Abstract
Aim
To clarify the value of dobutamine stress tissue Doppler in the evaluation of LV functional improvement after elective PCI.
Methods
The study included 60 patients with hibernating viable myocardium proved by DSE referred for an evaluation of myocardial viability prior to revascularization. Hemodynamic and echocardiographic variables (LVEF, WMSI and TDI Sm) were assessed at rest and during stress. 1 month after PCI follow up echocardiography and TDI were done. Patients were divided into 2 groups: (Group I): 18 patients (30%) with no global functional recovery and (Group II): 42 patients (70%) with global functional recovery.
Results
SBP, DPB, HR, EF, WMSI and (Sm) increased significantly at stress P = 0.001. After 1 month patients were divided into 2 groups according to functional recovery. There were no statistically significant differences between two groups neither as regards age, sex, risk factors (P > 0.05) nor as regards SBP, DBP, HR, rate/pressure product, EF and WMSI during stress but Sm increased during stress and after1 month follow up in Group II (P = 0.001). Univariate regression showed that (Sm) is the only predictor for global functional recovery. ROC curve statistical analysis shows that (Sm) is more sensitive and accurate than (WMSI) in the detection of viable myocardium which predicts improvement after revascularization (sensitivity 100%, 50% and accuracy 93.3%, 83.3% respectively).
Conclusion
Stress TDI provides a feasible and quantitative technique that improves reproducibility of DSE. Sm during stress showed better accuracy than WMSI for the prediction of functional recovery following revascularization and was simple, sensitive and accurate for the detection of subtle myocardial systolic velocity changes.
Abbreviations:
- ACS
- acute coronary syndrome
- CAD
- coronary artery disease
- DBP
- diastolic blood pressure
- DM
- diabetes mellitus
- DSE
- dobutamine stress echo
- HR
- heart rate
- IHD
- ischemic heart disease
- LDDSE
- low dose dobutamine stress echo
- LV
- left ventricle
- LVEF
- left ventricular ejection fraction
- NVP
- negative predictive value
- PCI
- percutaneous coronary intervention
- PPV
- positive predictive value
- SBP
- systolic blood pressure
- TDI
- tissue Doppler image
- WMSI
- wall motion score index
1 Introduction
Coronary artery disease (CAD) remains a principal cause of morbidity and mortality worldwide. Many subjects with coronary artery disease have viable but dysfunctional myocardium, where a kinetic or severely hypokinetic myocardium keeps the ability to contract if perfusion improves.Citation1
Dobutamine stress echocardiography (DSE) and myocardial perfusion imaging are commonly used to detect viable but dysfunctional myocardium. In studies that evaluated the improvement of function on the segmental basis, SPECT and PET demonstrate excellent sensitivity, whereas echocardiography with dobutamine stress has superior specificity and positive predictive value.Citation2
Tissue Doppler imaging (TDI) is evolving as a useful echocardiographic tool for quantitative assessment of left ventricular (LV) systolic and diastolic function.Citation3
Systolic tissue velocity imaging and post systolic shortening during acute coronary occlusion were correlated to the recovery of LV systolic function measured early and late after reperfusion. These results suggested that tissue velocity imaging may be related to an active process reflecting myocardial viability.Citation4
Several studies demonstrated the potential role of tissue Doppler imaging during dobutamine stress echocardiography to quantify myocardial velocity and deformation, instead of or in addition to traditional evaluation of the wall motion score index (WMSI).Citation5 However, its application during stress echocardiography remains controversial since no clear advantage in terms of both test interpretation and objective quantification has been demonstrated.Citation6 Other studies concerning TDI proved its diagnostic value for the detection of myocardial viability during DSE and subsequent recovery after successful revascularization.Citation7
2 Aim of the work
The aim of the work was to clarify the value of dobutamine stress tissue Doppler in the evaluation of LV functional improvement after elective PCI.
3 Patients and methods
This study included 60 patients with IHD who were referred to the Benha university hospital, Cardiology department for evaluation of viability prior to revascularization during the period from March 2012 to March 2014.
Exclusion criteria:
| • | Recent myocardial infarction or ACS. | ||||
| • | AF or any Ventricular arrhythmias. | ||||
| • | Previous pace maker implantation. | ||||
| • | Dilated cardiomyopathy. | ||||
| • | RHD. | ||||
| • | Prosthetic valve disease. | ||||
| • | Complicated PCI. | ||||
| • | LVEF less than 45%. | ||||
| • | Patients whose viability studies showed no significant viable myocardium or scar tissue. | ||||
Patients will undergo the following:
| 1) | Detailed history – Age, sex, typical ischemic symptoms and presence of risk factors (DM, HTN, smoking, dyslipidemia and positive FH of IHD). | ||||
| 2) | Thorough physical examination – for assessment of the severity of IHD or HF symptoms (clinically S3 gallop, mitral regurge murmur or bilateral fine basal crepitation). | ||||
| 3) | Laboratory routine investigations – Complete blood count, random blood sugar, liver function test, kidney function test and coagulation profile. | ||||
| 4) | ECG. | ||||
| 5) | Echocardiography. | ||||
3.1 The conventional echocardiography study
Patients were imaged in the left lateral decubitus position using a commercially available system (Vivid 7, General Electric Vingmed). Images were obtained with simultaneous ECG-signals.
