Abstract
Introduction
Intussusception occurs when a segment of bowel, the intussusceptum, prolapses and invaginates into another segment, the intussuscipiens. It is the most common cause of acute bowel obstruction in infants. Over 90% of childhood intussusceptions are idiopathic, perhaps related to relative hyperplasia of lymphoid follicles in the distal ileum. Underlying pathologic lead points are uncommon. Lymphoma, polyps, Meckel’s diverticulum and hematoma are most common identified lead points in children.
Aim of the work
To assess the role of multidetector computed tomographic imaging in the diagnosis of secondary intussusception with pathological leading points in children.
Materials and methods
This study is a retrospective study including 12 children referred to the radiodiagnosis department at Alexandria University Hospitals presenting with signs of acute abdomen, in the period between June 2012 and January 2013, all of which were radiologically diagnosed by computed tomographic imaging as secondary intussusception with pathological leading points which were confirmed by surgery. All the studied patients were subjected to full history taking, thorough clinical examination, laboratory investigations and CT of the abdomen and pelvis: using multidetector row CT.
Results
All the patients were radiologically diagnosed by computed tomographic imaging as secondary intussusception with pathological leading points which were confirmed by surgery. The associated leading points detected in our cases were reactive mesenteric lymph nodes in three patients, lymphoma in four cases, one post appendectomy case, mesenteric lymphangioma in one case, malrotation in one case and Meckel’s diverticulum in another one case. Intramural hematoma was detected in one case diagnosed as Henoch–Schönlein purpura (8.33%).
Conclusions
Finally we conclude that multidetector CT could efficiently diagnose children presenting with secondary intussusceptions.
Keyword:
1 Introduction
Intussusception occurs when a part of the bowel, the intussusceptum, prolapses into another part, the intussuscipiens.Citation1,Citation2 It is the most common cause of acute bowel obstruction and pain in infants. This leads to venous congestion and bowel wall edema. If intussusception is not diagnosed and treated adequately, reduced arterial blood supply, bowel infarction and perforation may follow, causing peritonitis and may even cause death. Four types of intussusception are described: ileocolic; ileo-ileo colic; colo-colic; and ileo-ileal. Ileocolic is the most frequent and occurs in 90% of cases.Citation3,Citation4
Figure 2 A 12 year old girl with a history of appendectomy from 10 days (A, B) axial, (C) coronal and (D) sagittal contrast enhanced CT abdomen and pelvis images showing intussusception of ileal segment into another one (black arrow). It is associated with proximal dilatation of the bowel loops and pneumoperitoneum (white arrow) (note the surgical emphysema on the operative side). The CT diagnosis was postoperative ileo-ileal intussusception complicated by intestinal obstruction and perforation. The management was surgical resection anastomosis.
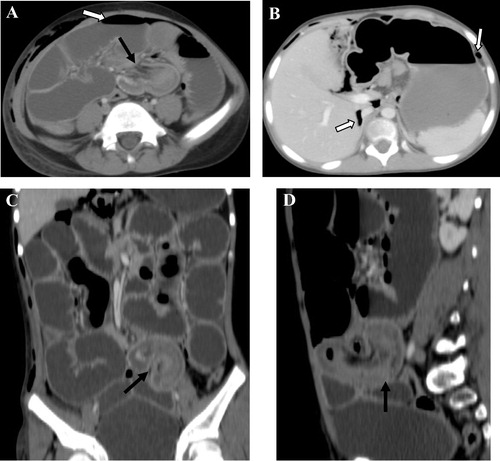
Figure 3 (A, B) Axial, (C) coronal and (D) sagittal contrast enhanced CT abdomen and pelvis images of a 15 year old boy showing ileo-ileal intussusception (arrow) at mid lower abdomen where a long bowel loop is seen invaginating into an ileal loop complicated by proximal intestinal obstruction. The CT diagnosis was ileo-ileal secondary intussusception with intestinal obstruction. The CT findings of intussusception at this site with small bowel obstruction might suggest Meckel’s diverticulum as a leading point for intussusception. The management of this case was surgical resection anastomosis and the presence of Meckel’s diverticulum was confirmed intraoperatively.
