Abstract
Rectal cancer is associated with a high risk of metastases and local recurrence; local recurrence rates after surgical treatment being up to 32% (1). Local recurrence is directly related to incomplete tumor resection (2, 3) and also related to the circumferential safety of resection (4, 5). An accurate local staging at the time of initial diagnosis is therefore very important.
Aim
The aim of this study is to use MRI in comparing the morphologic features of rectal cancer before and after 6 weeks of chemo irradiation treatment and to correlate the post treatment MRI appearances with the histological findings in resected tumors.
Material and methods
68 patients with histopathologically proven rectal adenocarcinoma received standardized 5-week chemo radiation therapy and subjected to MRI before and after treatment for clinical staging. A correlation between pathological response and MRI findings was done.
Result
Sixty-eight patients with adenocarcinoma rectal cancer were included in the study. Preoperative MRI examination was performed. All patients subsequently underwent operation. The mean time lag between the MRI study and operation was 16.8 days.
After preoperative chemo-radiotherapy, MRI findings showed that, there is a significant shift toward downstaging. 16/59 (23.5%) patients achieved down-staging from clinical stage III (before therapy) to stage II after therapy (P = 0.001) by achieving both tumor (T) downsizing and lymph node downstaging. MR images obtained after radiation therapy with concomitant chemotherapy have (100%) sensitivity, (78.7%) specificity, (100%) NPV in the differentiation of T1–2/T3–4 tumors with MRI, accuracy 80.9% with agreement 70.58% and 100% accuracy for node staging.
Conclusion
High resolution pre treatment MRI of the rectum has a high predictive value of treatment outcome either for neoadjuvant treatment or surgery.
1 Introduction
Rectal cancer is associated with a high risk of metastases and local recurrence; local recurrence rates after surgical treatment being up to 32%.Citation1 Local recurrence is directly related to incomplete tumor resection Citation2,Citation3 and also related to the circumferential safety of resection.Citation4,Citation5 An accurate local staging at the time of initial diagnosis is therefore very important. Tumor depth of invasion staging, especially local staging (referred to as T assessment), determines the treatment strategy. This includes operation planning and the use of neoadjuvant therapy.Citation1 The total mesorectal excision, gives the best chance for tumor-free circumferential resection margin, and this will reduce the local recurrence rate.Citation4 Preoperative chemoradiation therapy has become the standard adjunctive preoperative treatment of patients especially in patients where there is a high likelihood of not achieving free surgical margin.Citation6 MRI has been shown to be highly accurate for local staging. As it was less operator dependent, it enabled evaluation of anal infiltration as well as the depth of extramural invasion. It could also be used to predict the circumferential resection margin.Citation7 The tumor-free total mesorectal excision reduces the frequency of pathologically involved margin of resection by tumor. This benefit should lead to reduced rates of local tumor recurrence and lower patient morbidity.Citation8
2 Materials and methods
This is a prospective study that includes 68 patients with biopsy-proven stage II or III rectal adenocarcinoma who received standardized 5-week chemo radiation therapy over a 2-year period (September 2010–December 2012). The indications for chemo radiation therapy were biopsy-proven locally advanced rectal cancer. In this regard, a locally advanced rectal cancer patient in our study was selected on the basis of either tumor fixation by digital rectal examination or clinical staging MRI findings of a high likelihood of circumferential resection margin involvement and hence possibility of inadequate immediate resection.
Of note, tumors were classified clinically as rectal if the lower limit was within 12 cm from the anal verge at sigmoidoscopy
| • | Informed consent was obtained from all patients after full explanation of the technique of MRI which is non invasive, without any risk approved till now. | ||||
| • | Privacy of all patients’ data is guaranteed. | ||||
Inclusion criteria: T3, T4 N0–3 adenocarcinoma rectal cancer patients.
Exclusion criteria: Early T1–2 and/or distant metastatic rectal adenocarcinoma.
2.1 Pre treatment evaluation
2.1.1 Clinical
Evaluation started with a complete history and accurate clinical examination including digital rectal examination and performance status (PS) of all patients according to ECOG PS scoring.
2.1.2 Laboratory
Base line and before surgery complete blood count, liver and renal function tests, electrolytes, tumor marker Carcino-embryonic antigen (CEA) and CA19.9 level were performed.