3.1.1 2D echo
Images were acquired during breath hold and saved in cine-loop format, from the three 2 consecutive beats. The biplane Simpson’s technique was used to calculate LV end systolic volumes (LVESVs), LV end diastolic volumes (LVEDVs) and LVEF.
3.1.2 M-mode echo
Measurement of LV dimensions in systole and diastole (LVIDs, LVIDd), interventricular septum (IVSd, IVSs), posterior wall thickening (PWTd) and LVEF% was carried out.
3.1.3 Pulsed wave Doppler echo
Pulsed-wave Doppler of the mitral valve was obtained by placing the Doppler sample volume between the tips of the mitral leaflets. The early (E) and late (A) peak diastolic velocities and E-wave deceleration time were measured.
3.2 Dobutamine stress echocardiography
The patients abstain from all oral intake for at least 3 h before the procedure. B-blockers were withheld 48 h before the testing. Dobutamine was administered intravenously by an infusion pump at a starting dose of 10 μg/kg/min. At least at 3 min intervals, the dosage was increased to 20 μg/kg/min. Throughout the dobutamine infusion, the ECG was continuously monitored and recorded at 1 min interval and blood pressure was recorded every 3 min.Citation8
End points of interruption of the test:
| (1) | Extensive new wall motion abnormalities. | ||||
| (2) | Severe angina. | ||||
| (3) | Symptomatic reduction in systolic blood pressure (SBP) >40 mmHg from the baseline (See ). | ||||
| (4) | Severe hypertension (BP > 240/120 mmHg). | ||||
| (5) | Significant arrhythmias. | ||||
| (6) | Any serious side effects regarded as being due to dobutamine infusion. | ||||
| (7) | Upon patient request.Citation9 | ||||
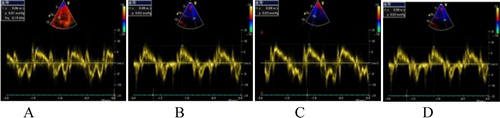
Figure 1 Average pulsed wave TD (Sm) of the patient at baseline about 7 cm/s. (A) Pulsed TD (Sm) at the level of basal septum 6 cm/s, (B) Pulsed TD (Sm) at the level of basal anterior about 8 cm/s, (C) Pulsed TD (Sm) at the level of basal inferior about 6 cm/s, (D) Pulsed TD (Sm) at the level of basal lateral about 8 cm/s.
The echocardiographic images are digitized and displayed side-by-side in quad screen format to facilitate the comparison of images. Wall motion is evaluated visually, using both endocardial motion and systolic wall thickening (See ).
| (a) | According to the American Society of Echocardiography, in a 16-segment model or optionally 17-segment model with an addition of the apical cap, the following numerical score is assigned to each wall segment on the basis of its contractility as assessed visually. | ||||
| (b) | Wall motion score index (WMSI): The American Society of Echocardiography has recommended a 16-segment model. This model consists of six segments at both the basal and mid-ventricular levels and four segments at the apex. The attachment of the right ventricular wall to the left ventricle defines the septum, which is divided at basal and mid-left ventricular levels into antero-septum and infero-septum. Continuing counterclockwise, the remaining segments at both basal and mid-ventricular levels are labeled as inferior, infero-lateral, antero-lateral and anterior. The apex includes septal, inferior, lateral and anterior segments. Each segment was analyzed and scored on the basis of its motion and systolic thickening. Segments were scored as normal (>40% thickening with systole) = 1, hypokinesis (10–30% thickening) = 2, akinesis (<10% thickening) = 3, dyskinesis = 4 and aneurysmatic = 5. WMSI was derived as the sum of all scores divided by the number of segments visualized.Citation10 | ||||
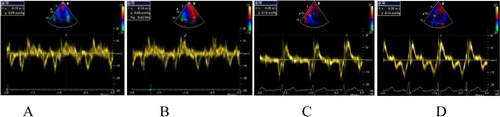
Figure 2 Average pulsed wave TD (Sm) of the patient at dobutamine stress about 17.5 cm/s. (A) Pulsed TD (Sm) at the level of basal septal about 20 cm/s, (B) Pulsed TD (Sm) at the level of basal anterior about 20 cm/s, (C) Pulsed TD (Sm) at the level of basal inferior about 15 cm/s, (D) pulsed TD (Sm) at the level of basal lateral about 14 cm/s with observed improved values during the stress test.