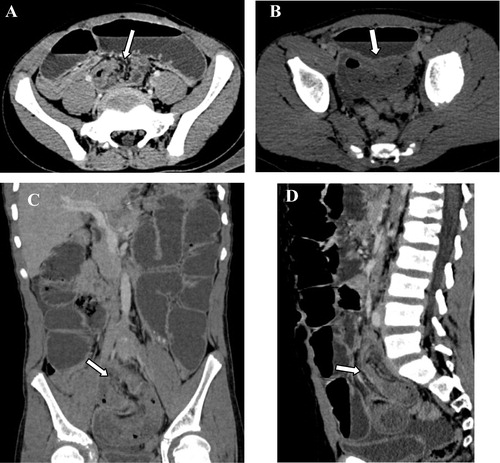
Figure 4 (A, B) Axial contrast enhanced CT abdomen and pelvis images of a 4 year old boy showing ileo-colic intussusception showing target sign appearance (white arrow) with thin walled multiloculated mesenteric cystic lesion (black arrows), associated with marked fluid collection. Note the collapsed bowel loops. The CT diagnosis of this child was ileo-colic intussusception secondary to mesenteric lymphangioma. The management of this case was surgical, and the diagnosis was confirmed hitopathologically.
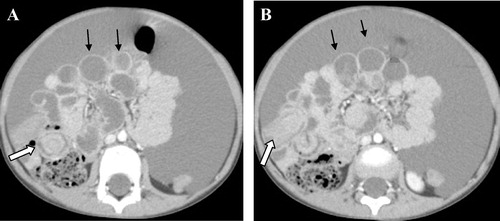
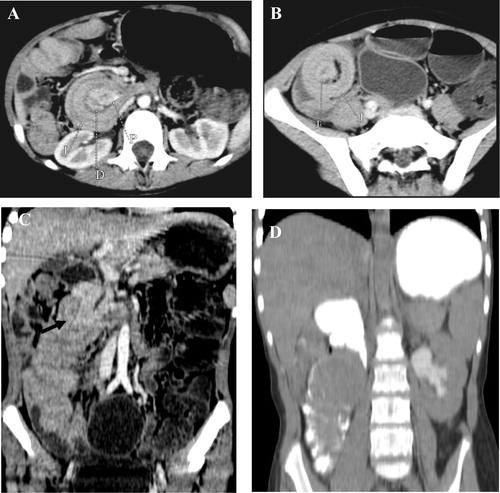
Figure 5 (A,B) Axial images and (C,D) coronal contrast enhanced CT abdomen and pelvis images of a 13 year old boy showing two segments of ileo-ileal intussusception (straight arrow) on the right side of the abdomen. Note the multiple pathologically enlarged mesenteric lymph nodes (curved arrow). The CT diagnosis of this case was ileo-ileal intussusception secondary to lymphoma. The diagnosis was confirmed surgically.
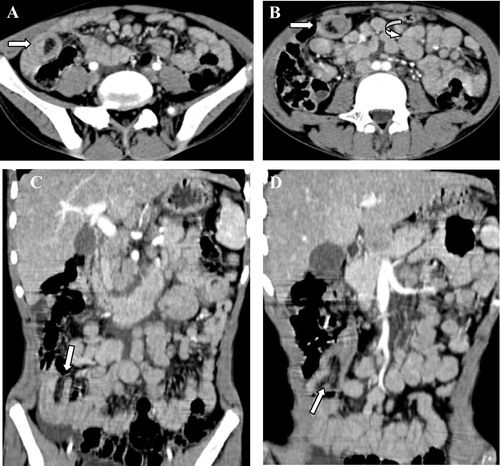
Figure 6 (A, B) Axial, (C) sagittal and (D) coronal contrast enhanced CT abdomen and pelvis images of a 12 year old boy showing ileo-colic intussusception (curved arrow) is noted with mural thickening of the ileal loop with soft tissue mass lesion (straight white arrow) showing homogenous texture, mild enhancement associated with multiple enlarged mesenteric lymph nodes (black arrow). The CT diagnosis was ileo-colic intussusception secondary to intestinal lymphoma. The diagnosis was confirmed by surgery and histopathology.
