Abstract
Introduction
Pelvic congestion syndrome (PCS), is a condition associated with ovarian vein (OV) incompetence among other causes. It is manifested by chronic pelvic pain with associated dyspareunia and dysmenorrhea. The diagnosis of PCS is often overlooked and the management can be difficult. Traditional therapy for PCS has included both medical and surgical approaches and more recently endovascular therapy.
The aim of this work
The aim of this work was to assess the clinical efficacy of ovarian vein embolization in treatment of PCS associated with OV incompetence and in the management of pelvic varices via catheter directed coil embolization.
Conclusion
From our and previous results, we can conclude that catheter directed OV coil embolization is a feasible procedure for treatment of pelvic congestion syndrome associated with OV incompetence. Presence of bilateral OV incompetence should always be investigated prior this therapy. Further prospective trials are required to assess the full benefits and efficacy of this technique, and to assess which may be the best embolic agent.
1 Introduction
Chronic pelvic pain (CPP) is a significant health problem in women particularly during childbearing age and may account for 10% of outpatient gynecologic visits.Citation1,Citation2 Etiology of chronic pelvic pain includes irritable bowel syndrome, endometriosis, adenomyosis, pelvic congestion syndrome, atypical menstrual pain, urologic disorders, and psychosocial issues.Citation3,Citation4
Pelvic congestion syndrome occurs mostly because of ovarian vein reflux, but can also occur because of the obstruction of ovarian vein outflow resulting in reversed flow.Citation5
Ovarian vein reflux (OVR) is found and PCS is diagnosed most frequently in multiparous women. During pregnancy, ovarian vein flow may increase up to 60 times. This increase in blood flow causes ovarian vein dilatation and may result in venous valve incompetence. PCS is likely caused by the incompetence of the venous valves of the ovarian and pelvic veins, which results in OVR leading to ovarian and pelvic vein dilatation and stasis. Therefore incompetence, venous reflux, and dilatation of the ovarian veins lead to the development of pelvic varicosities and congestion, which are known causes of pelvic pain and the most likely etiology of PCS.Citation6
The presence of OVR by itself does not make the diagnosis of PCS. But venous reflux in the ovarian veins of patients with CPP and with no other identifiable cause of organic pain makes the diagnosis of PCS.Citation6
Pelvic congestion syndrome can present with nonspecific pelvic pain, dyspareunia, and persistent genital arousal.Citation5 The pelvic pain of PCS may vary along the menstrual cycle and worsen during menses and be exacerbated by conditions that may increase congestion such as the upright position, bending and lifting, and coitus. The pelvic pain may be described as fullness and heaviness. The pelvic examination may demonstrate pelvic tenderness, congestion of the vaginal walls, and varices.Citation6 Pelvic varices can be seen in 10% of women in the general population and up to 60% of patients with pelvic varices may develop pelvic congestion syndrome. Varices can be seen in the vulva, buttocks, and legs.Citation5
Venography, CT, MRI, and Doppler US can demonstrate OVR. Noninvasive imaging such as sonography, MR, or CT not only may demonstrate the retrograde ovarian vein flow but also may exclude other pelvic pathologies that may be the cause of CPP as well as determine the size of the ovarian veins, and the presence of pelvic varicosities.Citation6 MRI is preferable as it avoids the large radiation dose associated with CT, which should be avoided where possible in young women. For PCS, an ovarian vein diameter of 8 mm on CT or MRI is considered diagnostic.Citation7
Non-steroidal anti-inflammatory drugs may help relieve pain in the short term but these are not a long-term solution to the patient’s problem. Analgesia is a good first line treatment but symptoms should not be ignored if it is not completely effective or pain recurs when it is stopped.Citation8
Hysterectomy and bilateral oophorectomy with hormone replacement are said to be an effective cure or at least symptomatic improvement in two-thirds of patients with PCS.Citation9 This surgical option, however, is not as effective as ovarian vein ligation, which has been reported as having a 73% cure rate with 78% of patients showing symptomatic improvement. However, ligation also cuts nerves to the pelvis and allows the establishment of collateral channels and recurrence of symptoms. Surgery is rarely used these days because endovascular treatments are more effective and less invasive.Citation8
Unlike ligation, endovascular embolization of the ovarian vein leaves the nerves that accompany the vein intact. Though it does allow the establishment of collaterals, these are limited by occlusion of collaterals that drain into the high ovarian vein.Citation8
Significant pulmonary embolic disease due to migration of embolic material does not seem to be a complication of embolizing the ovarian veins. Spasm and occasional rupture of the thin-walled ovarian vein can occur but this rarely leads to any sequelae and can be treated with simple analgesia.Citation8
2 Material and methods
This study was conducted on 11 patients over a period of 3 years.
