?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
It is clear that triple-negative breast cancer (TNBC) tumors are heterogeneous group, but clinically important sub-sets have begun to emerge. We investigate the immunohistochemical expression of androgen receptor (AR) among those hormonal insensitive groups which have only the option of chemotherapy. Exploiting this knowledge for therapy has been challenging.
Patients & methods
Seventy seven patients with TNBC subtype, treated from January 2009 until February 2011 were evaluated for AR expression where AR-positive expression group (⩾10% nuclear stained cells) was conducted to receive anti-androgen therapy post adjuvant chemotherapy (Bicalutamide “Casodex®”) 50 mg, once daily with or without meals at the same time each day, to date. AR expression was correlated with other prognostic factors and survival (disease free survival (DFS) and overall survival (OS)). Cox proportional hazard model was used to assess variables in the multivariate analysis.
Results
The median age in the present study was 35.6 year (19–63 years). The median follow-up period was 24 months (3–60 months). AR-positive expression in the present study was (2177) 27.27% correlated with clinical outcomes, for recurrent event (n = 4, 19.05%), (P = 0.000, HR 12.750, Cl 95% 3.668–44.318) and for death event, no body died in AR positive expression group (P = 0.000, HR 0.644, Cl 95% 0.533–0.779). Improved survival with AR-positive expression group for 2-year and 3-year DFS was 85% and 78% respectively with (P = <0.001, Cl 95% 39.17–51.39) and for OS at 2-year and 3-year was 100% (P = 0.0005). In univariate and multivariate analysis, AR positive expression with anti-androgen therapy in TNBC patients in our present study had retained their independent prognostic value for DFS (P = 0.0006, HR 4.659, Cl 95% 1.553–13.977). Bicalutamide was well-tolerated therapy with no grade 3/4 treatment-related adverse events.
Conclusions
Bicalumide is well tolerated in AR positive TNBC subtype patients and could offer an alternative to cytotoxic chemotherapy in those patients with better OS and DFS.
1 Introduction
Androgen receptor (AR) positivity has been detected in approximately half of all breast carcinoma cases.Citation1,Citation2 High (AR) expression in breast cancer has been correlated with a low risk of recurrence and death.Citation1
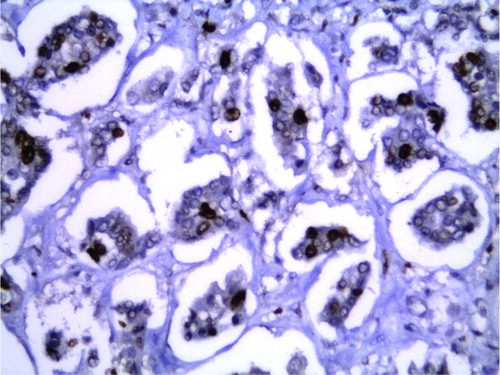
Figure 5a A case of invasive ductal carcinoma grade III showing negative immunohistochemical stain for estrogen receptor [Streptavidin biotin × 400].
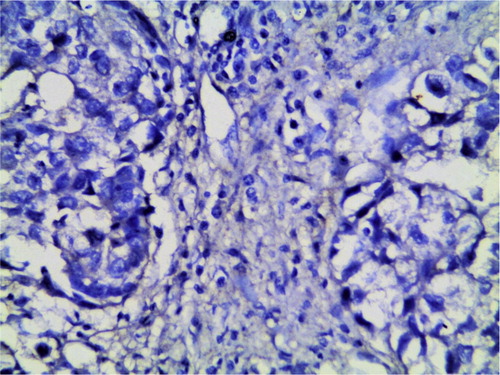
Figure 5b The same case of invasive ductal carcinoma grade III showing negative immunohistochemical stain for progesterone receptor [Streptavidin biotin × 400].
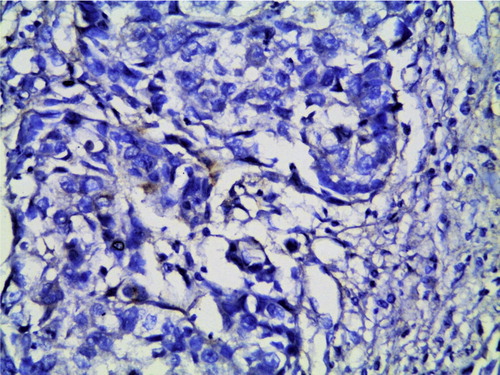
Figure 5c The same case of invasive ductal carcinoma grade III showing negative immunohistochemical stain for HER-2 receptors [Streptavidin biotin × 400].
