Abstract
Background
Electrolyte disturbances have been reported in both tuberculosis (TB) infection alone and TB-HIV co-infected patients.
Objectives
To evaluate the effects of treatments on the imbalance of some electrolytes among patients infected with Mycobacterium tuberculosis in Osogbo Southwestern Nigeria.
Methodology
A total of one hundred and ten patients participated in this study. They were divided into four groups as follows: group 1 contains 50 normal patients without TB or HIV infection (M = 25; F = 25), group 2 20 new positive cases of TB patients without HIV infection (M = 13; F = 07), group 3 20 new positive cases of tuberculosis co-infected with HIV infection (M = 10; F = 10), and group 4 20 positive cases of TB patients on anti tuberculous drugs (M = 11; F = 09). All patients were screened for the presence and absence of TB, HIV and the level of some electrolytes in plasma (sodium, potassium, chloride and bicarbonates) were determined using standard methods.
Results
Levels of sodium in TB patients on drugs (TBD) were significantly lowered compared to new case tuberculosis (NCT) patients (134.80 ± 5.83 mmol/L vs 142.10 ± 6.68 mmol/L) while potassium levels were significantly elevated in TB patients on drugs compared with their new case counterparts (3.75 ± 0.15 mmol/L vs 3.07 ± 0.42 mmol/L) P < 0.05 respectively. Chloride levels were significantly decreased in TB patients on treatment compared to new case tuberculosis NCT (99.26 ± 6.85 mmol/L vs 108.76 ± 8.42 mmol/L) while serum bicarbonate levels were significantly elevated in TB patients on drug (TBD) compared to their NCT counterparts (24.00 ± 1.81 mmol/L vs 21.00 ± 2.05 mmol/L, P < 0.05, respectively).
Conclusion
Hyponatraemia, hyperkalaemia, and hypochloremia characterized some of the electrolyte imbalance among TB patients receiving treatments. The raised level of bicarbonate may be attributed to overcorrection of respiratory acidosis often found in patients with tuberculosis. Monitoring electrolytes is therefore an important component of TB management.
1 Introduction
Tuberculosis is a major cause of morbidity, disability and death.Citation1 It accounts for 2–3 million deaths per annum, globally.Citation1,Citation2 One third of the World population has been exposed to the TB bacterium, and new infections occur at a rate of one per second.Citation3 In 2006, a total of 1.7 million people died of TB including 231,000 people with HIV.Citation3 Nigeria has the fourth highest burden of Tuberculosis (TB) in the world, with an annual incidence of 311 cases per 100,000 population and a mortality rate of 81 per 100,000 population in 2006.Citation4 In Nigeria, about 21% of all TB patients are dually infected with TB and HIV.Citation4,Citation5
Factors contributing to the resurgence of tuberculosis in developing countries include co-infection with HIV; emergence of multiple resistant tuberculosis, inadequate treatment, poverty, malnutrition, overcrowding, armed conflict and increasing numbers of displaced persons. diarrhea, vomiting, and excessive sweating, are common features of HIV/AIDS and Tuberculosis infections and have been described as possible cause of loss of water and electrolyte. However, reports showed that the frequency and nature of renal and electrolyte abnormalities in HIV patients vary considerably from centre to centre.Citation6 Fluid-electrolyte and acid-base derangements frequently encountered in AIDS and TB, have been found to be major factors for the development of acute renal failure.Citation7
In view of this associated water and electrolyte derangement and associated cytochemical changes in Tuberculosis and HIV infections, this study was designed to determine the effect of treatment on common electrolytes and free radical status in patients with tuberculosis and those with co-infection with HIV. Comparing electrolyte values in controls with pulmonary tuberculosis patients not on treatment, comparing electrolyte values in controls with pulmonary tuberculosis patients on treatment, and electrolyte in pulmonary tuberculosis patient on treatment with those not on treatment could all contribute to the body of knowledge on electrolyte disturbances associated with these diseases. The overall objectives of this study are to evaluate the effects of treatments on the imbalance of some electrolytes among patients infected with Mycobacterium tuberculosis in Osogbo Southwestern Nigeria
2 Methods
2.1 Study location
The study location was Osogbo, the capital city of Osun State. With a population of about half a million, HIV prevalence of 25% was reported among TB positive in 2010, though HIV prevalence in the state was a bit lower than the national average of 4.1.Citation8 There are numerous health facilities providing care at different levels of health care. There are two non governmental organizations whose presence could be felt in the areas of HIV and TB in the city.
2.2 Study design
Descriptive cross sectional study among various categories of TB infected patients.