3.3 Tissue velocity imaging
By activating the DTI function in the echocardiographic machine, the mitral annular velocities were recorded using the pulsed-wave DTI. From the apical 4- and 2-chambers views, the longitudinal mitral annular velocities were recorded from septal, lateral, inferior and anterior LV sites. A mean value of the above four sites were used. The velocities were taken into account: the positive peak systolic velocities when the mitral annulus moved toward the cardiac apex due to longitudinal contraction of the LV. A mean of the three consecutive cycles was used to calculate all echo-Doppler parameter (See ).Citation3
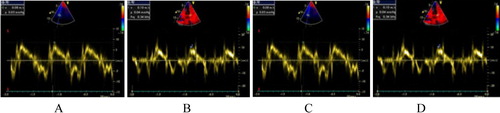
Figure 3 Average pulsed wave TD (Sm) of the patient at baseline, 1 month follow up about 9 cm/s. (A) Pulsed TD (Sm) at the level of basal septal about 8 cm/s, (B) Pulsed TD (Sm) at the level of basal anterior about 10 cm/s, (C) Pulsed TD (Sm) at the level of basal inferior about 8 cm/s, (D) Pulsed TD (Sm) at the level of basal lateral about 10 cm/s with observed improved values in comparison with the baseline values before the PCI.
All echocardiographic parameters (LVEF, WMSI and TD Sm), were detected twice (at rest and during dobutamine stress after each stage). All patients underwent coronary revascularization by elective PCI.
3.4 Angiographic procedure
Coronary angiography was performed via the femoral approach, using the standard technique with 7Fr arterial sheath. Non-infarct-related coronary was visualized first, and then IRA was visualized and treated. The goal of PCI was to restore TIMI 3 grade flow, assessed following standard criteria: with residual stenosis <30% at visual estimation, which was defined as a successful procedure. Complete procedural success was defined as <30% residual stenosis and TIMI 3 flow on every lesion treated, whereas partial success was defined as a residual stenosis >30% or TIMI <3 flow on non-IRA lesions. No-reflow phenomenon was defined as TIMI myocardial perfusion grade <3, assessed following standard criteria, and reported. Complete revascularization was defined as absence of total occlusion and/or residual stenosis >70% in any major coronary artery or their major branches at discharge (See ).Citation11
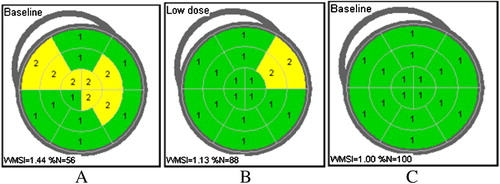
Figure 4 Wall Motion Score Index (WMSI), (A) at baseline, (B) at low dose dobutamine stress, (C) at 1 month follow up after PCI with observed improvement of the WMSI during the 3 different stages.
Follow up study:
One month later after doing elective PCI, a follow up resting conventional echocardiography and TDI were done for all patients to detect the following parameters:
| – | Left ventricular function (LVEF) to determine the global myocardial functional recovery. | ||||
| – | Wall motion score index (WMSI). | ||||
| – | Tissue velocity imaging (TD Sm). | ||||
Patients were considered to have global functional recovery at the follow up stage if their LVEF% had improved by >5% on 2-D follow up echocardiography as compared to LVEF% at basal study before revascularization.Citation12
Segmental recovery means the number of segments in each patient that showed recovery of baseline wall motion abnormalities.Citation12
4 Results
4.1 Demographic characteristics of the studied patients
The study included 60 patients, 93.3% were male and 6.66% were female with mean age 56.62 ± 2.59. As regards the risk factors of the patients 30% of the patients were diabetics, 56.66% were hypertensive, 73.33% were smokers, 63.33% were dyslipidemic and 10% had +ve FH of IHD.
As regards the clinical presentation of patients, 60% of them had previous anterior MI, 26.66% had previous inferolateral MI and 13.33% had previous NSEMI and UA. 63.33% of the patients were in Canadian class score (CCS) I, 23.33% were in class II and 13.335% were in class III. 83.33% of the patients were taking beta blockers (BB), 10% were taking calcium channel blockers (CCB), 66.66% were taking angiotensin converting enzyme inhibitors (ACEI) and 10% were taking nitrates. All patients were receiving aspirin and statins.
As regards angiographic findings of patients during coronary artery angiography, 65% of patients had single vessel disease (35% had LAD and 30% had LCX) and 35% of patients had two vessel disease (both LAD and LCX).
PCI was done to LAD in 30 patients (50%), to LCX in 19 patients (31.66%) and to both LAD and LCX in 11 patients (18.33%).
4.2 Response to dobutamine stress echo
As regards the hemodynamic response of the patients during dobutamine stress test, there were high statistically significant differences in the values of SBP, DPB and HR during stress in comparison with the rest of the values as the P-values were 0.001 ().
Table 1 Hemodynamic and echocardiographic variables of the studied patients in relation to different stages of the test.
As regards the complication developed during the DSE, 16.66% of patients developed mild anginal pain, 23.33% of them developed ECG-changes in the form of premature atrial and ventricular contractions and 6.66% developed other complications in the form of headache, dizziness and palpitation.
As regards the echocardiographic findings of the patients including the EF, WMSI and TD average (Sm), there were statistically highly significant differences between values at rest and those during the low dose stress as the P-values were 0.001 ().
4.3 At 1 month follow up
After 1 month a follow up study was done and patients were classified into two groups: 18 patients (30%) had non recovered global myocardial function (Group I) and 42 patients (70%) had recovered myocardial function both globally (improved EF) and at segmental level (improved WMSI) (Group II).