2.1.3 Radiologically
| • | Abdomino-pelvic ultrasound of all patients. | ||||
| • | Chest X-ray and/or computed tomography (CT) if needed to exclude pulmonary metastasis of all patients. | ||||
| • | Abdominal CT with contrast to exclude liver metastasis. | ||||
| • | Pelvic Magnetic Resonance Imaging (MRI): All cases underwent MRI examination in the Radio diagnosis Department (Tanta University) using a machine (GE signa 1.5 Tesla) with abdominal surface coil. All patients were positioned in the supine position. The following sequences are used, axial, sagittal and coronal T2WI. Axial cuts with fat saturated fast spin-echo T2WI and TIWI were obtained. Also axial, sagittal and coronal T1WI were taken immediately after a manual intravenous injection of 0.1 mg of Gd-DTPA/kg of body weight (Magnevist: Schering Berlin, Germany). Patients were asked to do breath-holding techniques to the extent tolerable. | ||||
2.1.4 Image analysis
MRI images were evaluated on a work station. Tumors were classified into two groups according to their anatomic location: low rectal tumors were diagnosed when less than 5 cm from the anal verge, upper and middle rectal tumors were diagnosed when more than 5 cm from the anal verge.
MR signal intensity of rectal mucosa and submucosa appear (inner hyperintense) followed by muscularis propria (appearing as hypointense intermediate layer). Then perirectal fat tissue (appearing as hyperintense layer), the mesorectal fascia appear as thin low intensity structure which envelops the mesorectum and the surrounding perirectal fat tissue. Also the extramesorectal lymph nodes were detected. The depth of the tumor invasion, the mesorectal infiltration, and number of enlarged lymph nodes were assessed. Mesorectal fascia was clearly delineated.
Each rectal tumor was staged according to the MRI findings and was later correlated with the operative and pathological findings. The depth of mural invasion by the tumor was staged according to the TNM staging system.Citation9
We characterized T1 tumors by an infiltration of the submucosal layer and a sparing of the muscularis propria. When the tumor invades muscularis propria we accepted the tumor as T2. T2 lesions were differentiated from T3 lesions by identification of a smooth outer tumor border within the rectal wall with no invasion into the fat surrounding the rectum. T3 lesions had irregular outer borders and invaded the fat surrounding the rectum either by a plaque, mass, or cordlike signal intensity that projected into the perirectal fat. The presence of spiculation within the fat alone was not sufficient evidence of an extramural invasion. In T4 lesions, fat planes between the rectal carcinoma and surrounding organs disappeared. Mesorectal fascia involvement and the invasion into adjacent organs were also noted as indicators of T4 tumors. Mesorectal and extramesorectal lymph nodes with irregular margins and/or a short axis greater than 5 mm were accepted as metastatic.Citation9
2.1.4 Treatment
Treatment is carried out in three Clinical Oncology centers: Tanta, Alexandria and Assiut. Radiation therapy for rectal cancer patients using Linear accelerator Photon 15 MeV Varian Medical Systems, Palo Alto, CA (United States) and Siemens Primus (German) Serial No. 3301; Radiotherapy dose consisted of a total of 5040 cGy delivered in 28 fractions of 180 cGy, five times a week, to the pelvis with individually shaped portals and the use of a four-field box technique. Concomitant chemotherapy used oral capecitabine (Xeloda)® 825 mg/m2 tablets twice daily throughout radiotherapy without interruption. Clinical and radiological restaging was performed 6 weeks after completion of preoperative treatment. Surgical resection either with anterior resection or abdomino-perineal resection was performed 6–8 weeks after completion of the chemo radiation therapy according to the principles of total mesorectal excision.
Patients were monitored for toxicity as radiation dermatitis, diarrhea and if needed were scored according to the National Cancer Institute Common Terminology Criteria for adverse Events (version 3.0).Citation8
2.2 Ethical approval
Ethical and record linkage approvals were obtained from the Human Research Ethics Committee at the University of Tanta and the Confidentiality of Health Information Committee of Tanta and from Human Researches Ethics Committee at Assiut University.