Over 90% of intussusceptions in children are of the idiopathic type, likely attributed to relative hyperplasia of lymphoid follicles in the distal ileum. However intussusception could be secondary to underlying pathologic lead points like lymphoma, polyps, Meckel’s diverticulum and hematomas. Most patients are six months to four years of age with the peak incidence of idiopathic intussusception between the ages of 3 and 9 months. Pathological leading points are highly suspected in patients younger or older than this age range. The diagnosis of secondary intussusception is essential for planning for eventual surgical management and avoiding reduction techniques used for the treatment of primary type.Citation3
Ultrasound has a nearly 100% diagnostic accuracy in expert hands in case of primary intussusception. Ultrasound should be performed with a high-frequency linear-array probe. The intussusception in transverse section has a hypoechoic outer ring and a hyperechoic center and is known as the target or doughnut sign. In longitudinal section there are alternating hypoechoic and echogenic layers giving a pseudokidney or sandwich appearance. The hypoechoic layer is due to oedematous bowel wall and the echoic center, the mucosa and trapped intraluminal content. However there is difficulty in the detection of associated pathological points via ultrasonography in cases of secondary intussusception.Citation5,Citation6
CT is an efficient imaging tool for disorders of the abdomen especially after the invention of multidetector CT which has resulted in several important advantages. After the increasing use of CT scans in pediatric patients with atypical abdominal complaints, unsuspected intussusceptions have been more frequently diagnosed. CT appearance of intussusception includes a target sign, a sausage-shaped mass of different layers of attenuation, and/or a less-defined kidney-like mass. One of the main goals of CT in these cases is the detection of associated pathological leading points like polyps and lymphoma.Citation7
The aim of this study is to assess the role of multidetector computed tomographic imaging in the diagnosis of secondary intussusception with the pathological leading points in children.
2 Materials and methods
This study is a retrospective study including 12 children referred to the radiodiagnosis department at Alexandria University Hospitals presenting with signs of acute abdomen, in the period between June 2012 and January 2013, all of which were radiologically diagnosed by computed tomographic imaging as secondary intussusception with pathological leading points which were confirmed by surgery.
All the studied patients were subjected to the following:
| 1. | Full history taking, thorough clinical examination and laboratory investigations. | ||||
| 2. | Plain X-ray of the abdomen and pelvis (standing or decubitus views) for detection of intestinal obstruction and air under diaphragm. | ||||
| 3. | Ultrasonography of the abdomen and pelvis. | ||||
| 4. | CT of the abdomen and pelvis: using 16 multidetector row CT scanner. All patients were scanned after IV contrast injection. A pre contrast scan was obtained followed by IV contrast injection with the venous phase obtained with a delay time of 35 s. The IV contrast material used was of the non-ionic type namely (Iopromide 300) with a dose of 1.5 mg/kg. Automatic injection was used with a rate of 3 ml/s in 10 children older than 4 years while manual injection was used in two children younger than 4 years. Scanning parameters for children were considered by adjusting the peak kilovoltage and tube current settings (mAs) to minimize the radiation dose delivered to the pediatric patients. The examinations were done on a 16 slice MDCT scanner: MX 16 (Philips Netherland) Eindhoven). The scanning parameters used were: 100 mAs, 110 KVP, tube rotation time of 0.6 s/rot., 2 mm slice thickness and 1 mm reconstruction increment for Philips MDCT, while for Siemens these were: 80 mAs, 110 KVP, 0.8 s/rot., 2.5 mm slice thickness and 1.25 mm reconstruction increment. Sedative techniques were only used in five patients to control the excessive movements of these children and its impact on the multiplanar and reconstructive techniques. They received the sedative dose of intravenous thiopental sodium 3 mg/kg. MDCT images were reconstructed using filtered reconstruction algorithms. The thin slices were sent to the workstation, after reconstruction of the raw data using medium soft tissue reconstruction algorithms (B30), where they were available to be viewed in axial, sagittal and coronal planes. | ||||
The medical ethics were considered and the protocol of the research was approved by the research ethical board in Alexandria faculty of medicine: The parents were aware of the examination, parents’ agreement was obtained and the child had to get benefit from the examination. Informed consent was taken from the relative. The feedback of the medical, surgical and histopathological data was obtained whenever available.
3 Results
This study included 12 children referred to the radiodiagnosis department at the Alexandria University Hospitals presenting with signs of acute abdomen, in the period between June 2012 and January 2013, all of which were radiologically diagnosed by computed tomographic imaging as secondary intussusception with pathological leading points which were confirmed by surgery. The age of studied patients ranged between 3 years and 15 years.
All the patients presented with acute abdominal pain. Ten patients presented with abdominal distention, five patients presented with fever, four patients presented with constipation and five patients presented with vomiting. Elevated leukocytic count was detected in five patients.