2.3 Study population
Include 4 categories of patients, recruited from four TB management centres in Osogbo. The categories are
| (a) | Group 1: 50 normal patients without TB or HIV in the sex ratio of 1:1. | ||||
| (b) | Group 2: 20 new positive cases of M. tuberculosis patients without HIV in the ratio of M:F of 2:1. | ||||
| (c) | Group 3: 20 new positive cases of tuberculosis co-infected with HIV in a sex ratio of 1:1. | ||||
| (d) | Group 4: 20 positive cases of M. tuberculosis patients on anti tuberculous drugs with 11 males and 09 females. | ||||
2.4 Exclusion criteria
Patients with symptoms of malaria fever, Diabetes Mellitus, severe malnutrition, patients with intestinal infection which could lead to dysentery, women using contraceptives, patients on corticosteroid therapy, pregnant women and patients with symptoms of jaundice were excluded from this study.
2.5 Ethical approval
The study received approval of the ethics review committee of LAUTECH Teaching Hospital Osogbo. Written informed consent was obtained from each subject after the study has been explained to them.
2.6 Sampling procedure
Two Primary Health Care (PHC) centers were randomly selected from the list of primary health facilities to complement the tertiary and secondary level facilities in Osogbo. These evolved Sabo Primary Health Centre, Oke-Baale Primary Health Centre, General hospital Asubiaro and Ladoke Akintola University of Technology Teaching Hospital, Osogbo. A total of one hundred and ten patients were serially recruited to participate in this study. Every new case was screened for M. tuberculosis (in their sputum using Ziehl-Neelsen modified technique). The presence or absence of HIV in their blood was carried out using the National algorithm for the diagnosis of HIV (Determine-Unigold-Start-pack Kits). Fifty (50) controls for this study were recruited among volunteers who were on routine medical check-up at the teaching hospital. These were matched for age with the cases. They were also screened for HIV and pulmonary TB and confirmed negative.
2.7 Treatments
After their tuberculosis was diagnosed, patients were commenced on Anti TB drugs of DOTS (Directly Observed Treatment– Short course) according to National guidelines on treatment of TB, and TB and HIV co-infection.Citation9 All cases were managed by the attending TB officer while TB-HIV co-infected patients attend both TB and ART (antiretroviral therapy) clinics. AntiTB drugs were administered by the health care workers in the facility.
2.8 Blood and sputum sample collection
Five to seven millimeters of venous blood was obtained from the cubital vein of each patient using a sterile needle and syringe into a lithium heparin bottle. The plasma was extracted by centrifugation for 10 min at 4000 rpm into a plain bottle and stored at −20 °C until the time of analysis for electrolytes and free radicals. The sputum of patients (except those on anti-tuberculosis drugs) and controls were collected into a sterile universal bottle for Ziehl-Neelsen staining.
3 Biochemical analysis
Estimation of sodium and potassium using Flame emission spectrophotometry method. Atom of metals in the hot flame gained sufficient energy thereby making a specific amount of quantum of thermal energy to be absorbed by an orbital electron. The electrons being unstable in this high energy (excited) state release their excess energy as photons at a particular wavelength as they change from excited state to their previous or ground state.Citation10
Estimation of chloride using colorimetric: TPTZ [mercury(II)-2,4,6-tri-(2-pyridyl)-s-triazine] method. This was based on the principle that Chloride ions react with a mercury(II)-2,4,6-tri-(2-pyridyl)-s-triazine (TPTZ) complex to form mercury(II) Chloride. The librated TPTZ react with Iron (II) ions yielding a blue coloured complex. The resulting absorbance change at 590 nm is directly proportional to the amount of chloride ion in the sample.Citation11
Estimation of bicarbonate using back titration method. This was based on the principle that: When a known volume of a standard HCl is added to HCO3 present in the plasma, there will be a reaction between HCl and HCO3 resulting in the production of carbon dioxide gas. The excess HCl that is not used up is back titrated with a standard solution of NaOH to an end point. The reaction mixture must be thoroughly shaken.Citation12
4 Results
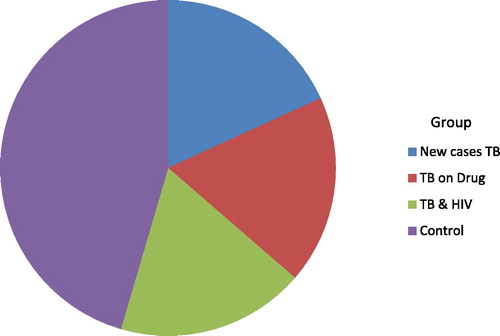
is a pie chart showing the frequency and percentage distribution of the study population. The test group comprises three (3) sub-groups; first group are the new cases and made up of 20 patients (18.18% of the total population) who are not on drugs. The second group are those on drugs for 5–6 weeks and also made up of 20 patients (18.18% of the total population) while the third group are those having co-infection with HIV. They are also made up 20 patients and not on drugs (18.18% of the total population). The control groups are 50 patients (45.45% of the total population).