3 Result
Sixty-eight adenocarcinoma rectal cancer patients were included in the study (M:F = 48:20). The commonest clinical presentation was per-rectal bleeding (95.6%, n = 65). Preoperative MRI examination was performed. No treatment interruption occurred as no major toxicity occurred. All patients subsequently underwent operation. The mean time lag between the MRI study and operation was 16.8 days. 27 (39.71%) patients achieved a statistically significant partial response to concomitant radio chemotherapy and underwent low anterior resection and 41 (60.29%) patients abdomino-perineal resection + colostomy (P value 0.001∗∗) ().
Table 1 Correlation between disease response after induction concomitant radio chemotherapy and patient characteristics.
3.1 MRI down staging after induction radio-chemotherapy
After preoperative chemo-radiotherapy, there is a significant shift toward downstaging. 16/59 (23.5%) patients achieved down-staging by tumor (T) downsizing () and lymph node (N) downsizing () and from clinical stage III (before therapy) to stage II after therapy (P = 0.001)∗∗ () by achieving both.
Table 2 Rectal tumor (T) down staging after induction radio-chemotherapy by MRI.
Table 3 MRI lymph node (N) down staging after induction radio-chemotherapy.
Table 4 Rectal cancer downstaging after induction radio-chemotherapy by MRI.
The accuracy of pre-operative MRI versus pathological staging after either low anterior resection or abdomino-perineal resection:
Using Wilcoxon signed ranks test, there is a significantly strong correlation between histopathological and post MR images obtained after radiation therapy with concomitant chemotherapy in the differentiation of T2/T3 tumors (z = −4.472; P = 0.001∗∗).
When compared with pathological findings after surgical manipulation, MRI achieved 100% sensitivity, 78.7% specificity, 100% NPV, 80.9% accuracy with an agreement of 70.58% for rectal tumor (). MRI showed 100% accuracy for detection of node staging ().
Table 5 Correlation between histo-pathological and post chemo-radiotherapy MRI findings for rectal tumor (T) staging.
Table 6 Correlation between histo-pathological and post chemo-radiotherapy MRI findings for LN (N) staging.
3.1.1 Case number 1
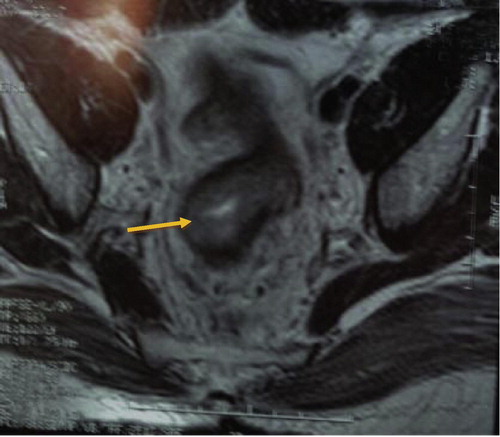
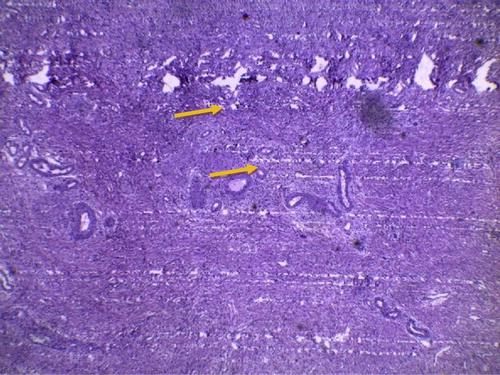
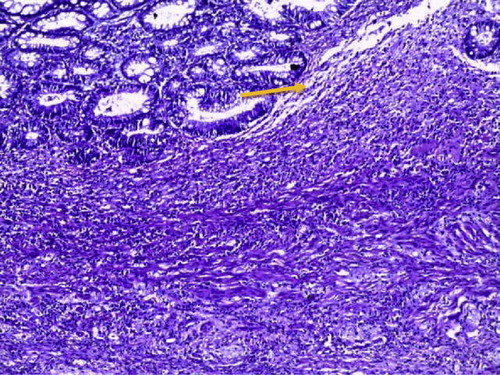
Female patient 60 years old presented by bleeding per rectum 2 months, Pre chemo-irradiation MRI (–) show antero-lateral aspect of lower rectum 6–9 O’clock rectal adenocarcinoma with loss of the muscularis propria and early infiltration of the adjacent mesorectal fat. Post therapy MRI shows regression course of rectal adenocarcinoma with down staging of early T3 → T1 ( and ) which correlates with post operative low anterior resection of pathological finding of the complete response () with no evidence of adenocarcinoma (100% accuracy).