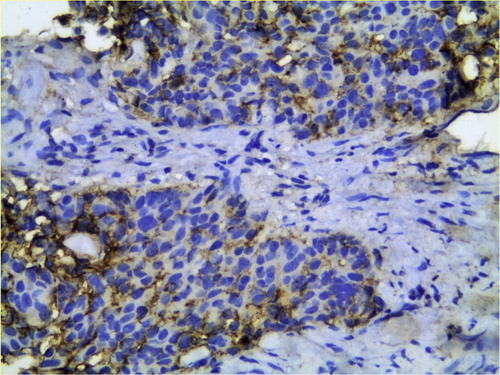
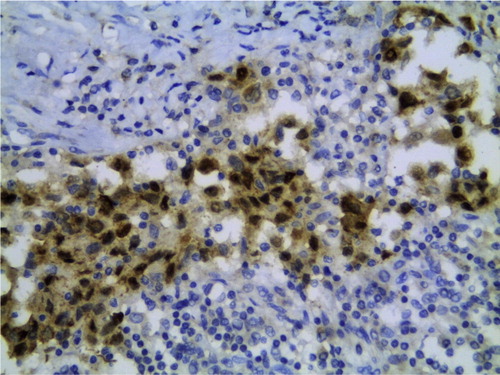
Figure 5d The same case of invasive ductal carcinoma grade III showing positive immunohistochemical stain for androgen receptors in more than 10% of the tumor cells [Streptavidin biotin × 400].
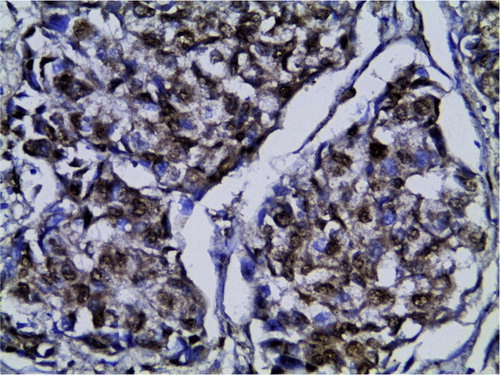
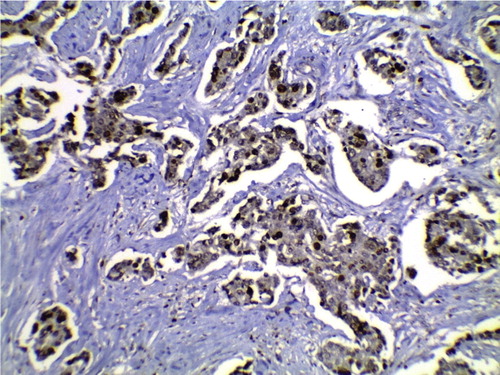
Figure 7 A case of invasive breast carcinoma grade II showing positive immunohistochemical stain for androgen receptors in more than 10% of the tumor cells [Streptavidin biotin × 100].
AR has been shown to have prognostic implications in breast carcinoma, and higher AR expression levels have been associated with older age at diagnosis, higher expression of ER or PR, lower nuclear grades, and smaller tumor size.Citation2,Citation3
Triple-negative breast cancers (TNBC) were recently divided into further subtypes including a subtype with high AR expression.Citation4
Previous studies looking at AR expression in TNBC have demonstrated that AR negativity has been associated with a shorter disease-free interval and overall survival than AR-positive TN cancer. These studies suggest that AR expression could be a useful prognostic marker in TN tumors.Citation4
AR is expressed in 60–70% of breast tumors independent of estrogen status, and in 20–32% of TNBC patients. Estrogen and Progesterone and the gene HER-2, these are the three big markers and/or targets in breast cancer. Evidence presented at the AACR Annual Meeting 2013 adds a fourth: androgen receptors.Citation5
2 Patients and methods
This Retrospective study was conducted in Clinical Oncology Department and Histopathological Department, Tanta University 2009 until February 2011. The study included 77 consecutively treated patients with TNBC. The established clinical and histo-morphological factors of all patients were assessed. The steroid hormones status including (ER, PR, Her.2, AR and KI-67) was evaluated by immunohistochemistry (IHC).
The aim of this study focused on predictive and prognostic value of AR expression as a hormonal marker in TNBC patients.
2.1 Immunohistochemistry for ER, PR, HER-2, AR and KI-67
For immune-staining, 3–5 mm sections were deparaffinized with 40 min incubation at 60_C and subsequent immersion in xylene, and were rehydrated in solutions of decreasing ethanol. Then specimens were incubated in 0.3% H2O2 for 30 min to inhibit activation of endogenous peroxidases. Slides were then washed with phosphate-buffered saline (PBS) and heated in an 830-W microwave oven for at least 15 min in 10 mmol/l sodium citrate buffer (pH 6.0) for antigen retrieval. Sections were incubated with primary antibodies against [mouse monoclonal, androgen receptors (ab9474 1:500 dilution), rabbit monoclonal Estrogen receptor (ab37438 1:25 dilution), rabbit monoclonal Progesterone receptor (ab2765 1:25 dilution), rabbit monoclonal HER-2 receptor (ab134182 1:100 dilution) and Rabbit polyclonal KI-67 (ab15580 1:100 dilution) overnight at 4_C. For the negative control, the primary antibody was replaced with phosphate buffered saline (PBS). Rabbit anti-mouse horseradish peroxidase-conjugated secondary antibody was added followed by incubation for 40 min at room temperature. The color was developed using diaminobenzidine (DAB) as a chromogen. Slides were extensively washed with PBS after each step. Finally they were counter-stained with Mayer’s hematoxylin.