The mean age of the patients was 39.8 years with a range of 31–52 years. All patients were uniparous or multiparous.
10 patients presented with lower abdominal pain and vulval varicosities, 5 of them had thigh varicose veins as well. One patient had no pelvic pain symptoms, but presented with thigh varices; the Doppler scan of this patient suggested pelvic source of the varices.
Five patients had unilateral left OV embolization and 6 had bilateral OV embolization; in 5 patients bilateral embolization was performed in the same sitting, while the remaining patient underwent staged embolization. Embolization was performed using Spirale coils (Pyramed, Australia) in all patients.
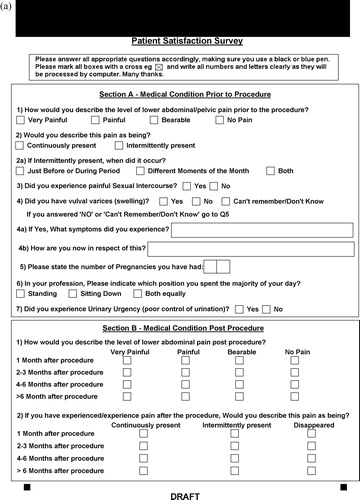
Outpatient clinical assessment and mailed questionnaires () were conducted 3–72 months post-embolization with a mean follow-up period of 28.1 months.
2.1 Procedure
The procedure was performed under local anesthesia. After puncture of the right femoral vein with a 5-French sheath (Cordis, Johnson & Johnson Medical, Diegem, Belgium), a cobra catheter (Cook Medical Inc, Bloomington, USA) was advanced into the left renal vein. Subsequently, the left ovarian vein was catheterized and a venogram was performed. The right ovarian vein is selectively catheterized directly into the IVC below the level of the right renal vein.
Embolization was performed with Spirale coils (Pyramed, Australia). After embolization, repeat venography was performed to confirm OV thrombosis, and the patency of the left renal vein.
The criteria for embolization included the following: an OV diameter of more than 8 mm, moderate to severe congestion of the ovarian plexus, and filling of the contralateral pelvic veins. Parallel OV trunks that entered the main trunk or that directly entered the left renal vein were embolized as well.
3 Results
Intraprocedural ovarian venography confirmed presence of pelvic varices in all 11 patients.
The procedural success rate was 100%; 5 patients had unilateral left OV embolization and 6 had bilateral OV embolization.
Post-embolization pelvic pain relief and relief of vulval varices were encountered in 7 of 10 patients (70%) by 3 months after the procedure.
Recurrent pelvic pain and vulval varices occurred in 1 patient (10%) after 6 months of embolization.
Improvement of thigh varicosities was reported in 4 of 6 patients (66.7%).
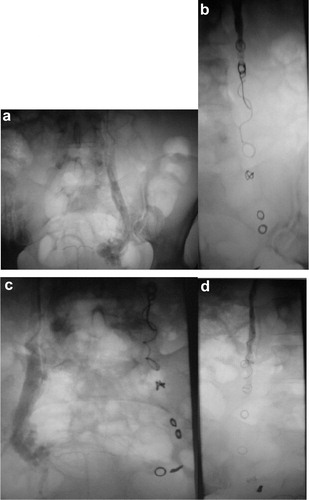
No significant complications encountered in the study group regarding coil migration, contrast extravasation, or puncture site hematoma (see and ).
Figure 2 (a) Selective left ovarian vein (OV) venography showing dilated OV. (b) Left OV occlusion with multiple coils (6 mm in diameter). (c) Selective right ovarian venography in the same sitting shows dilated right OV. (d) Multiple coils are placed in the right OV and venography immediately after embolization demonstrates occlusion of the right OV.
4 Discussion
Women who report intermittent or continuous pelvic pain and have no apparent disease have to be considered potential candidates for pelvic congestion syndrome. The pelvic pain is often described as fullness or heaviness, has a variable intensity and duration, and often worsens pre-menstrually.Citation10 Ovarian vein embolization has been used for many years as a treatment for OVS resistant to medical therapy. Coil embolization, first described in 1993.Citation11
Our results were comparable to other studies of clinical outcome of ovarian vein coil embolization in PCS, as summarized in .