There were no statistically significant differences between the two groups as regards age and sex or risk factors as the P-value was >0.05.
As regards the clinical presentation of the studied patients according to the global functional recovery including the ACS type (STEMI, NSTEMI and UA), CCS and medical treatment including beta blockers (BB), calcium channel blockers (CCB), angiotensin converting enzyme inhibitors (ACEI) and nitrate, there were no statistically significant differences between the two groups as the P-values were >0.05.
4.3.1 Hemodynamic response in Group I
As regards the hemodynamic response of the studied patients during the dobutamine stress in non-recovered group (Group I), the mean SBP was 112.78 ± 11.14 mmHg at rest and 138.33 ± 13.39 mmHg during the stress, the mean DBP was 73.06 ± 7.3 mmHg at rest and 93.06 ± 10.02 mmHg during the stress and the mean HR was 85.67 ± 15.24 b/min at rest and 115.72 ± 18.28 b/min during the stress with statistically significant differences in relation to the different stages of the test as the P-values were highly significant (0.001).
4.3.2 Hemodynamic response in Group II
As regards the hemodynamic response of the studied patients during the dobutamine stress in recovered group(Group II), the mean SBP was 114.64 ± 8.93 mmHg at rest and 144.29 ± 9.73 mmHg during the stress, the mean DBP was 73.1 ± 7.24 mmHg at rest and 96.9 ± 6.89 during the stress and the mean HR was 87.26 ± 11.9 b/min at rest and 120.29 ± 13.49 b/min during the stress with statistically significant differences in relation to the different stages of the test as the P-values were highly significant (<0.001).
4.3.3 Comparison between the two groups as regards hemodynamic response
From a comparison between the two groups as regards the hemodynamic response of the studied patients during the dobutamine stress including SBP, DBP and HR, there were no statistically significant differences as the P-values of those parameters were >0.05. Also in a comparison between the two groups as regards the rate/pressure product (Robinson index) during the stress, there was no statistically significant difference (P-value > 0.05).
4.3.4 Echocardiographic variables in Group I
As regards echocardiographic variables of the studied patients in non-recovered group (Group I), the mean value of the EF was 52.17 ± 2.43 at rest, 55.06 ± 2.69 during the stress and 56.5 ± 1.43 at 1 month follow up and the mean value of WMSI was 1.49 ± 0.12 at rest, 1.26 ± 0.13 during the stress and 1.24 ± 0.14 at 1 month follow up while, the mean value of Sm of TD was 5.06 ± 0.91 at rest, 11.97 ± 2.36 during the stress and 5.67 ± 1.01 at 1 month follow up with statistically significant difference of the all variables in relation to the different stages of the test as the P-values were highly significant (0.001) in all variables, also as regards the difference between stress and follow up EF, P-value was significant (< 0.05) ().
Table 2 Echocardiographic response during (DSE) of the studied patients in non recovered group (Group I).
4.3.5 Echocardiographic variables in Group II
As regards echocardiographic variables of the studied patients in the recovered group (Group II), the mean value of the EF was 50.74 ± 2.72 at rest, 54.9 ± 2.48 during the stress and 56.62 ± 2.81 at 1 month follow up and the mean value of WMSI was 1.54 ± 0.11 at rest, 1.25 ± 0.08 during the stress and 1.21 ± 0.10 at 1 month follow up while, the mean value of Sm of TD was 5.5 ± 0.99 at rest, 16.02 ± 3.82 during the stress and 7.48 ± 0.92 at 1 month follow up with statistically significant difference of all variables in relation to different stages of the test as the P-values were highly significant (0.001) ().
Table 3 Echocardiographic response during (DSE) of the studied patients in non recovered group (Group II).
4.3.6 Comparison between the two groups as regards echocardiographic variables
From a comparison between the two groups as regards echocardiographic variables of the studied patients in relation to different stages of the test, there were no significant differences as regards the EF and WMSI, while, there was a statistically significant difference as regards the Sm parameter of the TD between the studied patients of both groups during the stress and 1 month follow up as the P-value was highly significant (0.001) ().
Table 4 Comparison between two groups as regards echocardiographic variables of the studied patients in relation to different stages of the test.
4.3.7 Comparison between the two groups as regards angiographic findings
Patients with single vessel disease showed a high significant incidence of the functional global recovery while, patients with two vessel disease showed a significant incidence of the non-global functional recovery.
4.3.8 Regression analysis showing the predictors of the recovery
From a comparison between the two groups as regards risk factors, a multivariate regression analysis of echocardiographic data shows no significant difference between the two groups regarding those parameters while a univariate regression analysis shows that the TD (Sm) parameter is the only predictor for the global functional recovery.
4.3.9 ROC curve for identification of cut-off value and accuracy of low dose dobutamine stress WMSI for prediction of functional recovery
By demonstration of the values derived from ROC curve for the identification of cut-off value and accuracy of WMSI parameter during low dose dobutamine stress for the prediction of functional recovery, the cut-off value was 1.35 which gave a sensitivity of 50%, specificity of 97%, PPV of 90%, NPV of 82% and accuracy of 83%. The area under the curve (AUC) was 0.493.