The immunostaining results for ER, PR & AR were assessed semiquantitatively and reported as positive if more than 10% of cells have nuclear immunostaining in a tumor. Tumor cells were considered positive for HER2 protein overexpression when more than 10% of the cells showed complete moderate or strong membrane staining. Ki 67 immunostaining was considered positive if there were nuclear staining in more than 10% of the tumor cells.Citation6
2.1.1 Study design
Seventy seven TNBC patients were classified into two sub-groups according to AR-expression profile, where AR-positive expression group 21/77 (27.27%) designated to receive anti-androgen therapy post adjuvant traditional chemotherapy, Bicalutamid 50 mg once daily with or without meals at the same time each day still received to date.
At the time of primary treatment, none of the patients had any evidence of distant metastases. After the completion of the primary treatment, our TNBC patients underwent regular follow-up examinations at our department for DFS and OS as regards AR expression profile. All the procedures were in accordance with the ethical standards of our faculty’s Ethical committee.
2.1.2 Statistical analysis
Statistical presentation and analysis of the present study were conducted, using Number and percentage for qualitative and tested by chi-square test. We used Kaplan–Meier and Cox regression for survival analysis by SPSS for windows version 18.0 software package (SPSS Inc., Chicago, 11) and P value = <0.05%. Overall survival (OS) defined the length of time from the date of diagnosis and the patients still alive either free or not. Disease-free survival (DFS) expresses the period after curative treatment (disease eliminated) when no disease can be detected.
3 Results
At the time of the primary treatment, none of the patients had any evidence of distant metastases.
The tumor’s, patient’s and treatment’s characteristics in 77 TNBC patients are presented in , the median age of the patients was 35.6 years (range, 19–63). Age >35 years was 50.65%, premenopausal at the presentation was 52.63%, patients had grade III tumors 32.47%, tumor size larger than 2 cm was 27.27%, and patients had invasive ducal carcinoma (IDC) (92.21%). At least one axillary lymph node was positive in 57.14% of patients, and positive mitotic index was 67.53%. In twenty one patients (21/77) 27.27% were positive for AR expression in TNBC patients in the present study. Positive AR immunostaining was inversely correlated with large tumor size (P = 0.001), nodal status (P = 0.007), high grade (p = 0.000) and higher Ki67 (p = 0.08). Positive AR expression was associated with age less than 35 years (42.86%), female patients (100%), premenopausal status (42.86%) and no patients had stage III at presentation. For AR negatively expressed tumors in TNBC patients in the present study 51.79% was associated with age <35, 3 male patients (5.36%), premenopausal status (56.36%). Stage III at presentation was 41.07%, 35.7% presented as T3, N2 in 21.43%, 92.86% presented with IDC histology subtype, GIII in 42.86%, high CA15.3 in 32.14% of patients and 73.21% presented with high KI-67 more than 14%. All patients underwent the radical local treatment, all patients of this study received anthracycline-based chemotherapy regimens A/C (Adriamycin and cyclophosphamide), T/A (Taxol and adriamycin)
Table 1 Tumor’s and treatment’s characteristics in 77 TNBC patients.
3.1 Follow-up
Local and distant recurrences were 59.74% (n = 46) of patients and 23.38% (n = 18) patients were died in the whole studied population of TNBC ().
Table 2 Clinical outcomes in 77 TNBC patients.
The median follow-up was 24 months (range, 3–60) months. Ten (12.99%) patients experienced local recurrence, 45 (58.44%) patients experienced distant recurrence and 18 (23.38%) patients were died, in the entire study (). The risk of relapse (local spread) in AR-positive group (n = 1, 4.76%) versus (N = 9, 16.07%) in AR-negative group with p value = 0.15, for distal spread (n = 3, 14.28%) versus (n = 42, 75.00%) for AR-Positive and AR-negative groups respectively, (p = 0.000). AR-expression was positively associated with clinical outcomes for recurrent event (n = 4, 19.05% versus n = 42, 75%), AR-Positive and negative groups respectively (P = 0.000, HR = 12.750, 95 Cl% 3.668, 44.318), for death event nobody died in AR positive group in comparison with (n = 18, 32.9%) for AR-negative group (P = 0.000, HR 0.644, Cl 95% 0.533–0.739) .
Table 3 Correlation of different prognostic factors with AR expression (AR+ve versus AR-ve groups).
Table 4 Relation of AR-expression and clinical outcomes.
