Abstract
Objective
To assess the diagnostic accuracy of combined use of conventional grayscale US and sono-elastography in differentiating benign and malignant solitary thyroid nodules.
Materials and methods
This prospective study included 50 patients with solitary thyroid nodules being evaluated using grayscale US followed with sono-elastography (USE). Suspicious conventional sonographic data for malignancy then evaluated using USE were classified according to Rago criteria with calculation of strain ratio. The diagnostic performances of grayscale US, elastography with Rago criteria, for predicting thyroid malignancy were compared and cutoff value for strain ration was statistically analyzed. Finally all patients with solitary nodule were subjected to US-guided FNAC and 35 patients recommended for surgery in the form of 12 patients underwent total thyroidectomy and 23 patients underwent thyroidectomy with neck dissection.
Results
30 females (60%), and 20 males (40%) were included (Mean age 38) with final diagnosis comprised 29 (58%) pathologically proved benign thyroid nodules and 21 (42%) pathologically proved malignant nodules. US showed significant relation between markedly hypo-echogenicity, oval than tall, margin irregularity, presence of micro-calcification with diagnosis of thyroid malignancies with p value <0.001. Regarding sonoelastography, there was significant relation between elastography scores 4 and 5 and thyroid malignancies showing sensitivity of 80%, a specificity of 100%, and p value <0.001. The most accurate strain ratio cutoff value among studied cases was 2.52. Combination of grayscale US and sono-elastography yielded better results with sensitivity of 92%, specificity of 95%, PPV of 89%, NPV of 92% and diagnostic accuracy or efficacy of 96%.
Conclusion
Combined use of USE and grayscale US, showed superior performance in the differentiation of malignant and benign thyroid nodules compared with each technique alone. Suspicious US criteria with elasticity Rago scores 4 and 5 and strain ratio more than 2.52 are the most predictive signs of malignancy.
Keywords:
1 Introduction
Thyroid nodules presented commonly as they are found in 4–8% of adults by palpation, in 10–41% by ultrasound either intentionally or incidentally, and in 50% by pathologic examination at autopsy.Citation1 Inspite of high prevalence of nodules, thyroid cancer is relatively rare and not more than 6% of all nodules being malignant; however, thyroid cancers generally have good prognosis and fortunately, early diagnosis and treatment is fruitful.Citation2
Table 2 Distribution of Patients according to elastogram score in correlation with post operative histopathology.
Common presentation of cancer thyroid is solid solitary nodule and therefore, it is crucial to differentiate between the benign and malignant causes and hence it is essential to have a strategy determining which nodules candidates for fine needle aspiration cytology.Citation2,Citation3
Ultrasound has a wide utility more than confirming presence of thyroid nodules and assessment of its size, texture and vascularity as it added helpful information about the qualitative characterization of thyroid nodules based on benign or malignant features.Citation4,Citation5
Experienced hand palpation can give initial idea about nodule stiffness, and hence, can suggest possibility of being malignant, considering that the more firm nodules are likely to be malignant. On the other way, deep or small nodules are hardly evaluated by palpation and recently, used the elasticity imaging, namely sono-elastography (USE), that estimates the tissue mechanical properties in vivo using complementary conventional US systems with modified software.Citation6,Citation7
The idea of its application depends upon low-amplitude, low-frequency shear waves that are propagated through thyroid gland and whenever hard inhomogeneity, for example tumor, is present, a decrease in the vibration amplitude will occur at its location. Under a certain applied force, stiff tissue shows less strain than softer tissue. Thus, by measuring tissue strain induced by compression we can obtain tissue stiffness information.Citation8,Citation9
Thyroid gland is well positioned for elastographic examination due to superficial and anterior location, and so could be easily compressed against underlying anatomic structures by US probe.Citation10,Citation11 Tissue deformation or strain caused by compression is estimated with pre- and post-compression ultrasonic signals. Regarding fundamentals of sonoelastography, it is proposed that elastic modulus for malignant thyroid nodules is significantly higher than that for normal thyroid tissue and benign nodules, which establishes the idea for application of USE in assessment of the nature of nodules.Citation12–Citation14