4.3.10 ROC curve for identification of cut-off value and accuracy of dobutamine stress TD (Sm) parameter for prediction of functional recovery
By demonstration of the values derived from ROC curve for the identification of cut-off value and accuracy of TD (Sm) parameter during dobutamine stress for the prediction of functional recovery, the cut-off value was 16 which gave a sensitivity of 100%, specificity of 74.6%, PPV of 55%, NPV of 100% and accuracy of 93.3%. The area under the curve (AUC) was 0.735 with an observed larger area under the curve (AUC) which indicates better sensitivity and accuracy of TD Sm parameter compared with the WMSI of DSE for the prediction of functional recovery of the viable myocardium after doing revascularization.
5 Discussion
The differentiation of viable from non-viable myocardium is highly relevant in patients who are being considered for revascularization. Dysfunctional but viable myocardium can still preserve a contractile reserve, which may be evoked by an appropriate stimulus.Citation13
In patients with jeopardized but viable myocardium, the LV ejection fraction (EF) will show improvement with low-dose dobutamine in direct proportion to the number of segments with contractile reserve.Citation8
Prediction of functional recovery, based on the detection of contractile reserve with dobutamine stress echocardiography (DSE), includes myocardial perfusion imaging, metabolic imaging with conventional scintigraphy and positron emission tomography (PET).Citation12
Dobutamine stress echocardiography is widely used in the clinical setting because it is a safe and accurate method for the detection of myocardial viability. The main limitation of dobutamine echocardiography is its subjective interpretation.Citation8
Several studies demonstrated the potential role of tissue Doppler imaging during dobutamine stress echocardiography to quantify myocardial velocity and deformation, instead of or in addition to traditional evaluation of the wall motion score index (WMSI).Citation14,Citation5 However, its application during stress echocardiography remains controversial since no clear advantage both in terms of test interpretation or objective quantification has been demonstrated.Citation6
Identification of small changes in myocardial wall velocities during dobutamine challenge has been shown to be feasible with TDI. Hence, TDI is a quantitative technique for the assessment of myocardial velocities and is at least as accurate in identifying viable myocardium in patients with CAD and myocardial dysfunction as other traditional qualitative method.Citation15 Previous investigators have shown that systolic velocity changes during dobutamine infusion are seen as sensitive indexes of myocardial viability.Citation16
The present study was concluded on sixty patients with IHD and hibernating viable myocardium proved by DSE who were referred for evaluation of myocardial viability prior to revascularization, then they were followed up 1 month later after doing elective PCI to detect functional myocardial recovery.
Every patient was subjected to careful history taking, full clinical examination, resting standard 12-leads ECG, full 2D, M-mode, Doppler echocardiography in the standard views, dobutamine stress and tissue Doppler velocities. All parameters including the hemodynamic data and echocardiographic variables (LVEF, WMSI and TD Sm) were assessed twice, at rest and during dobutamine stress.
All patients underwent coronary revascularization (elective PCI) after assessment by DSE and TDI. Follow up 2-D conventional echocardiography and TDI were done one month after coronary revascularization and all echocardiographic variables were assessed again at rest. Global functional recovery was identified if the EF had improved by more than 5% on the follow up study.
In the present study, patients were classified according to the global functional recovery at 1 month follow up into two groups:
Group I: included 18 patients (30%) with no global functional recovery.
Group II: included 42 patients (70%) with global functional recovery.
The mean age of our patients was 56.62 ± 2.59. 56 patients (93.33%) were male and 4 patients (6.66%) were female. As regards their risk factors, 18 patients (30%) were diabetic, 34 patients (56.66%) were hypertensive, 44 patients (73.33%) were smokers, 38 patients (63.33%) were dyslipidemic and 6 patients (10%) had previous +ve FH of IHD. As regards the clinical presentations of the patients, 36 patients (60%) had previous anterior and anterolateral MI, 16 patients (26.66%) had previous inferolateral MI and 8 patients (13.33%) had previous NSTEMI and UA. As regards the medications, all patients were receiving aspirin and statins, 50 patients (83.33%) were taking BB, 6 patients (10%) were taking CCB and 40 patients (66.66%) were taking ACEI. Angiographic findings of our patients showed 39 patients (65%) had single vessel disease (35% was LAD and 30% was LCX) and 21 patients (35%) had two vessel disease. On comparison between the two groups, there were no statistically significant differences as regards the demographic data, risk factors and clinical presentation.