3.2 Survival plots
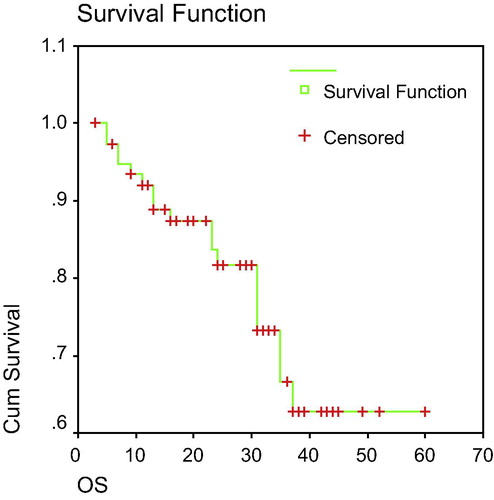
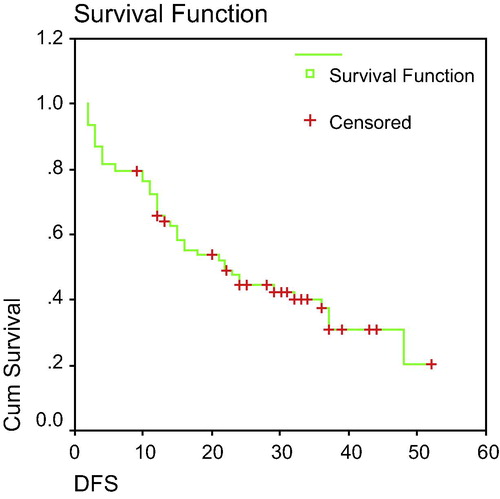
The median overall-survival (OS) of the entire group was 46.58 months with 5-Year OS 63% (). Median disease-free-survival (DFS) was 22.00 months with 5-year DFS 18% and in the entire group we found a pattern of maximum recurrence and death rates in the first 3 years following the diagnosis and a clear decline after that ().
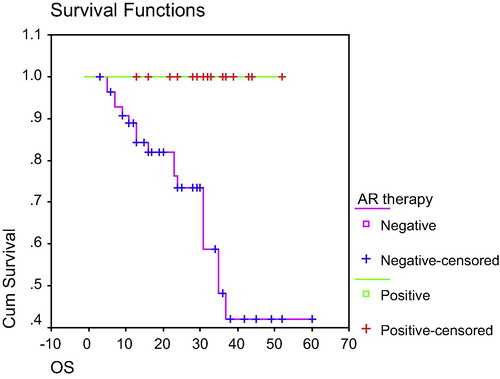
The median OS, was 35 months for AR-ve group with no death in AR positive group received anti-androgen therapy; 2-year OS was 100% versus 74%, 3-year OS was 100% versus 42% and 5-year OS was 100% versus 42% for AR-positive and AR-negative groups respectively (P = 0.0005) “”.
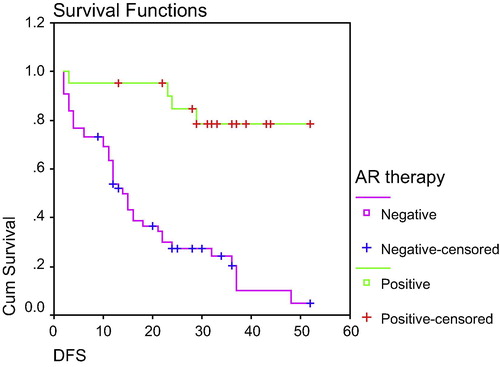
The median DFS was 45.26 months versus 14.00 in AR-positive with anti-androgen therapy and AR-negative groups respectively with (P = 0.000). 2-Year DFS was 85% versus 28%, 3-year DFS was 78% versus 20% and 78% versus 5% at 5-year DFS (p = <0.001), for AR + positive and AR-negative groups respectively “”.
3.3 Univariate and multivariate survival analysis
In the univariate analysis (), AR expression was positively associated with nodal status, grade, Ki67 and CA 15.3 with significant impact on DFS (P = 0.001, 0.043, <0.001, 0.003). In the multivariate analysis () for DFS, only AR expression group which received anti-androgen therapy, tumor grade and ki-67 proliferation index retained their in-dependent prognostic and predictive values in TNBC patients (P = 0006, HR 4.659, CI 95% 1.553–13.977): for AR expression, (P = 0.000, HR 4.105, CI 95% 2.065–8.159), for tumor grade, and (P = 0.000, HR 0.281, CI 95% 0.119–0.665) for Ki-67.
Table 5 Univariate analysis of the entire group for our study (77 patients) TNBC of different prognostic factors as regard DFS.
Table 6 Multivariate analysis of the entire group for significant prognostic factors as regard DFS.