Multiple variable sonoelastography scores, depending on the color changes or numerical estimation of the degree of stiffness are applied. Rago’s scoring system is the commonest, representing five-degree elastography qualitative evaluation system that can be applied to thyroid nodules using a scale of 1–5 with color coding varied from green (most benign) to blue (most malignant).Citation15
Other numerical methods such as estimating strain ratio (calculated as the ratio of stiffness between nodular tissue and surrounding normal thyroid tissue) could be of help to differentiate benign from malignant solitary thyroid nodules besides using the color scale.Citation16
To address terminology and other issues related to thyroid fine-needle aspiration (FNA), the National Cancer Institute (NCI) hosted the NCI Thyroid FNA State of the Science Conference. The conclusions regarding terminology and morphologic criteria from the NCI meeting led to the Bethesda Thyroid Atlas Project and form the framework for The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC). Bethesda classification is graded into 6 grades according to degree of risk of malignancy linked with recommended clinical management.Citation17
Objective was to evaluate combined role of grayscale US criteria with help of USE as a recent screening modality in differentiating benign from malignant solid thyroid nodules.
2 Patients
Current prospective study was conducted from 1–2014 to 5–2015 on selected 50 patients having solitary thyroid nodule either by clinical palpation or by conventional US neck examination, who were referred to Radiology department.
2.1 Inclusion criteria
Patients with palpable solitary thyroid nodule, those of solid or predominantly solid nature (75% or more solid consistency), patients with incidentally noted thyroid nodules during US or CT neck examination for other reasons, patients who had conclusive FNA result and/or underwent surgery after US examination.
2.2 General exclusion criteria
Patients with non-conclusive final pathological diagnosis, patients having more than one nodule or multiple confluent thyroid nodules with ill-defined margins. Regarding USE examination, we excluded nodules more than 4 cm in diameter to have enough surrounding residual normal thyroid tissue to be compared with the nodule, using either color or numerical scales. Cystic (or predominantly cystic nodules) and nodules having egg-shell calcification were excluded.
This was explained as posterior enhancement of the cysts or posterior shadowing of the calcification will obscure the posterior margin of the nodules and so interfere with accurate elastography scoring. Also technical limits for applying USE in cystic nodules (as classic elastogram for a cyst consists of three color layers {blue–green–red} from top to bottom) and macro-calcifications (coarse or egg shell) have hard blue appearance at real-time USE, as the US beam does not cross the calcification and the compression does not result into tissue strain deformation.
Current study protocol was approved by the Committee of Ethics and all patients had informed written consents. Complete history taking was performed including age, sex and symptoms. Full dedicated general and local clinical examination was done. The patients were operated upon maximum within 10 days of the real-time ultrasound elastographic evaluation.
3 Methods
3.1 Conventional ultrasonography (US) and sono-elastography (USE)
Real-time conventional US and sonoelastography examinations were performed for all patients by the same radiologist, having more than 7 years of experience in thyroid imaging, using a 6–14 MHz linear transducer, Siemens Acuson X300 PE premium ultrasound machine (Erlangen, Germany).
Patients were supine and positioned on his or her back with the neck slightly extended over a pillow under the shoulders to prevent over stretching of the neck muscles.
The probe was placed on the patient’s neck with US gel creating a stand-off pad. Transverse and longitudinal grayscale US images followed by real-time USE for each nodule were obtained. Diameter, cystic nature and rim calcification were evaluated as important excluding points. The composition was described as solid, predominantly solid (where the cystic component occupying area of less than 25%).
Suspicious grayscale US features for malignancy included marked hypo-echogenicity, non or poorly defined margin (loss of halo sign), micro-calcifications (punctate), taller than oval shape. If one or more of these suspicious features are seen by grayscale US features, the nodule was assessed as “suspicious” and nodules with no suspicious features were assessed as “probably benign”.