According to the site of the intussusception, six cases were of the ileo-ileal type, five cases were of ileo-colic type and one patient had two segments of intussusception of duodeno-jejunal and jejuno-jejunal type. The associated leading points detected in our cases were reactive mesenteric lymph nodes in three patients, lymphoma in four cases, one post appendectomy case, mesenteric lymphangioma in one case, malrotation in one patient and Meckel’s diverticulum in another one case. Intramural hematoma was detected in one case diagnosed as Henoch–Schönlein purpura ().
Table 1 Summary of the leading points detected in cases of secondary intussusception.
Out of the 12 patients, seven cases were uncomplicated and five patients were complicated. Detected complications were small intestinal bowel obstruction in three patients, ischemic bowel changes in four patients and bowel perforation in one case. The diagnosis was confirmed by the surgical feedback.
In all cases abdominal plain radiography was done showing multiple air–fluid levels in three cases, otherwise no definite findings could be detected and no definite complete diagnosis was reached on this imaging modality.
US of the abdomen and pelvis was done in all cases showing target sign of the intussusception in ten patients, dilated bowel loops in three patients and free fluid collection noted in nine patients. No definite pathological leading point could be detected in any of the patients.
The MDCT findings detected in all cases of secondary intussusception were telescoping of the bowel loops. Free fluid collection was detected in nine cases. Specific CT findings related to the causative pathological lead points were also reported and were the main cornerstone for diagnosis.
In four cases of lymphoma, the specific findings included multiple pathologically enlarged abdominal lymph nodes, one of them showed intestinal mural thickening and soft tissue intestinal mass lesion.
Multiple reactive mesenteric lymph nodes were detected in three cases associated with bowel intussusception without definite specific signs for lymphoma histopathology after surgery confirmed the absence of lymphoma.
In the case of mesenteric lymphangioma, the specific CT finding was the detection of thin walled multiloculated cystic mesenteric lesion forming a leading point for an ileo-colic intussusception associated with marked fluid collection.
In the case of malrotation, the duodeno-jejunal junction was noted on the right side of the vertebral column which was associated with jejuno-jejunal intussusception with invagination of the head of the pancreas into it.
The patient diagnosed with Henoch–Schönlein purpura showed an intramural hematoma as an initial mural hyperdensity in the bowel wall in the precontrast image forming a leading point for an ileo-ileal intussusception.
In the patient diagnosed with Meckel’s diverticulum, the site of the ileo-ileal intussusception at the mid lower abdomen was the key finding for diagnosis.
MDCT findings detected in the complicated cases included; dilated small bowel (SB) loops in the three cases complicated by intestinal obstruction, thickened edematous less enhancing bowel wall in the four cases complicated by ischemia and pneumoperitoneum detected in the case complicated by bowel perforation.
– show demonstration of CT findings in seven patients included in this study.
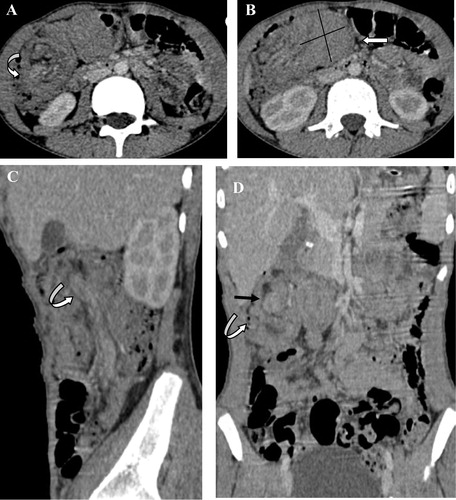
Figure 1 A 4 year old girl with a history of Henoch–Schönlein purpura (A) axial pre-contrast CT image showed initial mural hyperdensity involving the intussusceptum loop reflecting intramural hematoma (white arrow), (B–D) axial contrast enhanced CT abdomen and pelvis images showed intussusception of the long segment of ileal loop into another one. The intussusceptum showed thickened edematous wall (black arrow), associated with proximal small bowel dilatation and fluid collection. The CT diagnosis was ileo-ileal intussusception secondary to intra-mural hematoma complicated with ischemia and intestinal obstruction. The management of this case was surgical resection-anastomosis.