Figure 1 Axial T2 MR cuts showing soft tissue mass of intermediate to high T2 signal intensity (S1) on the antero-lateral aspect of the lower rectum 9 O’clock (arrow) with loss of the muscularis propria and early infiltration of the adjacent mesorectal fat represent early T3.
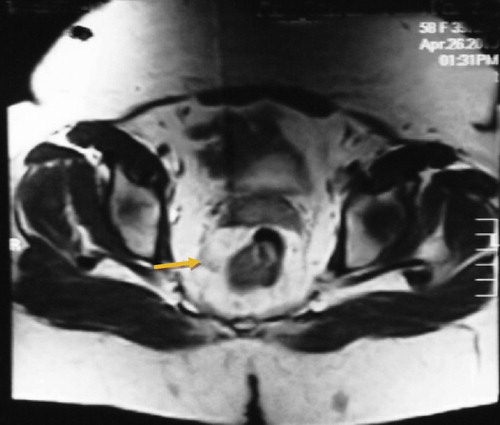
Figure 2 Axial T2 MR cuts showing soft tissue mass of intermediate to high T2 signal intensity (S1) on the antero-lateral aspect of lower rectum 6–9 O’clock (arrow) with loss of the muscularis propria and early infiltration of the adjacent mesorectal fat represent early T3.
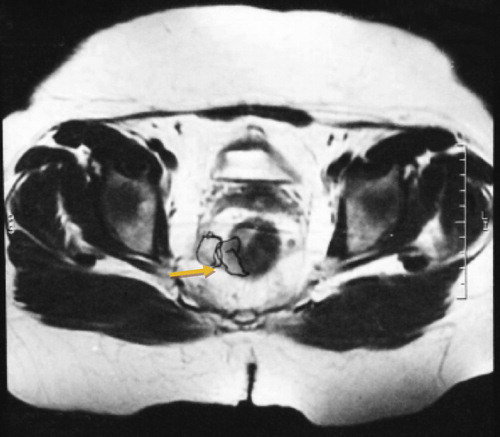
Figure 3 Coronal T2 MRI showing right lower third rectal mass about 2 cm from levator ani puborectalis insertion (arrow).

Figure 4 Axial MR sequence showing T1 soft tissue mass in the posterior right lateral rectal wall (arrow) with clear invasion into mesorectal fat.
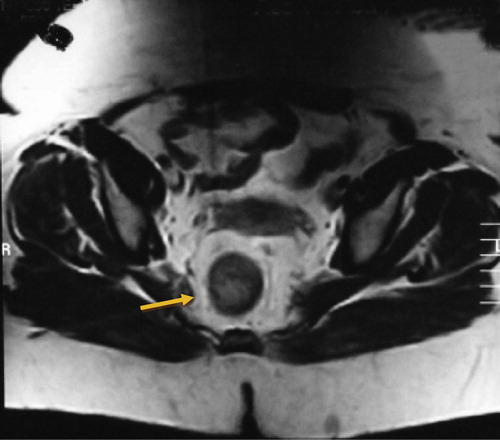
Figure 5 Coronal T2 MRI showing right lower third rectal mass 1 cm from levator ani puborectalis insertion (arrow).