After US, sonoelastography technique was performed using same probe where the elastography function was activated with split-screen technology. US elastogram image was displayed over B-mode image on right side of the screen in a color scale that ranged from red for components with the greatest elastic strain (softest) to blue for those with no strain (hardest) where the green showed intermediate elasticity.
B-mode sonography images were displayed on the left side of the screen, to compare both images of the same scan plane. Elastographic images include nodule with sufficient surrounding normal thyroid tissue, which were obtained with appropriate compression. Images were considered reliable when the coloring was constant over the entire nodule for more than 5 s. Light level of pressure is maintained constant throughout the examination as excess pressure results in false readings.
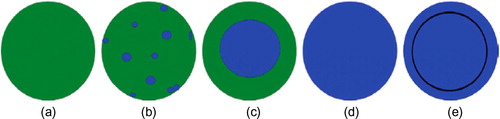
In the current study, sonoelastography scoring was performed on the basis of Rago et al.,Citation15 score () that is widely used as a qualitative evaluation system for thyroid nodules, using a scale of 1–5. Nodules with Rago scores of 4 and 5 were classified as suspicious for malignancy.
Figure 1 Rago elastography criteria for assessment of thyroid nodules: (a) score of 1, indicated even elasticity along the entire nodules, (b) score of 2, indicated elasticity along most of the nodule, (c) score of 3 indicated preserved elasticity at the periphery of the nodule, (d) score of 4 indicated no elasticity along the entire nodule, (e) score of 5 indicated loss of elasticity in the whole nodule and along the area showing posterior shadowing. Rago et al. Citation15
3.2 US-guided FNAC and histopathological diagnosis
All nodules were subjected to FNAC and 35 patients recommended for surgery in the form of 12 patients underwent total thyroidectomy and 23 patients underwent thyroidectomy with neck dissection. Histopathological examination included gross and microscopic examination of the thyroid nodule as well as the adjacent thyroid parenchyma.
4 Data analysis
4.1 Statistical analysis
Data were fed to the computer using IBM SPSS (V. 21.0, IBM Corp., USA, 2012) software package version 20.0. Data were expressed as mean ± standard deviation (SD) for quantitative parametric measures, in addition to median percentiles for quantitative non-parametric measures and qualitative data were described using both number and percentages.
Comparison between different groups regarding categorical variables was tested using Chi-square test. For comparison between two independent mean groups for parametric data, Students’s t-test was used. Quantitative data were described using mean and standard deviation for normally distributed data while abnormally distributed data were expressed using median, minimum and maximum.
The final histopathological diagnosis was used as the reference standard. The probability of error (p value) at 0.05 was considered significant, while, at 0.01 and 0.001 was considered highly significant. In addition, the diagnostic validity test was used to calculate the sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy or efficacy. Finally, estimation of the best cutoff value for the strain ratio was assessed.
5 Results
5.1 Demographic data
The study included 50 patients presented with solid or predominantly solitary thyroid nodules, of them, 30 were females (60%), and 20 were males (40%) (Mean age 38, ranged between 23 and 70 years). Final diagnosis comprised 29 (58%) pathologically proved benign thyroid nodules and 21 (42%) pathologically proved malignant nodules. The mean age of benign cases was 34 years and mean age for malignant cases was 62 years.
All patients were evaluated initially using grayscale ultrasound, followed with sono-elastography. Commonest complaints were painless neck swelling (26 patients 52%), compression manifestations (9 patients 18%), hoarseness of voice (2 patients 4%) and toxic manifestations (2 patient 4%) and eleven patients (22%) were asymptomatic and nodules were incidentally discovered during neck scanning for extra-thyroid neck diseases.