3.4 Toxicity profile for anti-androgen therapy
As regarded Bicalutamide toxicity profile, no patient presented with grade 3/4 toxicity, only 621 patients, 28.57% presented with breast tenderness of fullness and hot flushes (n = 2), Feeling sick (nausea) (n = 3), weight gain (n = 1) and all of them controlled, Bicalutamid still received as hormonal therapy to date among AR-positively expressed subtype in the present study.
4 Discussion
To date, studies on patients with TNBC have been limited mostly by the small sample sizes and short follow-up times. Our present retrospective study was conducted in 77 TNBC patients treated in the routine clinical practice with the median follow-up time of almost 24 months.
In the study, TNBC patients had relatively large tumors at presentation (more than 2 cm in 27.27% of patients), pre-menopausal (52.63%), predominant type of tumor was invasive ductal carcinoma (92.21%), poorly differentiated (32.47%), positive ki-67 > 14% (67.53%), almost more than half of patients (57.14%) had positive axillary lymph nodes and twenty-one patients (27.27%) were positive for AR expression at presentation (). Also, in some previous reports triple-negative tumors were presented in premenopausal young women with poorer clinical outcomes similar to our results, median DFS was 4 years among women who were diagnosed between age 31–40 years compared with 8 years among women diagnosed at age 60 or older (7). TNBC tumors were described as relatively large (>2 cm) with high rate of node positivityCitation7–Citation15 similar to our results. Other investigators found that characteristically TNBC exhibits an invasive ductal histology and a high histologic grade, presented with high mitotic index.Citation16–Citation18 In the population based Carolina Breast Cancer Study (CBCS), basal like breast cancers (defined by triple negative status plus EGFR and/or cytokeratin 5 positivity) were virtually all of ductal or mixed histology 90% and of high grade (84%), whereas TNBC is identified tumor subtype characterized by aggressive behavior and poor prognosis where the majority of triple-negative cases were of high grade and of large tumor sizeCitation19–Citation24 similar to our results. TNBC cases are associated with higher expression of ki-67 than non-TNBC and so ki-67 can be used for further classification of TNBC into two subtypes with different response and prognosis.Citation25–Citation27 Garay et.al.Citation28 stated that AR was expressed in 10–35% of TNBC patients and also, stated by RicherCitation5 (5. Traditionally, chemotherapy has been the mainstay of systemic treatment for TNBC, TNBC is highly responsive to primary anthracycline and anthracycline/taxane protocols, however, a high risk of relapse remainsCitation29–Citation31 similar to our study).
AR expression was significantly related to older age at diagnosis, smaller tumor size, well differentiated tumors, lower proliferative index, lack of lymph node metastasis and of ductal type.Citation8,Citation17,Citation32–Citation38
TNBC patients with androgen negative have a higher proportion of positive lymph nodes,Citation3 higher level of pre-operative CA15.3, larger tumor size, higher grade.Citation19,Citation39,Citation40 It has been documented that AR expression is related to positive prognostic factors.Citation8,Citation33,Citation38,Citation41
Correlation between histopathologic grade and the expression of all sex hormone receptors in breast tumors revealed that as tumor grade progressed from 1 to 3 AR-expression decreased from 95% to 76% in ductal carcinoma in situ (DCIS) and 88–47% in invasive carcinoma. In the same analysis, ER expression decreased from 100% to 8% in DCIS and to 9.5% in invasive carcinoma with increasing tumor grade.Citation28
In our study as a whole, the median follow-up was 24 months (range, 3–60) where 12.99% of patients experienced local recurrences, 58.44% of patients experienced distal recurrence and 23.38% of patients died. Two-year OS was 82% and 67% for 3-year OS, as regards DFS in the whole study 2-year DFS was 46% and 31% for 3-year DFS. Pattern of metastasis was 25.97%, 24.68%, 7.79% and 7.79% for lung, brain, liver and bone respectively. Other investigators agreed with us where TNBC was reported to have higher rate of recurrences and decreased overall survival.Citation4,Citation8,Citation27,Citation37,Citation42–Citation44
Albergaria et al.Citation10 suggested that there was a significant association of tumor size, histologic grade and lymph node status to high scores of NPI (Nottingham prognostic index) in TNBC. In terms of survival there is a sharp decrease in survival during the first 3–5 years after diagnosis but distant after that time is much less common.Citation11,Citation23,Citation31,Citation45–Citation48 In a study published by Dent et al.Citation48 the median time to death was 3.5 years for TNBC compared to 5.7 years for patients with other cancers. In fact, as we can infer by the survival functions, TNBC experienced a severe decrease in their outcomes before 48 months as seen in their overall survival curves.Citation10,Citation49 The prognosis of women with TNBC is significantly poor, compared to women with other subtypes of breast cancer, and the underlying differences in recurrence and patient mortality rates may be explained in part by different routes of metastatic spread. The current theory points out the suggestion that TNBC metastasizes to axillary bones less frequently than the non-triple negative subset of breast tumors, favoring a hematogenous spreadCitation16,Citation23,Citation45 similar to our results.