4.1 Physical parameters
In , the mean age and mean height for all the patients was not significantly different from those of the control patients. There was a significant decrease in weight (in kilograms) when TB-co-infection with HIV patients was compared with new cases of Tuberculosis and TB patients on drugs (43.83 ± 7.58 vs 52.78 ± 15.10, 50.75 ± 12.47; P < 0.05). There was no significant difference in the weight when new cases of tuberculosis were compared with TB patients on drugs (P > 0.05).
Table 1 Comparing parameters in Control patients with cases (TB new cases, TB cases on drug, TB cases co-infection with HIV).
4.2 Biochemical parameters
In , the sodium value was significantly lower in controls when compared with the total subject population, new case TB patients and TB co-infection with HIV patients (135.46 ± 4.00 vs 139.15 ± 7.50 vs 142.10 ± 6.68, 140.55 ± 8.07) mmol/L There was a significant increase in mean sodium value when TB co-infection with HIV patients were compared with TB patients on drugs (140.55 ± 8.07 vs 134.80 ± 5.83 mmol/L; P < 0.05), .
Potassium value was significantly lower in controls when compared with total subject population, TB patients on drugs and TB co-infection with HIV subject (3.17 ± 0.31 vs 3.50 ± 0.48, 3.75 ± 0.15, 3.66 ± 0.42 mmol/L; P < 0.05). However, there was a significant decrease in potassium value of new case TB patients when compared with control (3.07 ± 0.42 vs 3.17 ± 0.31 mmol/L; P < 0.05).
Similarly, there was a significant decrease in mean potassium value when new case TB patients were compared with TB patients on drugs and TB co-infection with HIV (3.07 ± 0.42 vs 3.75 ± 0.15, 3.66 ± 0.42 mmol/L; P < 0.05). There was no significant difference between TB patients on drug and TB co-infection with HIV (3.75 ± 0.15 vs 3.66 ± 0.42) mmol/L.
There was no significant difference observed between the total subject population and control (104.27 ± 8.56 vs 101.52 ± 4.40) mmol/L. There was a significantly higher mean value of chloride in new case of TB patients when compared with control (108.76 ± 8.42 vs 101.52 ± 4.40 mmol/L; P < 0.05) as well as highly significant mean value of chloride in control when compared with TB patients on drugs (101.52 ± 4.40 vs 99.26 ± 6.85 mmol/L; P < 0.05).
However, the mean value of chloride was significantly higher in new case TB patients when compared with TB patients on drug and TB co-infection with HIV (108.76 ± 8.42 vs 99.26 ± 6.85, 104.81 ± 8.08 mmol/L; P < 0.05). The mean chloride value was also significantly higher in TB co-infection with HIV when compared with TB patients on drugs (104.81 ± 8.08 vs 99.26 ± 6.8) mmol/L; P < 0.05).
However, there was no significance difference in mean bicarbonate value when new case TB patients were compared with controls (21.00 ± 2.05 vs 21.64 ± 1.47 mmol/L; P < 0.05). The mean value of bicarbonate was significantly lower in control when compared with total patient population, TB patients on drug, TB co-infection with HIV patients (21.64 ± 1.47 vs 23.13 ± 2.40, 24.00 ± 1.81, 24.40 ± 1.64 mmol/L; P < 0.05). Also, the mean value of bicarbonate was significantly lower in new case TB patients when compared with TB patients on drug and TB co-infection with HIV (21.00 ± 2.05 vs 24.40 ± 1.64 mmol/L; P < 0.05). Meanwhile, there was no significant difference between TB patients on drugs and TB co-infection with HIV (24.00 ± 1.81 vs 24.40 ± 1.64) mmol/L.
In , the patients on drugs show a positive correlation between height and weight (r = 0.828, P < 0.01), sodium and chloride (r = 0.970, P < 0.01) while an inverse correlation was observed between sodium and bicarbonate (r = 0.690, P < 0.01), chloride and bicarbonate (r = 0.803, P < 0.01). In , which shows Pearson’s correlation of TB patients co-infection with HIV a positive correlation was observed between sodium and chloride (r = 0.979, P < 0.01), while an inverse correlation was observed between height and bicarbonate (r = 0.519, P < 0.05), potassium and chloride (r = 0.763, P < 0.01), potassium and sodium (r = 0.793, P < 0.01) and potassium and free radicals (r = 0.478, P < 0.05).