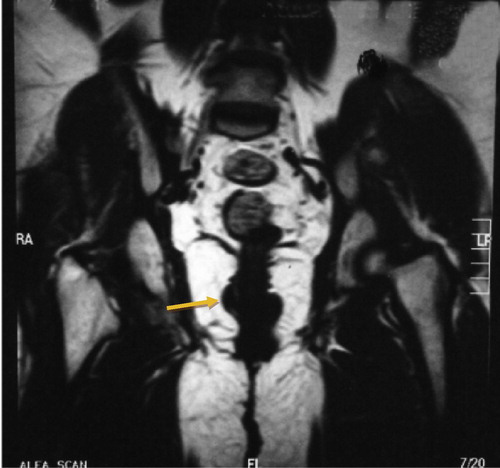
Figure 6 Histo pathological examination showing chronic non specific chemoradiotherapy induced proctitis showing transmural lymphoplasmacytic inflammatory infiltrate, glandular architectural atypia but with preserved mucin production (arrow). No granuloma & no malignancy include H&E X100 (100% agreement).
3.1.2 Case number 2
A male patient 38 years old presented with bleeding per rectum for 6 months. With alternation of bowel habits rectal adenocarcinoma is proved by punch biopsy before starting concurrent chemo-radiotherapy. Pre chemo-irradiation MRI shows circumferential wall thickening mainly at the ano-rectal junction and narrowing of the lumen T3 ().
Figure 7 Pre-therapeutic sagittal T2 MRI sequence show circumferential wall thickening mainly at the ano-rectal junction, narrowing the lumen.
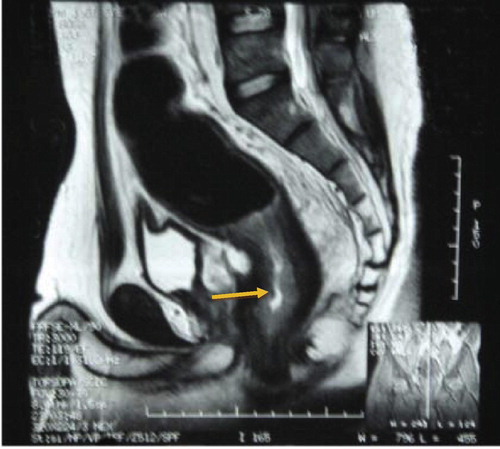
Post chemo-irradiation MRI shows stationary course of T3 rectal adenocarcinoma ( and ) which correlates with post operative abdomino-perineal resection pathological finding () of no response with evidence of adenocarcinoma (100% accuracy).
Figure 8 Post therapeutic sagittal T2 MRI examination of the ano-rectal junction showing slight regressive course of the previously detected mass (arrow).

4 Discussion
There are different modalities for diagnosis of rectal tumors including barium enema, and either colonoscopy or sigmoidoscopy. However these endoluminal techniques do not provide significant information about the extraluminal spread of the tumor needed for preoperative planning. Now several imaging methods have been used to assess the accurate spread of the tumor, such as endorectal ultrasound (EUS), computed tomography (CT) and MRI.Citation10
Many studies have reported that MRI shows excellent overall accuracies in the diagnosis of mesorectal fascia spread and invasion into adjacent organs (88−100% and 100%, respectively).Citation11–Citation13 However this high accuracy rate was not achieved either by EUS or multi detector CT.Citation14 Differentiation between T3 from T2 lesions is very important mainly for preoperative therapy, and the most important criterion is the invasion into perirectal fat. Early criteria for an assignment of pT3 in MRI are the absence of hypointensity of the muscle layer seen between the edge of the tumor and the extramural soft tissue.Citation15
Infiltration of tumor to the perirectal fat is the best indicator of T3 tumor on MRI images. However it is difficult to differentiate spiculation seen in the perirectal fat caused only by fibrosis from that spiculation caused by fibrosis containing tumor cells.Citation16
The mesorectal fascia that represents the CRM, and hence invasion into the CRM has a high recurrence rate.Citation17 In our work, neoadjuvant chemo-radiotherapy leads to down staging of the tumor in terms of its T and N stages as we investigated the MR accuracy obtained after radiation therapy with concomitant chemotherapy for the prediction of down staging of tumors confined to the rectal wall T3–4/T1–2 by using histopathologic findings (ypT3/T1–2 lesions) as the reference standard in patients with cancerous rectum. After preoperative chemo radiotherapy there is a significant shift toward earlier TNM stages with significant down-staging from stage III before therapy to stage II after therapy (P value = 0.001). MR images obtained after concomitant chemo-irradiation have 100% sensitivity, 78.7% specificity, 100% NPV for the prediction of tumor downsizing to a ypT0–2 lesion with accuracy 80.9%. This result agrees with that of WilliamsonCitation18 and Chari.Citation19