Mohamed et al.Citation19 showed that TNBC is identified tumor subtypes characterized by aggressive behavior and poor prognosis. TN phenotype was associated with high microvessel invasion. The majority of TN cases were of high grade and of large size with biologically heterogeneous group of tumors where expression of basal markers with vascular invasion was 26%, preferable metastatic dissemination sites were visceral like brain, lung and liver and less to the bone (40% lung, 30% brain, 20% liver and 10% bone) in agreement with our results, with 3-year OS with complete pathological remission 94% dropped to 68% in patients with less than complete pathological remission after primary chemotherapy.Citation11,Citation31,Citation44,Citation47
In the present study, Androgen receptor-positive expression TNBC tumors which received anti-androgen therapy with tolerable toxicities, showed favorable clinical outcomes in comparison with negatively AR expressed tumors, with 4.76% local spread and 14.28% distal spread. For recurrent event 19.05% and for death event nobody died in AR-positively expressed group of TNBC patients. The median DFS was 45.26 months versus 14.00 months in AR-positive and AR-negative groups respectively, 2-year DFS was 85% versus 28%, 3-year DFS was 78% versus 20% for AR-positive and negative groups, respectively. As regards 2-year OS was 100% versus 74% and 3-year OS was 100% versus 42% for AR positive versus AR-negative groups respectively.
AR-dependent cell cycle progression is a critical regulator of the G1-S transition in prostatic carcinoma, and a similar role may be envisaged in breast cancer.Citation41 The sensitivity and specificity and likelihood ratio of AR for therapeutic response were higher relatively to other markers, individually and also in combination. AR expression showed inverse correlation with EGFR, and loss of EGFR would lead to suppression of cell growth and consequently would result in better therapeutic response.Citation41 Because AR ligands can have opposing and paradoxical effects in various breast cancer cell lines expressing AR, applying AR-targeted therapies for breast cancer treatment has been challenging.Citation28,Citation32,Citation37,Citation49
Thike et al.Citation40 suggest that loss of AR in TNBC augurs a worse prognosis and predicts early recurrence in TN and basal like breast cancer. DFS was significant in AR-positive TNBC with trend to improve OS was noted within 5 years of diagnosis, and also, other investigatorsCitation28,Citation31,Citation33,Citation50–Citation53 stated a significant correlation between AR expression and DFS and OS, similar to our results in AR expression group which received anti-androgen targeted therapy (Bicalutamide, (casodex) where the prognostic marker give a sufficient level of evidence in this subgroup).Citation4,Citation28,Citation54–Citation62
In the present study, the univariate analysis and the multivariate analysis retained the significant prognostic value of AR expression with positive impact on DFS and OS in TNBC patients. This is in agreement with many researchers.Citation5,Citation28,Citation31,Citation51
In conclusions, it is apparent that AR inhibition can stabilize disease in TNBC patients. Bicalumide is well tolerated in AR positive patients and could offer an alternative to cytotoxic chemotherapy in those patients. TNBC needs for a paradigm shift in personalized treatment than one size fits all.
Conflict of interest
There was no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 30 October 2015
References
- S.LoiblB.M.MullerG.von MinckwitzAndrogen receptor expression in primary breast cancer and its predictive and prognostic value in patients treated with neoadjuvant chemotherapyBreast Cancer Res Treat1302011477487
- S.ParkJ.S.KooM.S.KimAndrogen receptor expression is significantly associated with better outcomes in estrogen receptor-positive breast cancersAnn Oncol22201117551762
- R.HuS.DawoodM.D.HolmesAndrogen receptor expression and breast cancer survival in postmenopausal womenClin Cancer Res17201118671874
- J.HeR.PengZ.YuanPrognostic value of androgen receptor expression in operable triple-negative breast cancer: a retrospective analysis based on a tissue microarrayMed Oncol292012406410
- Jennifer Richer. Androgen receptors found to be a potential target in Breast cancer. AACR news: studies show increasing evidence that androgen drives breast cancer. AACR Annual Meeting 2013. University of Colorado Denver.