5.2 Histopathological examination
All included patients subjected to US-guided FNAC and the results were classified according to the Bethesda systemCitation17 for histopathological diagnosis of thyroid nodules. Final histopathological results () revealed 29 cases of benign nodules distributed as follows: 20 hyperplastic nodules (), 3 subacute thyroiditis, 3 follicular adenomas () and 3 Hashimoto’s thyroiditis (), and 21 cases of malignant nodules as follows: 12 papillary carcinomas (), 6 follicular carcinomas () and 3 medullary carcinomas (). 35 patients were recommended for surgery (12 patients underwent total thyroidectomy and 23 patients underwent thyroidectomy with neck dissection).
Figure 2 54 years old male patient presented with painless neck swelling since 3 years (A) Transverse grayscale US of a thyroid nodule at the junction between the isthmus and the left lobe showing mainly solid nodule, hypo-echoic to thyroid parenchyma with thin regular halo surrounding the nodule (black arrow). (B) US elastogram showing elasticity score 2 and strain ratio was 1.9. FNAC revealed Bethesda II. Total thyroidectomy was done, and final diagnosis was benign hyperplastic nodule.
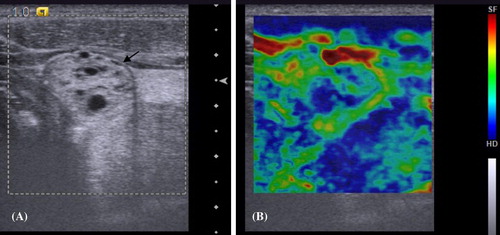
Figure 3 40 years old female patient presented by painless neck lump since two years.(A) Transverse grayscale US of a right thyroid nodule showing a well defined, solid, homogenously slightly hypoechoic nodule (black arrow). (B) US elastogram showing elasticity score 3, strain ratio was 2.4. FNAC was Bethesda IV. Total thyroidectomy was done, and the diagnosis was follicular adenoma.
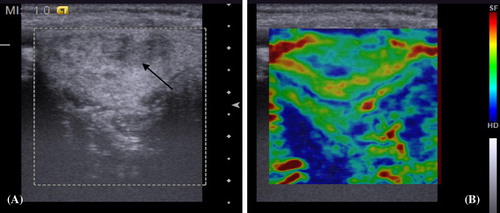
Figure 4 50 years old male patient presented painless neck swelling since one year with rapid growth in the last four months. (A) Transverse grayscale US of the left thyroid lobe showing hypoechoic echotexture and multiple internal echogenic septae (black arrow). (B) US elastogram showing elasticity score 3 and strain ratio 2.1. FNAC showed Bethesda V. Total thyroidectomy was done and the diagnosis was nodular Hashimoto thyroiditis.
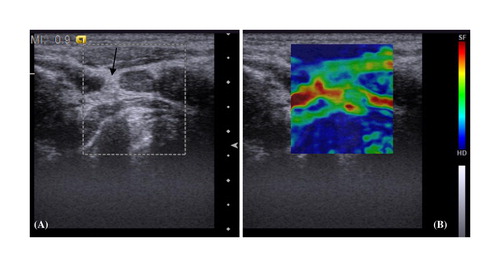
Figure 5 35 years old male patient presented with painless neck lump since one year. (A) Transverse grayscale US of a right thyroid nodule showing predominantly solid nodule, isoechoic, well defined and surrounded by thin regular halo with punctuate foci of micro-calcification (black arrow). (B) US elastogram showing elasticity score 4 and strain ratio 2.7. FNAC revealed Bethesda IV. Total thyroidectomy was done and the diagnosis was follicular carcinoma.

Figure 6 21 years old female patient presented with painless neck swelling since three months. Thyroid function was normal. (A) Transverse grayscale US of a solid nodule at the junction between the isthmus and right lobe showing solid isoechoic echotexture with irregular margin and multiple punctuate echogenic foci of micro calcification (black arrow). (B) US elastogram showing elasticity score 5 and strain ratio was 4.3. FNAC showed Bethesda IV. Total thyroidectomy with neck dissection was done and the diagnosis was papillary carcinoma with nodal metastasis.