In our study MRI shows 100% accuracy in the differentiation of N0/N1–2 tumors (z = −4.472; P = 0.001) with sensitivity 100%, specificity 100% () with agreement 70.58%. This concords with Beets-Tan and colleagues who investigated 76 patients and found preoperative MRI to be accurate in the assessment of CRM. The agreement is 100% in T4 tumors, and 97% and 93% for both readers in tumors with a histologically determined tumor-free CRM >10 mm.Citation10,Citation11 The low accuracy of MR imaging in these studies could be explained by the low spatial resolution that was used with early MRI techniques in 2001. But even with higher spatial resolutions in the new generation of phased-array coils, the accuracy for T staging was not as high as expected, with values varying between 65% and 86%.Citation11,Citation20–Citation22
One exception to the above was the study done by Brown and colleaguesCitation6 who reported 100% accuracy and complete agreement between two readers on the diagnosis of tumor stage with MR imaging results. The most difficult staging with MR imaging occurs in the differentiation of T2-stage and borderline T3-stage lesions. This is mainly due to the over-staging of the tumor. Over-staging is caused mainly by desmoplastic reactions.Citation6,Citation11,Citation22 In our work there is strong correlation between histopathological and post MRI tumor staging in the differentiation of T2/T3 (Z = 472; P = 0.001) and also in the differentiation of N1/N2 (Z = 472; P = 0.001). This is in concordance with Minsky and others in 1995 as MRI and histology for T staging have ranged from 66% to 94%. The main difficulty with MRI has been the differentiation between two stages T2 and T3. However, the definitive treatment being the same for both these stages, this means the differentiation does not play a huge impact on patient outcome.Citation23
On the other hand, in a study Bissett and his colleague reported good agreement between preoperative MRI and histopathology as regards tumor invasion detection through the mesorectal fascia with an high accuracy of 95%.Citation24 The exact staging is very important because the number of metastatic nodes has been shown to affect the prognosis of the disease.Citation25 Lymph node involvement in the vicinity of the mesorectal fascia is associated with a higher risk of local recurrence,Citation2 and therefore the accuracy in the detection of lymph nodes is essential for accurate treatment. Patients with metastatic lymph nodes outside the mesorectal fascia need extended lymph node resection with removal of the internal iliac lymph nodes.Citation11 This group of lymph node is not removed when TME is done.
Nodal staging by MRI usually depends on the size criteria. Typically a lymph node is considered malignant when the short axis of the lymph node measures over 0.5 cm.Citation26 Also the lymph node features such as ill defined edges, dissimilarity of signal enhancement within the node increase the accuracy of MRI.Citation27 This can explain achieving 100% accuracy in our study. The disappointing accuracy seen in MRI imaging in staging rectal cancer is due to both overstaging and under-staging. Over staging, in the assessment of invasion into the rectal wall, occurs because after radiotherapy the responding tumors are replaced by fibrosis, inflammatory and vascular proliferation.Citation28 Promising strategies of imaging using lymph node specific paramagnetic nano particles have been reported to increase the accuracy in the detection of micro metastasis.Citation29
5 Conclusion
MRI plays an important role in the multimodality imaging used in the treatment of patients with cancerous rectum. Accurate preoperative staging is very important for making effective therapeutic decisions. MRI accurately delineates the extent of primary tumor. Regarding the depth of tumor invasion these give effective decisions for patient treatment.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 4 December 2014
References
- P.M.SagarJ.H.PembertonSurgical management of locally recurrent rectal cancerBr J Surg831996293304
- I.J.AdamM.O.MohamdeeI.G.MartinRole of circumferential margin involvement in the local recurrence of rectal cancerLancet3441994707711