On another similar study, 42 patients with previous myocardial infarction with documented significant coronary artery disease by coronary angiography were submitted for elective coronary revascularization of the infracted related artery. The mean age of the patients was 53.5 ± 8.7, 38 patients (90.5%) were male, 4 patients (9.5%) were female. As regards risk factors, 15 patients (35.7%) were diabetic, 16 patients (38%) were hypertensive, 15 patients (35.7%) were dyslipidemic and 9 patients (21.4%) had +ve FH of IHD. Regarding clinical presentation, 24 patients (57.1%) had previous anterior MI , 5 patients (11.9%) had previous inferior and lateral MI, 13 patients (31%) had previous anterior and inferior MI. As regards angiographic findings, 9 patients (21.4%) had single vessel disease, 13 patients (31%) had 2 vessel disease and 20 patients (47.6%) had 3 vessel disease.Citation17
Also, in another study, 73 consecutive patients presented with previous anterior myocardial infarction, underwent some form of coronary revascularization for the significant coronary stenosis. The mean age of those patients was 49.8 ± 10.3, 62 patients (84.9%) were male, 11 patients (15%) were female, 45 patients (61.6%) were smoker, 38 patients (52.1%) were hypertensive, 37 patients (50.5%) were diabetic, 43 (58.9%) were dyslipidemic. As regards medical treatment patients received, 48 patients (65.8%) were on BB, 54 patients (73.9%) were on ACEI and 23 patients (31.5%) were on CCB.Citation18
Since the functional recovery is the gold standard of myocardial viability assessment, the present study used the myocardial viability to detect the global functional recovery after revascularization.
The identification of contractile reserve during DSE has been shown to provide important prognostic information and clinical outcome. Contractile reserve is defined as the difference between values of an index of LV contractility during stress and its baseline values. Ejection fraction (EF) and wall motion score index (WMSI) are the most frequently used indices of LV performance.Citation12
Interestingly, from our study’s major findings, an increase in the ejection velocities of the myocardium was observed during the test in all patients. Also improvement of both global myocardial function (LVEF) and WMSI parameters was observed. The increase in ejection velocities during dobutamine stress test seems to be an reliable index for accurate identification of myocardial viability in patients with ischemic heart disease and subsequent myocardial recovery after coronary revascularization.
In agreement with the present study Gorcson et al., who demonstrated increased sensitivity of myocardial viability detection by using pulsed wave Doppler tissue samplings compared to dobutamine stress echocardiography.Citation19
Also, Hoffmann et al. had validated the TDI technique as a clinical tool and that study correlated the dobutamine response with metabolic evidence of viability by PET. Thirty-seven patients with ischemic heart disease who underwent low-dose dobutamine stress echocardiography and positron emission tomography were studied. Viability was defined on the basis of perfusion metabolism mismatch and tissue velocity imaging was found to be more accurate than dobutamine in the prediction of viability.Citation20
Also Penicka et al. tested the ability of peak systolic velocities to predict recovery of myocardial function after coronary revascularization. They showed that a positive systolic velocity after revascularization predicts recovery of function in the reperfused area. This suggests that the measurement of systolic velocities may provide important diagnostic information with regard to myocardial viability and subsequent recovery after coronary revascularization.Citation21
Similarly, Manish et al. compared myocardial tissue velocity imaging and speckle tracking echocardiography (STE) for the prediction of myocardial viability at dobutamine stress echocardiography. Fifty-five patients with ischemic heart disease underwent DSE for evaluation of myocardial viability. Functional recovery was defined by improved wall motion-score on side-by-side comparison of echocardiography images before and after revascularization. Only TD parameter predicted the functional recovery independent of wall motion analysis.Citation22
In the present study, echocardiographic variables of EF, WMSI and average (Sm) parameter of TDI at rest, dobutamine stress and one month follow up resting values were assessed. For each parameter assessed, values in different groups were related to different stages of the test; they were related to global functional recovery. All the studied parameters showed statistically significant differences as regards stages of the test and at follow up study. There were statistically significant differences as regards the Sm parameter of TD values in relation to global functional recovery and this can be explained by improvement in contractility and related to pathological changes if the amount of viable myocytes in relation to fibrotic tissue is too high and also, improved the integrity of cardiac myocyte cell membranes after revascularization. However, as regards global functional recovery, EF & WMSI were not statistically significantly different and these can be explained by a delayed improvement in the myocardial relaxation and a varying lag in contractile recovery after revascularization as in most studies, follow up improvements in those parameters were observed between 6 and 9 months.
In agreement with our findings, Auerbach et al. found no significant difference as regards LVEF between patients with contractile recovery and those without myocardial recovery after revascularization.Citation23
In disagreement with that, Leclercq et al. proved that there is a better significant correlation between the left ventricular function and contractile recovery in comparison with non-recovery after revascularization. And these controversies can be explained by different heterogeneous nature of the underlying disease process and lack of uniformity in patient selection and study protocols among different studies.Citation24
In agreement also with our study findings, there were several studies that tested the accuracy of TD parameter for the prediction of functional recovery after revascularization, as well discussed in the following:
Katz et al. assessed the accuracy of TD and concluded that peak ejection velocities of the dysfunctional viable myocardium predict recovery after reperfusion.Citation25
Also, Yamada et al. assessed the value of TD during DSE in the detection of contractile reserve and demonstrated that higher Sm velocity of TD was associated with improved global LV function after revascularization.Citation26
In agreement with this study, another additional study reported that systolic mitral annular motion toward the cardiac apex measured with echocardiography could have a high degree of sensitivity and specificity for the detection of myocardial viability. It was found that a correlation between ejection fraction and the systolic mitral annular velocity is relatively good irrespective of the presence or absence of mitral regurge.Citation27
Also, Penicka et al., used low-dose dobutamine TD parameters (peak systolic velocities and pre-ejection velocities) to predict myocardial functional recovery after revascularization and found those parameters more specific and accurate compared with WMSI detected with DS.Citation21
Also from our finding, ROC curve statistical analysis shows that TD Sm is more sensitive and accurate than WMSI in the detection of viable myocardium which predicts improvement after revascularization (sensitivity 100%, 50% and accuracy 93.3%, 83.3% respectively).