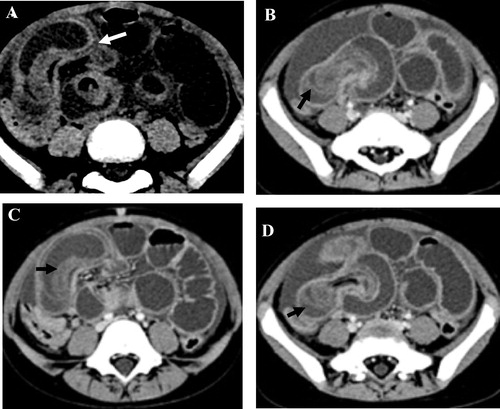
Figure 7 Contrast enhanced CT of the abdomen and pelvis of a 7 year old girl (A) axial image showed duodeno-jejunal intussusception with the head of the pancreas (P) seen invaginating within the intussusception. (B) Axial image showed jejuno-jejunal intussusception. (C) Coronal image showed the pancreatic head (black arrow) invaginating into the jejunum. (D) Coronal image with oral positive contrast showed the duodeno-jejunal junction on the right side of the vertebral column, denoting intestinal malrotation. The CT diagnosis was duodeno-jejunal and jejuno-jejunal intussusceptions associated with intestinal malrotation. The diagnosis was confirmed surgically. (D = duodenum, J = jejunum, P = pancreas.)
shows the different CT findings detected in the examined patients.
Table 2 Summary of MDCT findings in secondary intussusception cases.
4 Discussion
This study included 12 children referred to the radiodiagnosis department at Alexandria University Hospitals presenting with signs of acute abdomen, in the period between June 2012 and January 2013, all of which were radiologically diagnosed by computed tomographic imaging as secondary intussusception with pathological leading points which were confirmed by surgery.
In the current study, MDCT exams were done considering the ALARA (‘as low as reasonably achievable’) general principles to minimize the radiation exposure to children while maintaining diagnostic image quality. Justification for the requested study and adjusting the CT parameters regarding the peak kilovoltage and tube current settings (mAs) to minimize the radiation dose delivered to the pediatric patients was also considered. These considerations matched with the guidelines of, Kalra et al.,Citation8 Shah et al.,Citation9 and McCollough et al.,Citation10 who stated that the pediatric radiologists should apply the practice of ALARA (‘as low as reasonably achievable’) to minimize radiation exposure to children while maintaining the efficiency and the reliability of the diagnostic modality by justification of the use of CT for the specific diagnostic task and considering the dose reduction strategies considering the scanning parameters of the pediatric protocols.
Ko et al.,Citation11 mentioned that on MDCT and MRI, the presence of a bowel-within bowel configuration with inclusion of mesenteric fat and/or mesenteric vessels is diagnostic for intussusception. However, in infants and children, these methods should be only used for complex diagnostic situations, when US is inconclusive or atypical, or when complications such as suspicion of an oncological disease require additional imaging which was the situation in the present study. Tseng et al.,Citation12 stated that both plain film X-rays and abdominal ultrasonography had lower diagnostic accuracies compared with MDCT of the abdomen and pelvis in acute abdomen pediatric patients. This is matching with the present study in which plain radiography and ultrasonography failed to reach a complete diagnosis and CT was ordered to reach a complete diagnosis.
Ko et al.,Citation11 demonstrated that MDCT was 100% sensitive in the diagnosis of pediatric small bowel intussusception disease (SBID). CT also allowed detection of pathological lead points. Moreover, CT is also helpful in detection of other abdominal conditions, changing the diagnosis and treatment. It is also observed that the pediatric small bowel intussusception disease (SBID) may present with nonspecific symptoms and may be similar to that of ileocolic intussusception leading to delayed operative intervention. Navarro et al.,Citation13 and Linke et al.,Citation14 stated that less than 5% of intussusceptions in infants occur sequel to pathological lead points (PLPs) and this rate increases up to 60% in the 5- to 14-year age group. Intussusception has also been reported post-operatively. Also Ko et al.,Citation3 CartyCitation2 and StrouseCitation1 stated that the most common pathological lead points in intussusception are Meckel’s diverticulum, polyp, lymphoma, duplication cyst, cystic fibrosis, Henoch–Schönlein purpura and celiac disease. In the present study CT adequately detected the pathological leading points in all the examined patients. In four cases of lymphoma, the diagnostic findings included multiple pathologically enlarged abdominal lymph nodes, one of them showed an intestinal mural thickening and soft tissue intestinal mass lesion. Multiple reactive mesenteric lymph nodes were detected in three cases associated with bowel intussusception without definite specific signs for lymphoma histopathology after surgery confirmed the absence of lymphoma. A case of mesenteric lymphangioma, showed thin walled multiloculated cystic mesenteric lesion forming a leading point for an ileo-colic intussusception associated with marked fluid collection. In a case of malrotation, the duodeno-jejunal junction was noted on the right side of the vertebral column which was associated with jejuno-jejunal intussusception with the invagination of the head of the pancreas into it. In a patient diagnosed with Henoch–Schönlein purpura an intramural hematoma as an initial mural hyperdensity in the bowel wall in the pre-contrast image formed a leading point for an ileo-ileal intussusception. One patient was diagnosed with Meckel’s diverticulum, the site the of the ileo-ileal intussusception at the mid lower abdomen was the key finding for diagnosis.