Table 2 Pearson’s correlation table of tuberculosis patients on drugs.
Table 3 Pearson’s correlation table of tuberculosis co-infection with HIV patients.
5 Discussion
The mean lower level of sodium Na+ found in TB co infections with HIV patients than the new cases pulmonary tuberculosis patients, is consistent with another study.Citation13 This can be attributed to the loss of Na+ through diarrhoea presented by most of AIDs infected patients.Citation13,Citation14 At the same time, decreased Na+ observed in patients on drug than control patients, and those patients on drugs than new cases pulmonary TB patients, and TB co infections with HIV patients could be due to the fact, that loss of water and salt leads to dehydration.Citation14 These are consistent with findings from this study in which 14 (70%) of patients taking drug experience vomiting. This is one of the major adverse reactions of some antiTB drugs especially Pyrazinamide.Citation15
The observed significant higher mean values of Sodium Na+ level in the total patients than in control may be attributable to dehydration due to vomiting, muscle wasting, fever and because sweat is hypotonic compared with plasma.Citation16 The same reason for the above can also hold for higher significant values of Na+ in new case tuberculosis patients, TB Co infection with HIV when compared with controls.
It was found that the mean K+ level in patients with TB co infections with HIV patients was significantly higher than those of the new cases pulmonary tuberculosis patients and the control patients. The above observation can be attributed to the facts that in HIV/AIDS infection, there is the killing of cells by virus, high grade pyrexia/fever (causing the destruction of cells) and therefore leading to the influx of K+ from the cells to the plasma.Citation17 The mean K+ value of patients on drug was significantly higher compared to other patient groups and control; this may be due to non compliance in prescription of drug therapy. Inappropriate administration of Rifampicin (less often than twice weekly) may cause a flu like syndrome characterized by fever and anaemia leading to hyperkalamia.Citation18
In this study, the level of K+ was significantly lower in pulmonary tuberculosis patients when compared to the normal patients. This agreed with another study.Citation19 In the stress situation due to severe/chronic illness there is increased catabolism of protein leading to the movement of K+ from the intercellular compartment to the plasma and consequently excreted in the urine, sweat and vomitus without any compensatory replacement through food due to anorexia a common feature of pulmonary tuberculosis.Citation20
The mean value of chloride gave the same pattern as the level of Na+ in the patients because Na+ is always (in most cases) in association with Cl−, therefore the same reason for the level of Na+ in the patients also holds for this. The lower significant bicarbonate level in the pulmonary tuberculosis patients than the TB co infections and the normal patients can be attributed to the body’s compensatory mechanism to maintain electrochemical neutrality due to the plasma levels of Na+ and especially chloride.Citation16 The significantly higher level of free radicals found in new case pulmonary tuberculosis patients, TB co-infection with HIV can be attributed to the facts that mycobacterium induces Reactive Oxygen Species (ROS) and nitrogen intermediates (RNI) by activating phagocytes,Citation21 there by promoting tissue injury and inflammation. This further contributes to immune-suppression,Citation22 in HIV infected patientsCitation23,Citation24 with consequent production of ROS and RNI in larger amounts.Citation22 The inability of this study to do a PCR or culture to differentiate between typical and atypical Mycobacteria due to resource constraints could be regarded as a limitation to this study. This could have given a differential diagnosis with the likelihood of presenting with similar symptoms. This is however not a main focus of this research.
6 Conclusion
This study suggests that the institution of treatment on TB patients seems to bring about the development of hyponatraemia, hyperkalaemia, hypochloraemia and hypercarbonaemia. The raised level of bicarbonate may be attributed to overcorrection of increased partial pressure of carbon dioxide (i.e., respiratory acidosis) often found in patients with tuberculosis. Electrolyte and acid-base balance monitoring in patients with tuberculosis is recommended once treatment is recommenced.
Funding
This study received no external funding. Authors contributed personal resources to fund the research work.
Conflict of interest
None exists among authors or institutions involved in this study.
Contribution of authors
The first two authors conceived the research idea and were involved in planning, research designs, methods and data collection and analysis and write up. The third author was involved in methods, data collection and write up. The 4th author was actively involved in data collection, analysis and discussions.