In agreement with our study, Celutkiene et al. reported that the peak systolic velocity during DSE was the most accurate index of prediction of contractile reserve (sensitivity 73–100%, specificity 82–97%).Citation28
Also, Antonio et al. assessed quantitative segmental analysis by TDI technique during DSE for detecting myocardial recovery after revascularization in patients with IHD and segmental myocardial dysfunction and compared results with those of 2D echocardiography and tissue Doppler imaging (TDI) as well as rest – 4–24 h redistribution thallium SPECT. Forty-one patients underwent dobutamine 2D/TDI and SPECT before and after revascularization. Sensitivity, specificity and accuracy of regional myocardial recovery were 73%, 81% and 77% for dobutamine 2D and 77%, 82% and 80% for dobutamine TDI.Citation29
In another report, Aggelic et al. investigated low dose dobutamine stress echocardiography combined with tissue Doppler imaging for the assessment of myocardial recovery after revascularization. Conventional qualitative LDDSE showed sensitivity of 78%, specificity of 85% for prediction of recovery.Citation30
Also, Enbiya et al. concluded that strain/strain rate imaging was better for myocardial deformation changes following PCI and for assessment of viability than tissue Doppler velocity imaging (TDI). SR > strain > TDI (P-value = 0.004, 0.012 and 0.099 respectively).Citation31
Also from our observed findings as regards the angiographic data, from a comparison between the two groups, patients with single vessel disease (39 patients 65%) showed a highly significant incidence of recovery while, patients with two vessel disease (21 patients 35%) showed a significant incidence of the non-functional recovery. This can be explained by the extensive presence of microvascular obstruction in patients with multivessel disease which affects the success of the reperfusion process and subsequent myocardial remolding that impacts recovery.
In agreement with those findings, Paul et al. concluded that patients with extensive CAD remote from the infracted related artery have reduced reperfusion success, myocardial recovery and associated adverse clinical outcome.Citation32
Also, Stein et al. reported that patients with multivessel disease showed delayed recovery and adverse outcomes in comparison with those with single vessel.Citation33
From the previously mentioned results, it has been suggested that TDI provides a feasible and quantitative technique that improves reproducibility of dobutamine stress echocardiography. Peak systolic velocity (PSV) of TDI with low-dose dobutamine showed better accuracy than visual assessment of WMSI during DSE for the prediction of functional recovery following revascularization. However, that needs to be confirmed in studies with larger patient population.
6 Conclusion
From the previously mentioned results, it has been suggested that stress TDI provides a feasible and quantitative technique that improves reproducibility of dobutamine stress echocardiography. Systolic tissue velocity imaging (Sm) during dobutamine stress showed better accuracy than visual assessment of WMSI for the prediction of functional recovery following revascularization.
Among the different TDI parameters, systolic velocity (Sm) was a simple, sensitive and accurate parameter for that purpose even in the detection of subtle myocardial systolic velocity changes.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 12 December 2014
References
- K.RosamondK.FlegalK.FurieHeart disease and stroke statistics: a report from AHA statistics and stroke statistics subcommitteeCirculation11720102547
- H.SedaghianJ.Majd-AldakaniM.Lotfi-TokaldanyM.CullochComparison between dobutamine stress echocardiography (DSE) and myocardial perfusion imaging to detect viable myocardium in patients with CADHellenic J Cardiol50120094551
- J.ZamoranoA.DuqueM.BaqueroV.AntonioM.TeresaG.CarioStress echocardiography in the pre-operative evaluation of patients undergoing major vascular surgery. A new results comparable with dipyridamole versus dobutamine stress echo?Rev ESP Cardiol552002121126
- T.ShiotaC.AsherN.SmediraD.BachD.MullerB.GrosUsefulness of real-time three dimensional echocardiographic cardiomyopathy for evaluation of myectomy in patients with hypertrophic cardiomyopathyJ Am Coll Cardiol942004964966
- H.BadranS.ShalabyA.SeragMyocardial contractile reserve detected by dobutamine stress tissue doppler imaging as a preoperative determinant of outcome after valve replacement in chronic mitral regurgitationEur Heart J2009455530
- A.Mor-AviR.LangL.BandanoM.BakerR.BattleM.SahaCurrent and evolving echocardiographic techniques for quantitative evaluation of cardiac mechanism: ASE/EAE consensus statement on methodology and indication indorsed by Japanese Society of EchocardiographyCirculation1122011167205
- D.AnandI.TheodosiadisR.SeniorImproved interpretation of dobutamine stress echocardiography following 4 months of systematic training in patients following acute myocardial infarctionEur J Echocardiogr320041217