Ko et al.,Citation3 and Puapong et al.,Citation7 mentioned that the bowel complications in intussusception include ischemia, necrosis and perforation. Five patients in the present study presented with complications. Sahu et al.,Citation15 stated that the presence of severe engorgement of the mesenteric vessels, loss of layered pattern, extraluminal fluid collection and bowel perforation may raise the possibility of intestinal necrosis. The complications detected in our cases were small intestinal bowel obstruction in three cases, ischemic bowel changes in four patients and bowel perforation in one case. The CT findings detected in the complicated cases include dilated small bowel (SB) loops in the three cases complicated by intestinal obstruction, thickened edematous less enhancing bowel wall in the four cases complicated by ischemia and pneumoperitoneum detected in the case complicated by bowel perforation.
5 Conclusion
Finally we conclude that multidetector CT could efficiently diagnose children presenting with secondary intussusceptions and could adequately detect the site and nature of the associated pathological leading points, still the examination has to be reviewed by an experienced pediatric radiologist who is oriented with such clinical entity and aware of the practice of ALARA (‘as low as reasonably achievable’) principles for the reduction of radiation exposure to children and he should consider the dose reduction strategies and the scanning parameters of pediatric protocols which are essential before utilizing the CT in imaging of children.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 2 December 2014
References
- P.StrouseImaging and the child with abdominal painSingapore Med J442003312322
- H.M.CartyPaediatric emergencies: non-traumatic abdominal emergenciesEur Radiol12200228352848
- H.S.KoJ.P.SchenkJ.TrogerW.K.RohrschneiderCurrent radiological management of intussusception in childrenEur Radiol17200724112421
- Andrei S.PuryskoErick M.RemerHilton M.Leão FilhoLeonardo K.BittencourtRodrigo V.LimaDouglas J.RacyBeyond appendicitis: common and uncommon gastrointestinal causes of right lower quadrant abdominal pain at multidetector CTRadiographics312011927947
- J.RatcliffeS.FongI.CheongP.O’ConnellThe plain abdominal film in intussusception: the accuracy and incidence of radiographic signsPediatr Radiol221992110111
- P.VerscheldenD.FiliatraultL.GarelA.GrignonG.PerreaultJ.BoisvertIntussusception in children: reliability of US in diagnosis–a prospective studyRadiology1841992741744
- D.PuapongS.L.LeeG.RadnerP.I.TsaiD.S.KatzM.A.AbbasComputed tomography findings of unanticipated prolonged ileocolic intussusception in childrenPermanente J12200822
- M.K.KalraM.M.MaherT.L.TothL.M.HambergM.A.BlakeJ.A.ShepardStrategies for CT radiation dose optimizationRadiology2302004619628
- N.B.ShahS.L.PlattALARA: is there a cause for alarm? Reducing radiation risks from computed tomography scanning in childrenCurr Opin Pediatr202008243247
- C.H.McColloughA.N.PrimakN.BraunJ.KoflerL.YuJ.ChristnerStrategies for reducing radiation dose in CTRadiol Clinics North Am47200927
- S.F.KoM.M.TiaoC.S.HsiehF.C.HuangC.C.HuangS.H.NgPediatric small bowel intussusception disease: feasibility of screening for surgery with early computed tomographic evaluationSurgery1472010521528
- Y.C.TsengM.S.LeeY.J.ChangH.P.WuAcute abdomen in pediatric patients admitted to the pediatric emergency departmentPediatr Neonatol492008126134
- O.NavarroA.DanemanIntussusceptionPediatr Radiol342004305312
- F.LinkeF.EbleS.BergerPostoperative intussusception in childhoodPediatr Surg Int141998175177
- S.SahuB.JohnK.MishraS.DhavalaIntussusception: pain abdomen in paediatrics revisitedMed J Armed Forces India632007380381