Acknowledgements
The authors are grateful to the Medical Directors of participating hospitals, TB programmes Director, the laboratory Departments of LAUTECH College of Health Sciences as well as all patients who participated in the study.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 24 February 2015
References
- H.TomiokaK.NambaDevelopment of antituberculous drugs: current status and future prospectsKekkaku81122006753774
- R.G.DucatiA.Ruffino-NettoL.A.BassoD.S.SantosThe resumption of consumption – a review on tuberculosisMem Inst Oswaldo Cruz10172006697714
- World Health Organization WHO. Tuberculosis Fact sheet N°104-Global and regional incidence. 2006, Retrieved on 6 October 2006.
- World Health Organization. WHO Report Global TB control: Nigeria. In: WHO, editor. Geneva, Switzerland: WHO; 2008. Available from: http://www.who.int/globalatlas/predefinedReports/TB/PDF_Files/nga.pdf [accessed 2013 December].
- L.LawsonM.A.YassinT.D.ThacherO.O.OlatunjiJ.O.LawsonT.I.AkingbogunClinical presentation of adults with pulmonary tuberculosis with and without HIV infection in NigeriaScand J Infect Dis10200716
- V.A.OnwuliriTotal bilirubin, albumin, electrolytes and anion gap in HIV positive patients in NigeriaJ Med Sci432004214220
- R.BerggrenV.BatumanHIV-associated renal disorders: recent insights into pathogenesis and treatmentCurr HIV/AIDS Rep22005109115
- National Agency for the Control of HIV/AIDS NACA. Prevalence of HIV among Tuberculosis and HIV co-infected clients. NACA Nigeria 2010.
- Federal Ministry of Health, Nigeria FMOH. National HIV/Syphilis Sero-prevalence Sentinel Survey Among Pregnant Women Attending Antenatal Clinics, 2005. Abuja, Nigeria: National HIV Sero-prevalence Sentinel Survey (Technical Report), Federal Ministry of Health, Nigeria; 2006.
- C.J.BhagatP.Garcia-WebbE.FletcherJ.P.BeilbyCalculated vs measured plasma osmolalities revisitedClin Chem3010198417031705
- L.T.SkeggsH.C.HochstrasserThiocyanate (colorinmetric) method of chloride estimationClin Chem101964918920
- S.VanFlitration method and urea estimationJ Biol Chem521922495497
- T.KaileI.ZuluR.LumayiN.AshmanP.KellyInappropriately low aldosterone concentrations in adults with AIDS-related diarrhoea in Zambia: a study of response to fluid challengeBMC Res Notes1200810
- U.SiddiquiE.J.BiniK.ChandaranaPrevalence and impact of diarrhea on health-related quality of life in HIV-infected patients in the era of highly active antiretroviral therapyJ Clin Gastroenterol412007484
- Hong Kong Chest Service/British Medical Research CouncilAcceptability, compliance, and adverse reactions when isoniazid, rifampin, and pyrazinamide are given as a combined formulation or separately during three-times-weekly antituberculosis chemotherapyAm Rev Respir Dis.1406198916181622
- Baron DN, Whicher JT, Lee KE. A new short textbook of chemical pathology. ELBS fifth edition printed and bound in Great Britain by Bulter and Tanner Ltd., Frome and London, 2009; 17–32.
- Macleod J. David son’s principle and practice of medicine, price Thirteenth Edition Publisher by ELBS and Churchill Livingstone, 1981, 307.
- O.W.MwandaHaematological changes in HIV infectionEast Afr Med J742007732736
- Mayne PD. Clinical chemistry in diagnosis, 6th ed., Oxford Scientific Publications, London, 1994; 267–270.
- Cheebrough M. District Laboratory Practice in Tropical Countries Part 2, Cambridge Low Price Editions, Cambridge University Press, 2000: 207–212 and 253–266.
- Y.N.ReddyS.V.MurthyD.R.KrishnaM.C.PrabhakarRole of free radicals and antioxidants in TB patientsIndian J Tuberc512004213218
- E.H.CemT.R.YusufMustafaCekmenSerum levels of TNF-a, sIL-2R, IL-6, and IL-8 are increased and associated with elevated lipid peroxidation in patients with Behçet’s diseaseMediators Inflammation1120028793
- R.van CrevelT.H.OttenhoffJ.W.van der MeerInnate immunity to Mycobacterium tuberculosisClin Microbiol Rev152002294309
- F.MullerA.M.SvardalI.NordoyR.K.BergeP.AukrustS.S.FrolandVirological and immunological effects of antioxidant treatment in patients with HIV infectionEur J Clin Invest302000905914