflPrenatal diagnosis of placenta accreta and percreta with ultrasonography, color Doppler, and magnetic resonance imagingObstet Gynecol10432004537540
- R.D.KokM.M.de VariesA.HeerschapAbsence of harmful effects of magnetic resonance exposure at 1.5 T in utero during the third trimester of pregnancy: a follow up studyMagn Reson Imaging222004851854
- R.P.JaparajT.S.MiminK.MakudanAntenatal diagnosis of placenta previa accreta in patients with previous cesarean scarJ Obstet Gynecol3342007431437
- D.A.MillerJ.A.CholletT.M.GoodwinClinical risk factors for placenta previa–placenta accretaAm J Obstet Gynecol1771997210214
- C.G.ZorluC.TuranA.Z.IsikN.DanismanT.MunganO.GokmenEmergency hysterectomy in modern obstetric practiceActa Obstet Gynecol Scand771998186190
- C.H.ComstockAntenatal diagnosis of placenta accreta: a reviewUltrasound Obstet Gynecol2620058996
- D.M.TwicklerM.J.LucasA.B.BalisR.Santos-RamosL.MartinS.MaloneColor flow mapping for myometrial invasion in women with a prior cesarean deliveryJ Matern Fetal Med92000330335
- H.J.FinbergJ.W.WilliamsPlacenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean sectionJ Ultrasound Med111992333343
- C.H.ComstockJ.J.LoveJ.R.R.A.BronsteenW.LeeI.M.VettrainoR.R.HuangSonographic detection of placenta accreta in the second and third trimesters of pregnancyAm J Obstet Gynecol190200411351140
- J.P.LernerS.DeaneI.E.Timor-TritschCharacterization of placenta accreta using transvaginal sonography and color Doppler imagingUltrasound Obstet Gynecol51995198201
- V.A.CatanzariteL.M.StancoD.R.SchrimmerC.ConroyManaging placenta previa/accretaContemp Obstet Gynecol4119966695
- C.MaldjianR.AdamM.PelosiMRI appearance of placenta percreta and placenta accretaMagn Reson Imaging171999965971
- A.LaxM.R.PrinceK.W.MennittJ.R.SchwebachN.E.BudorickThe value of specific MRI features in the evaluation of suspected placental invasionMagn Reson Imaging2520078793
- T.H.TeoY.M.LawK.H.TayB.S.TanF.K.CheahUse of magnetic resonance imaging in evaluation placental invasionClin Radiol642009511516
- Warshak CR, Eskander R, Hull AD, Scioscia AL, Mattre RF, Benirschke K, et al. Diagnosis of placenta accreta. Obstet Gynecol 2006;108(3):573–81.
- M.M.ChouJ.J.TsengJ.I.HwangE.S.C.HoY.H.LeeSonographic appearance of tornado blood flow in placenta previa accreta/incretaUltrasound Obstet Gynecol172001362363