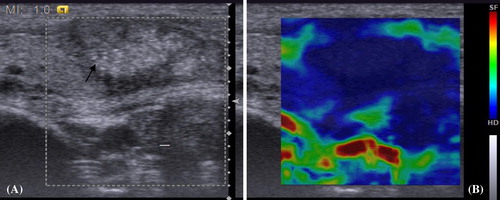
Figure 7 32 years old male patient presented with painless neck swelling since one year. The patient had positive family history of medullary carcinoma, bilateral pheochromocytoma and was diagnosed as MEN IIA. (A) Longitudinal grayscale US of a right thyroid nodule showing hypo-echogenicity, lobulated margin and multiple echogenic foci of micro-calcification (thick white arrow). (B) US elastogram showing elasticity score 5 and strain ratio 4.2. FNAC revealed Bethesda V. Total thyroidectomy was done and the final diagnosis was medullary carcinoma.

Table 1 Final histopathological diagnosis of the examined thyroid nodules.
5.3 Conventional sonography data analysis
Sonographic criteria included size, composition, echotexture, echogenicity, margin (presence of halo) and calcifications. No statistical significance found between sex and presence of malignancy; however 50% of the studied males had thyroid cancer. On the other hand, significant relation was found between the above 60 years patients and the presence of malignancies.
Included nodules (with diameter less than 4 cm) showed no significant relation between the size and malignant diagnosis.
All the hyper-echoic nodules (8 nodules representing 16%) were benign whereas 13 as 65% and 4 as 20% of the malignant nodules were hypo and markedly hypo-echoic respectively.
Well-defined margin was found in 18 as about 90% of the benign nodules compared to 7 as 33% of the malignant ones. 8 as 40% and 4 as 20% of the malignant nodules had irregular and lobulated margins respectively. Complete halo was present in 14 as 46.3% of the benign nodules compared to 4 as 16% of the malignant ones.
Three nodules showed both micro- and coarse calcifications that were all malignant. Ten of the malignant nodules (as 42%) had micro-calcification compared to none of the benign ones.
These findings were statistically significant with p value <0.001. Significant relation between findings such as marked hypo-echogenicity, oval than tall, margin irregularity, and presence of micro-calcification with the diagnosis of thyroid malignancies was found. Grayscale shows sensitivity 92%, specificity 34% and positive predictive value (PPV) 85.4% and negative predictive value (NPV) 72.3% and accuracy 73%.
5.4 Real time sono-elastography data analysis ()
According to Rago’s criteriaCitation15 for elasticity scoring system the results included the following: among 29 benign nodules, 12 nodules (representing 41%) had score 1, 14 nodules (48%) had score of 2 and 3 nodules (10%) had score of 3 including nodules of subacute thyroiditis, Hashimoto’s thyroiditis and one for follicular adenoma. None of the benign nodules diagnosed as score 4 or 5.
On the other hand, 21 malignant nodules comprised five cases (24%) had score of 3, all were follicular carcinomas, 12 cases (57%) had score of 4 as papillary, follicular and medullary carcinoma and the remaining four cases (19%) had score 5, of them were papillary carcinoma and one was follicular carcinoma. None of the malignant cases diagnosed as score 1 or 2.
Accordingly, scores of 1 and 2 with Rago criteria were highly significant in benign nodules, whereas, scores of 4 and 5 were highly significant seen in malignant nodules (p < 0.001). There was a significant relation between elastography scores 4 and 5 and thyroid malignancies showing sensitivity of 80%, a specificity of 100%, and p value <0.001.
Scores 4 and 5 with Rago criteria were predictive of malignancy with a sensitivity of 78.6%, while, scores 1 and 2 were predictive of benign disease with a specificity of 78.9%. The positive predictive value for malignancy was 73.3%, while, the negative predictive value for benign disease was 83.3% and the diagnostic accuracy or efficacy was 78.8%.