Table 1 Clinical outcome of ovarian vein coil embolization in PCS in different studies.
We did not encounter any post-procedural complications, and other studies reported low rate of coil migration 3%Citation12 and 9.1%Citation13. Coil migration could happen if the coil was not sized correctly, or if it was inserted too close to the renal vein.
Pelvic vein relief was variable ranging from partial to complete relief in all studies; in our study 7 out of the 10 patients with pelvic pain showed partial or complete relief, and our results were comparable to others. Pain recurrence occurred in 10% of cases in our study compared to 22–26% in other studies.Citation13,Citation14
The clinical outcome of the patients did not differ according to whether the patient has unilateral or bilateral insufficient ovarian veins on retrograde venography, and the same finding was reported by Maleux et al.Citation10
In Kwon et al.Citation12, 13.4% of patients underwent surgery to get relief from persistent pain after embolization. None of our patients underwent surgery following embolization.
Pelvic congestion syndrome is a clinical entity that is often disregarded; therefore, clinicians who do not include trans-vaginal ultrasound with color Doppler in the diagnostic evaluation of chronic pelvic pain continue to refer these women for psychotherapy, with a presumed diagnosis of undetectable organic disease.Citation16 Hence the relative small number of patients in most of the studies, including ours.
5 Conclusion
From our and previous results, we can conclude that catheter directed OV coil embolization is a feasible procedure for treatment of pelvic congestion syndrome associated with OV incompetence. Presence of bilateral OV incompetence should always be investigated prior to this therapy. Further prospective trials are required to assess the full benefits and efficacy of this technique, and to assess which may be the best embolic agent.
Conflict of interest
We have no conflict of interest to declare.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 20 February 2016
References
- S.J.ParkJ.W.LimT.Y.KoDiagnosis of pelvic congestion syndrome using transabdominal and transvaginal sonographyAJR Am J Roentgenol1822004683688
- R.W.BeardS.PearceJ.H.HighmanmDiagnosis of pelvic varicosities in women with chronic pelvic painLancet21984946949
- A.D.LiddleA.H.DaviesPelvic congestion syndrome: chronic pelvic pain caused by ovarian and internal iliac varicesPhlebology2232007100104
- Y.CheongR.William StonesChronic pelvic pain: aetiology and therapyBest Pract Res Clin Obstet Gynaecol2052006695711
- M.KarcaaltincabaD.KarcaaltincabaV.DograPelvic congestion syndromeUltrasound Clin32008415425
- M.CuraA.CuraWhat is the significance of ovarian vein reflux detected by computed tomography in patients with pelvic pain?Clin Imaging332009306310
- H.BhuttaS.WalshT.TangC.WalshJ.ClarkeOvarian vein syndrome: a reviewInt J Surg72009516520
- T.NicholsonA.BasilePelvic congestion syndrome, who should we treat and how?Tech Vasc Intervent Radiol920061923
- R.W.BeardP.W.ReginaldJ.WadsworthClinical features of women with chronic lower abdominal pain and pelvic congestionBr J Obstet Gynaecol951998153161
- G.MaleuxL.StockxG.WilmsG.MarchalOvarian vein embolization for the treatment of pelvic congestion syndrome: long-term technical and clinical resultsJVIR112000859864
- R.EdwardsI.RobertsonA.MacLeanA.HemingwayCase report: pelvic vein syndrome – successful treatment of a case by ovarian vein embolizationClin Rad471993429431
- S.H.KwonJ.H.OhK.R.KoH.C.ParkJ.Y.HuhTranscatheter ovarian vein embolization using coils for the treatment of pelvic congestion syndromeCardiovasc Intervent Radiol3042007655661
- P.R.CordtsA.EclaveaP.J.BuckleyC.A.DeMaioribusM.L.CockerillT.D.YeagerPelvic congestion syndrome: early clinical results after transcatheter ovarian vein embolizationJ Vasc Surg2851998862868
- P.CapassoC.SimonsG.TrotteurTreatment of symptomatic pelvic varices by ovarian vein embolizationCardiovasc Intervent Radiol201997107111
- G.N.BacharA.BelenkyF.GreifInitial experience with ovarian vein embolization for the treatment of chronic pelvic pain syndromeIsr Med Assoc J122003843846
- T.GargiuloV.MaisL.BrokajE.CossuG.B.MelisBilateral laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndromeAm Assoc Gynecol Laparosc1042003501504