- R.M.TamimiH.J.BaerJ.MarottiM.GalanL.GalaburdaY.FuComparison of molecular phenotypes of ductal carcinoma in situ and invasive breast cancerBreast Cancer Res102008R67
- S.BudveD.J.DabbsS.J.SchnittBasal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pahologists and oncologistsMod Pathol2422011157167
- E.A.RakhaM.E.El-sayedA.R.GreenPrognostic makers in triple-negative breast cancerCancer109120072532
- Diazlkv.l.CrysW.F.SymmansTriple negative breast carcinoma and the basal phenotype: from expression profiling to clinical practiceAdr Anat Pathol1462007419430
- AlbergariaAndreRicardoSaraMilaneziFernandaNottingham prognostic index in triple-negative breast cancer: a reliable prognostic tool?BMC Cancer112011299
- R.DentM.TrudeauK1PritchardTriple-negative breast cancer: clinical features and patterns of recurrenceClin Cancer Res13IS200744294434
- X.R.YangM.E.ShermanD.L.RimmDifferences in risk factors for breast cancer molecular subtypes in a population based study-cancerEpidermiol Biomarkers, Prev1632007439443
- K.R.BauerM.BrownR.D.CressDescriptive analysis of estrogen receptor ER-negative, progesterone receptor (PR)-negative and HER 2-negative invasive breast cancer, the so-called triple-negative phenotype: a population based study from the California cancer registryCancer1099200717211728
- F.M.BlowsK.E.DriverM.K.SchmidtSubtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studiesPlots Med7s20101000279
- Amal AbdEl-HafezAbdEl-MageedMohamed Abd-El-atyShawkyDifferent prognostic factors correlate with BCL-2-expression among triple negative and non-triple negative BCAsian Pacific J Cancer Prev1420131041
- Doreen CBrady-WestDonovan AMcGrowderTriple negative breast cancer, therapeutic and prognostic implicationsAsian Pacific J Cancer. Prevention12201121392143
- V.Kuenen-BoumeesterH.vander kwastC.C.Cleas senThe clinical significant of androgen receptor in breast cancer and their relation to histological and cell biological parametersEur J Cancer1996 32A-1560-156s
- G.VialeS.Z.N.RotmenP.MaisonneuveInfiltrating ductal carcinoma of the breast with TNBC phenotype: prognostic implications of EGFR immunoreactivityBreast Cancer Res Treat1162009317328
- Rabab A.A.MohammedIan O.EllisAli M.MohmmodLymphatic and blood vessels in basal and triple-negative breast cancers: characteristics and prognostic significanceModern Pathol242011774785
- E.A.RakhaS.E.ElsheikhM.A.AleskandaranyTriple-negative breast cancer: distinguishing between basal and non basal subtypesClin Cancer Res15200923022310
- A.A.LuckA.J.EvansA.R.GreenThe influence of basal phenotype on the metastatic pattern of breast cancerClin Oncol (R Coll Radiol)2020084045
- S.M.Rodriguez-PinillaD.SarrioE.HonradoPrognostic significance of basal-like phenotype and fascin expression in node-negative invasive breast carcinomasClin Cancer Res12200615331539
- L.G.FulfordJ.S.Reis FilhoK.RyderBasal-like grade III invasive ductal carcinoma of the breast: patterns of metastasis and long-term survivalBreast Cancer Res92007R4
- ChoccalingamChidambharamRaoLakshmiRaoSrutiClinico-pathological characteristics of triple-negative and non-triple-negative. High grades breast carcinomas with and without basal markers (CKS 16 and EGFR) expression at a rural tertiary hospital in india breast cancerBasic Clin Res620122129
- K.BhumsukI.Seock-AhKyung-HunKi-67 can be used for further classification of TNBC into two subtypes with different response and prognosisBreast Cancer Res132011R2210.1186/bcr2834 <http://breast-cancer-research.com/content/13/2/R22>
- KristrinaJoensnuMarjutLeidenlusMiaKeroER, PR, HER-2, ki-67, cks in early and late relapsing: breast cancer-reduced CKS expression in metastasesBreast Cancer: Basic Clin Res720132334
- RoohiIsmail-KhanMarilyn M.BuiA review of triple-negative breast cancerCancer Control1732007173176
- Joseph P.GarayBedriKarakasAbde M.A.BukhdeirDavid P.GosgroveThe growth response to AR Signaling in ERX-negative human breast cancer cell is dependent on P21 and mediated by MAPK activationBreast142012R27 doi: 10.11861bcr3112
- Careyl E.DeesL.SqwyerThe triple-negative paradox: primary tumor chemosensitivity of breast cancer subtypesClin Cancer Res13200723292334
- C.LiedtkeC.MazouniK.HessResponse to neoadjuvant therapy and long-term Survival in patients with TNBCJ Clin Oncol26200812751281
- L.J.MC GhanA.E.MC culloughC.A.ProtheroeAndrogen receptors positive TNBC: a unique breast cancer subtypeAnn Surg Oncol2122014361367 doi: 10.12451510434-013-3260-7-Epub2013Sep18
- S.SparkJ.S.KooM.S.KimAndrogen receptors expression is significantly associated with better outcomes in ER – positive breast cancerAnn Oncol228201017551762