Using numerical data analysis for the strain ratio to discriminate between benign and malignant solitary thyroid nodules, we found in the current study that the most accurate strain ratio cutoff value among studied cases was 2.52. The area under the curve was 0.861 and p was <0.001, meaning that a strain ratio >2.52 identified malignant nodules and a strain ratio <2.52 identified benign nodules having sensitivity of 85.7%, specificity of 90.5%, positive predictive value of 85.7%, negative predictive value of 90.5% and diagnostic accuracy or efficacy of 88.6%.
Among malignant thyroid nodules (n = 21), 7 nodules (33.3%) had a strain ratio 4 and 14 nodules (66.6%) had a strain ratio >2.52. Comparatively, among those benign nodules (n = 29), 24 nodules (82%) had a strain ratio less than 2.52.
Combination of grayscale US and sonoelastography yielded better results than using each technique independently, as combination showed sensitivity of 92%, specificity of 95%, positive predictive value of 89%, negative predictive value of 92% and diagnostic accuracy or efficacy of 96%.
6 Discussion
Variety of radiological approaches for characterizing solitary thyroid nodules were applied ranging from conventional ultrasound till MRI updates (including DWI) including radionuclide studies as isotope scanning and FDG-PET. Inspite of sensitivity of these modalities for lesion detection, yet most of them lack specificity for predicting malignancy and hence of limited clinical efficacy.Citation18,Citation19
Conventional US considered the initial tool for detection and characterization of palpable and deep nodules.Citation20,Citation21
In the current study, initial grayscale US used to select nodules highly suspicious for malignancy and also to exclude nodules having exclusion criteria, followed with USE as an easy technique coupled with US to give immediate combined accurate results.
Sonoelastography (USE) improved the diagnostic performance of grayscale US as the gland was suitable technically for effective compression against underlying anatomic structures using US probe and therefore for adequate evaluation of the elastic nature of the thyroid nodules.Citation22,Citation23
Our results revealed that 42% of the included thyroid nodules were malignant, matching with 21–54% in previous studies.Citation24–Citation26 This high percentage of malignancy was attributed to the selection of suspicious patients undergoing surgery and to exclusion criteria of purely cystic and the peripherally calcified nodules. Abodewan et al., estimated higher prevalence of malignancy of 62.2%.Citation27
We found that marked hypo-echogenicity, poorly defined margins, micro-calcifications, and taller than wide shape are high predictors for malignancy and agreed with many comparable authors.
Micro-calcifications (high specificity 98%, positive predictive value 91% and accuracy 81%), but major drawback was the low sensitivity (44%). This was matching with previous studiesCitation28–Citation30 as Hoang,Citation30 who mentioned that coarse calcifications might coexist with micro-calcifications in papillary cancers, as well as considered the commonest type of calcification in medullary thyroid carcinomas.
Marked hypo echogenicity considered a restricted sign for malignancy and was not detected in benign ones (high specificity and positive predictive value 100% with low sensitivity 16%), in agreement with Anil et al.,Citation31 and Moon et al.,Citation32 who stated that decreased echogenicity increased the risk for malignancy.
Hyperechoic nodules were seen in 5 nodules that were all benign, matching with Bonavita et al.,Citation33 who described the hyperechoic nodule as white knight that commonly found in benign lesions, and such nodules did not require biopsy.
The margin of nodules was considered ill-defined when more than 50% of demarcation between nodule and normal surrounding parenchyma was indistinct. Eleven nodules with irregular margin (one benign and ten malignant), and six with lobulated outline (one benign and five malignant), consider margin as useful marker of malignancy (specificity and PPV of 98.15% and 90.91% for irregular margin and 98.15% and 83.33% for lobulated margin respectively).
Our results were supported by Anil et al.,Citation31 who stated that the irregular margin was suggestive of malignancy; however, we contradicted Hoang et al.,Citation30 and Moon et al.,Citation32 who mentioned that unless frank invasion beyond thyroid capsule was demonstrated, the appearance of nodular alone was unreliable signs for either malignancy or benignity.