- P.QuirkeP.DurdeyM.F.DixonN.S.WilliamsLocal recurrence of rectal adenocarcinoma due to inadequate surgical resection: histopathological study of lateral tumor spread and surgical excisionLancet21986996999
- R.J.HealdR.D.H.RyallRecurrence and survival after total mesorectal excision for rectal cancerLancet1198614791482
- J.V.ReynoldsW.P.JoyceJ.DolanK.SheahanJ.M.HylandPathological evidence in support of total mesorectal excision in the management of rectal cancerBr J Surg83199611121115
- G.BrownC.J.RichardsR.G.NewcombeRectal carcinoma: thin-section MR imaging for staging in 28 patientsRadiology2111999215222
- MERCURY Study GroupExtramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY studyRadiology2432007132139
- A.TrottiDevelopment of comprehensive grading system for the adverse effects of cancer treatmentSemin Radiat Oncol1332003 July176181
- L.SobinC.WittekindTNM classification of malignant tumors5th ed.1997WileyNew York, NY 227
- R.G.Beets-TanG.L.BeetsRectal cancer: review with emphasis on MR imagingRadiology2322004335346
- R.G.Beets-TanG.L.BeetsR.F.VliegenAccuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgeryLancet3572001497504
- G.BrownA.G.RadcliffeR.G.NewcombePreoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imagingBr J Surg902003355364
- T.AkasuG.IinumaM.TakawaAccuracy of high-resolution magnetic resonance imaging in preoperative staging of rectal cancerAnn Surg Oncol16200927872794
- S.BipatA.S.GlasF.J.SlorsRectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging a meta-analysisRadiology2322004773783
- S.X.RaoM.S.ZengJ.M.XuAssessment of T staging and mesorectal fascia status using high-resolution MRI in rectal cancer with rectal distentionWorld J Gastroenterol13200741414146
- G.BrownC.J.RichardsR.G.NewcombeRectal carcinoma: thin-section MR imaging for staging in 28 patientsRadiology2111999215222
- G.BrownS.DaviesG.T.WilliamsEffectiveness of preoperative staging in rectal cancer: digital rectal examination, endoluminal ultrasound or magnetic resonance imaging?Br J Cancer9120042329
- P.R.WilliamsonM.D.HellingerS.W.LarachA.FerraraEndorectal ultrasound of T3 and T4 rectal cancers after preoperative chemoradiationDis Colon Rectum39119964549
- R.S.ChariD.S.TylerM.S.AnscherPreoperative radiation and chemotherapy in the treatment of adenocarcinoma of the rectumAnn Surg22161995778786 [discussion 786–777]
- L.BlomqvistM.MachadoC.RubioRectal tumor staging: MR imaging using phased-array and endorectal coils vs endoscopic ultrasonographyEur Radiol102000653660
- G.GagliardiS.BayarR.SmithR.R.SalemPreoperative staging of rectal cancer using magnetic resonance imaging with external phase-arrayed coilsArch Surg1372002447451
- T.J.VoglW.PegiosM.G.MackAccuracy of staging rectal tumors with contrast-enhanced transrectal MR imagingAJR Am J Roentgenol168199714271434
- B.D.MinskyConservative treatment of rectal cancer with local excision and postoperative radiation therapyEur J Cancer31A7–8199513431346
- I.P.BissettC.C.FernandoD.M.HoughIdentification of the fascia propria by magnetic resonance imaging and its relevance to preoperative assessment of rectal cancerDis Colon Rectum4422001259265
- R.TangJ.Y.WangJ.S.ChenSurvival impact of lymph node metastasis in TNM stage III carcinoma of the colon and rectumJ Am Coll Surg18061995705712
- J.BeynonN.J.MortensenD.M.FoyJ.L.ChannerH.RigbyJ.VirjeePreoperative assessment of mesorectal lymph node involvement in rectal cancerBr J Surg761989276279
- D.J.KimJ.H.KimY.H.RyuT.J.JeonJ.S.YuJ.J.ChungNodal staging of rectal cancer: high-resolution pelvic MRI versus 18F-FDGPET/CTJ Comput Assist Tomogr352011531534
- D.J.KimJ.H.KimJ.S.LimJ.S.YuJ.J.ChungM.J.KimRestaging of rectal cancer with MR imaging after concurrent chemotherapy and radiation therapyRadiographics302010503516
- O.WillS.PurkayasthaC.ChanT.AthanasiouA.W.DarziW.GedroycDiagnostic precision of nanoparticle enhanced MRI for lymph-node metastases: a meta-analysisLancet Oncol720065260