- P.CainT.BaglinC.CaseM.BrownR.NorrisM.TakayamaApplication of tissue Doppler to interpretation of dobutamine echocardiography and comparison with quantitative coronary angiographyAm J Cardiol8752006525531
- B.PaulR.KasliwalDobutamine stress echocardiography methodology. Clinical application and current perspectivesJAPI522004324329
- R.LangM.BierigR.DevereuxM.CompellL.MachinRecommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of CardiologyJ Am Soc Echocardiogr18200514401463
- C.GibsonC.CannonS.MurphyA.GopalA.KellerZ.ShenRelationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugsCirculation1012000125130
- A.EinsteinK.MoserR.ThompsonW.KatzV.GulatiC.MahlerRadiation dose to patients from cardiac diagnostic imagingCirculation11611200712901305
- L.PierardE.PicanoMyocardial viabilityE.PicanoStress echocardiography2009SpringerBerlin, Germany273294
- T.MarwickC.CaseR.LeanoUse of tissue Doppler imaging to facilitate the prediction of events in patients with abnormal left ventricular function by dobutamine echocardiographyJ Am Coll Cardiol932004142146
- O.Najos-ValenciaP.CainC.CaseS.LalkaS.SwadaM.DalsingDeterminates of tissue Doppler measures of regional diastolic and systolic function by dobutamine stress echocardiographyAm Heart1442002516523
- R.RambadiD.PoldermansJ.BaxDoppler tissue velocity sampling improves diagnostic accuracy during dobutamine stress echocardiography for the assessment of viable myocardium in patients with left ventricular dysfunctionEur Heart742000107113
- D.KhaledA.IhabO.AhmedPer ejection mitral annular motion velocity response to dobutamine infusion: a quantitative approach for assessment of myocardial viabilityJ Saudi Heart Assoc251120041522
- A.WalaaN.WailPredictors of contractile recovery after revascularization in patients with myocardial infarction and received thrombolyticsInt J Angio19220107882
- J.GorcsanIIIA.DeswalS.MandakR.LaneS.SawadaD.SegorQuantification of myocardial response to low-dose dobutamine using tissue Doppler echocardiographic measures of velocity and velocity gradientsAm J Cardiol811998615623
- R.HoffmannE.AltiokB.NowakR.LeeL.HunekomTissue Doppler imaging allows improved assessment of myocardial viability in patients with left ventricular dysfunctionJ Am Coll Cardiol392002443449
- M.PenickaJ.BatunekW.WijnsTissue Doppler imaging predicts recovery of left ventricular function after revascularization of an occluded coronary arteryJ Am Coll Cardiol4320048591
- B.ManishJ.LeanneL.RodelD.PaganoJ.TownendD.ParumsAssessment of myocardial viability at dobutamine echocardiography by deformation analysis using tissue Doppler velocity and speckle trackingJ Am Coll Cardiol322010121131
- M.AuerbachH.SchoderC.HohR.SicariA.RipoliE.PicanoPrevalence of myocardial viability as detected by positron emission tomography in patients with ischemic heart diseaseCirculation99200029212926
- F.LeclercqM.MessenerP.PellencMyocardial viability assessed by dobutamine echocardiography in acute myocardial infarction after successful coronary angioplastyAm J Cardiol802000610
- W.KatzV.GulatiC.MahlerS.SiuJ.RiveraJ.CuerreroQuantitative evaluation of segmental left ventricular response to dobutamine stress by tissue Doppler echocardiographyAm J Cardiol79199710361042
- E.YamadaM.GarciaJ.ThomasS.TakumaD.ZwasMyocardial Doppler velocity imaging – a quantitative technique for interpretation of dobutamine echocardiographyAm J Cardiol821998806809
- M.AlamJ.WardellE.AndersonAssessment of left ventricular function using mitral annular velocities in patients with ischemic heart disease with or without the presence of significant mitral regurgeJ Am Soc Echocardiogr1632003240245
- J.CelutkieneG.SatherlandA.LauceviciusP.PellikaJ.OhK.BaileyPeak systolic velocity and post systolic motion is the optimal ultrasound parameter to detect induced ischemia during dobutamine stress echoEur Heart J252004932942
- V.AntonioM.TeresaG.CarioM.OppizziM.PisaniA.MerisTissue Doppler dobutamine echocardiography for prediction of recovery after revascularization in patients with myocardial dysfunctionJ Card Fail122006268275
- C.AggelicG.GiannopoulosG.RoussakisPre ejection tissue Doppler velocities changes during low dose dobutamine stress predict segmental myocardial viabilityHellenic J Cardiol98120072329
- A.EnbiyaG.YektaS.BedriAssessment of regional myocardial deformation changes and viability in anterior myocardial infarction patients by tissue Doppler imagingJ Am Coll Cardiol1062010479487
- S.PaulJ.BernardA.DavidL.PierardE.PicanoImpact of multivessel disease on reperfusion success and clinical outcome in patients undergoing percutaneous coronary intervention for the myocardial infarctionEur Heart J26200717091716
- O.SteinM.CordG.OleR.TeoliC.CutanticG.PusanisiMicrovascular obstruction is a major determinant of infarct healing and subsequent ventricular remolding following the percutaneous coronary interventionEur Heart J20090814