However, Anil et al.,Citation31 and Moon et al.,Citation32 results were concordant with ours considering taller than wide shape is a suggestive finding, but alone was not a reliable sign in differentiating malignant from benign nodules.
The elasticity scoring system initially proposed by Ueno and Itoh,Citation9 was useful for comparing breast ultrasound and elastographic results. In our study, tissue stiffness was scored from 1 to 5 on the basis of Rago scoring for subjective analysis of the elastogram.Citation15
We used light external compression “free hand” technique where elastographic image was created by a slight raising and lowering movement with the transducer and the elastogram is generated in real-time. Avoid applying high compression to be proportionate with strain level and to minimizing the inter- and intra-observer variability and hence obtaining reliable results occurred.
Using carotid artery pulsation as the compression source or other methods where elastogram was generated off-line, has disadvantages of their high costs and more time consuming. Carotid artery pulsation approach has advantage of correlating measurements with expansion and contraction of carotid artery lumen during systole and diastole due to near position of carotid artery to the thyroid. Major disadvantage was generating arterial unavoidable movements which in turn may create unnecessary thyroid movement interfering with perfect elastographic images.Citation34,Citation35
Rago scores of 4 and 5 in the current study were highly significant for malignancy which was concomitant with many previous studiesCitation22–Citation24,Citation26 and agreed with these results. Hong et al.,Citation36 adopted a stiffness scoring system ranging from 1 (low stiffness over the entire nodule) to 6 (high stiffness over the entire nodule and surrounding tissue). They found that 90% of benign nodules had a score of 1–3, whereas, 88% of the malignant had a score of 4–6.
All pathologically proved papillary carcinomas in the current study (9 cases 100%) had either scores of 4 and 5, matching with Hong et al.,Citation36, who found that 41 of 44 papillary thyroid carcinomas (93%) had a score of 4–6. Histopathologically, papillary thyroid carcinoma composed of complex papillae with a central fibro-vascular stalk and psammomatous calcific bodies and background fibrosis that would result in high level of tissue stiffness.Citation17,Citation36
Six cases of follicular thyroid carcinoma had low sensitivity with inability to differentiate between thyroid follicular carcinoma and follicular adenoma confidently. As well, we detected three follicular thyroid carcinomas having a score of 3 that was concordant with the study done by Hong et al.,Citation36
Histopathologically, follicular carcinoma may overlap with benign adenoma and be differentiated only when capsular or vascular invasion was discovered.Citation37–Citation39
Alternatively, high tissue stiffness in some benign nodules in our study is in one nodule as Hashimoto thyroiditis and two nodules as subacute thyroiditis (all had a score of 3) and this is attributed to tissue composition in subacute thyroiditis where normal tissue was replaced by a interstitial fibrosis and infiltration of lymphocytes, histiocytes and plasma cells.Citation37
Concomitantly, Hong et al.,Citation36 reported that two nodules in patients with subacute thyroiditis showed malignant USE finding.
Sensitivity and specificity of USE for differentiating thyroid nodules have been reported to be 82–97% and 77.5–100% respectively.Citation22–Citation23,Citation24,Citation26,Citation30 Our results showed that combined use of US and USE had sensitivity of 92%, specificity of 95%, positive predictive value of 89%, negative predictive value of 92% and diagnostic accuracy or efficacy of 96%.
Regarding strain ratio, our results matched with previous studiesCitation36,Citation37 showing that malignant nodules have a significantly higher stiffness compared to benign ones. Statistically, best discriminative strain ratio cutoff value in the current study was 2.52 with sensitivity 85.7%, specificity 90.5%, positive predictive value 85.7%, negative predictive value 90.5% and diagnostic accuracy or efficacy 88.6%. The results most matching with ours had sensitivity, specificity and diagnostic accuracy of the strain index values as 85.7%, 82.1% and 82.4%, respectively, when the best cutoff point of 2.31 was used.Citation8
In other studies by Cantisani et al.,Citation40 strain ratio cutoff value is 2.05 for discriminating between benign and malignant lesions with 87.5% sensitivity, 92% specificity and 89.8% diagnostic accuracy. On the other hand, Kagoya et al.,Citation41 found that a strain ratio greater than 1.5 was set as the predictor of thyroid malignancy with 90% sensitivity and 50% specificity.