- A.K.AgrawalM.JelenGrzebieniakzAR as a prognostic and predictive factor in BCFolia Histochem Cytobiol462008269276
- V.OgawaE.HaiK.MatsumotoAR expression in breast cancer: relationship with clinicopathological factors and biomarkersInt J Clin Oncol132008431435
- R.E.MoeBoAndersonAndrogen and androgen receptors a clinical neglected sector in breast cancer biologyJ Sur Oncol952007437439
- Z.NahlehAndrogen receptor as a target for the treatment of hormone receptor-negative breast cancer: an unchartered territoryFuture Oncol420081521
- K.HanleyJ.WanP.Bournelack of expression of AR may play a critical role in transformation from in situ to invasive basal subtype of high grade ductal Cacinoma of the breastHum Pathol392008386392
- C.RivaE.DalneseG.CapraraImmuno histochemical study of androgen receptors in breast carcinoma. Evidence of their frequent expression in lobular carcinomasVirchows Arch4472005 965-700
- L.C.ChoY.H.HsuExpression of androgen, estrogen and progesterone receptors in mucinous carcinoma of the breast. Kaoh-suingJ Med Sci242008227232
- Aye AyeThikeLuke Yong-ZhengChongLoss of androgen receptor expression predicts early recurrence in triple-negative and basal-like breast cancerModern Pathol920131038 doi: 10.10381modpathol.2013.145
- Ashwani K.MishraUshaAgrawalShivaniNegiExpression of androgen receptor in breast cancer & its correlation with other receptor and growth factorsIndian J Med Res1352012843852
- D.ShaheenabTNBC: epidemiology and management optionsDrugs70201022472258
- Kaplan HG, Malngren JA, Al wood MK. Import of TNBC phenotype on breast cancer prognosis. Poster presented at: 29th annual san Antonio Breast cancer symposium. San Antonio, TX; 2006, December 14–17.
- M.C.CheangD.VoducC.BajdikBasal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotypeClin Cancer Res145200813681376
- D.G.HicksS.M.ShortN.L.PrescottBreast cancers with brain metastases are more likely to be estrogen receptor negative, express the basal cytokeratin CK5/6, and overexpress HER2 or EGFRAm J Surg Pathol309200610971104
- W.D.FoulkesI.E.SmithJ.S.Reis-FilhoTriple-negative breast cancerN Engl J Med36320201019381948
- M.TischkowitzJ.S.BrunetL.R.BeginUse of immunohistochemical markers can refine prognosis in triple negative breast cancerBMC Cancer72007134
- R.DentW.M.HannaM.TrudeauTime to disease recurrence in basal-type breast cancers: effects of tumor size and lymph node statusCancer11521200949174923
- S.ParkJ.KooH.S.ParkExpression of androgen receptor in primary breast cancerAnn Oncol212009488492
- GuozB.DaiJiantRegulation of androgen receptor activity by tyrosine phosphorylationCancer Cell102006309319
- S.N.AgoffP.E.SwansonH.LindenAndrogen receptors expression in estrogen receptor-negative breast cancer. Immunohistochemical, clinical and prognostic associationsAm J Clin Pathol1207200325731
- S.Toth-fejelJ.cheekCalhounkEstrogen and androgen receptors as comediators of breast cancer cell prolifrationArch Surg1392004 50-S4
- A.A.ThikeL. Yong-ZhengChongP.Y.CheokLoss of AR expression predicts early recurrence in triple-negative and basal-like breast cancerMoodern Pathol2732014352360
- ChelseaHardinRodneyPommierKristineCalhounA new hormonal therapy for estrogen receptor-negative breast cancerWorld J Surg31200710411046 doi: 10-10071S00268-007-0694-8
- Mod pathology. Androgen R in breast cancer: Expression in ER +ve tumors and ER-negative tumors with apocrine differentiation USA. Leo Aniemeier; 2010.
- Traina A, Wolff AC, Girik Feigin D. AR inhibition for the treatment of AR+ve, ER-ve, PR-ve, metastatic breast cancer. 2009 Breast cancer symposium. (Asco home) Momorial Sloan-Kettering cancer center, New York, NY. Translational Breast cancer Research Con Sortium, Baltimore MD; 2009.
- A.GucalpM.T.SaraJ.StevenASCO, targeting the androgen receptor (AR) in women with AR/PR-metastatic breast cancer (MBC)J Clin Oncolsuppl; abstr 1006201230 <http://meetinglibrary.asco.org/content/94715-114>
- M.CheangAsco. Triple-negative breast cancer and treatment: what do we know?Clin Cancer Res142012 1368-1367
- NaderiAliHughes-DavisLukeA functionally significant cross-talk between AR and ERB2 pathways in estrogen receptor negative BCNeoplasia1062008542548
- F.MoinfarM.OkcuO.TsybrovskyyAR frequently are expressed in breast carcinoma: potential relevance to new therapeutic strategiesCancer982008703711
- A.R.TanS.M.SwainTherapeutic strategies for TNBCCancer J142008343351
- Payal DShahAycaGucalpTiffany A.TrainaThe role of the androgen receptor in triple-negative breast cancerWomen’s Health94201335136010.2217/whe.13.33