Accordingly, in our opinion, combined use of grayscale US and USE as comprehensive diagnostic tools better than being used separately. The diagnostic performance of elastography itself or combined with grayscale US should be superior to grayscale alone.
Although the sensitivity was low in our study comparable to the previous studies, this was attributed to relatively small number of nodules, that was one of the major limitations of the current study and further studies including larger number of cases are recommended for more evaluation of the diagnostic performance of sonoelastography and in turn avoiding unnecessary surgical procedures for benign nodules and early diagnosis of malignant ones.
Other general limitations, related to the method itself, were that the impact of background abnormality in the thyroid parenchyma for example in Hashimoto thyroiditis was not adequately assessed. Further studies will be necessary to understand whether US elasto-graphic measurements can give reliable results in nodules that are greater than 25% cystic.
Last limitation of this technique was that the nodule to be examined must be clearly distinguishable from other nodules present in the thyroid, to select it for the US elastography measurement. Thus, multi-nodular goiters with coalescent nodules in most cases were not suitable for this analysis.
Our conclusions revealed that combined use of conventional and USE will help in differentiating solitary thyroid nodules considering that these nodules have no technical limits. Initial grayscale ultrasound screening could select suspicious nodules suitable for USE characterization, then use of color score and strain ratio reveals that high elasticity was markedly associated with benign histopathology and low elasticity is markedly associated with malignant histopathology.
Suspicious criteria for both techniques included nodules with marked hypo-echogenicity, irregular or lobulated margin, micro-calcifications, taller than wide shape along with Rago’s elasticity scores 4 and 5 considered the patterns most predictive of malignancy.
Conflict of interest
The authors stated that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 10 March 2016
References
- E.K.AlexanderE.MarquseeJ.OrcuttThyroid nodule shape and prediction of malignancyThyroid: Official J Am Thyroid Assoc142004953958
- E.PapiniR.GuglielmiA.BianchiniRisk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler featuresJ Clin Endocrinol Metab87200219411946
- L.HegedüsClinical practice. The thyroid noduleN Engl J Med35117200417641771
- J.I.LewC.C.SolorzanoUse of ultrasound in the management of thyroid cancerOncologist24201020092032
- O.AlperM.E.SukruE.AlkinThe diagnostic efficiency of ultrasound in characterization for thyroid nodules: how many criteria are required to predict malignancy?Med Ultras1420122428
- B.S.GarraE.I.CespedesJ.OphirElastography of breast lesions: initial clinical resultsRadiology20219977986
- A.LyshchikT.HigashiR.AsatoThyroid gland tumor diagnosis at US elastographyRadiology2372005202211
- F.TranquartA.BleuzenP.Pierre-RenoultElastosonography of thyroid lesionsJ Radiol8920083539
- A.ItohE.UenoE.TohnoBreast disease: clinical application of US elastography for diagnosis(1)Radiology2392006341350
- S.H.ParkS.J.KimE.-K.KimInter-observer agreement in assessing the sonographic and elastographic features of malignant thyroid nodulesAJR19352009W416W423
- A.LyshchikT.HigashiR.AsatoThyroid gland tumor diagnosis at US elastographyRadiology23712005202211
- D.-J.LimS.LuoM.-H.KimInterobserver agreement and intraobserver reproducibility in thyroid ultrasound elastographyAJR19842012896901
- N.NiledagK.ArdaB.K.AribasThe utility of ultrasound elastography and MicroPure imaging in the differentiation of benign and malignant thyroid nodulesAJR19832012W244W249
- J.BojungaE.HerrmannG.MeyerReal-time elastography for the differentiation of benign and malignant thyroid nodules: a meta-analysisThyroid2010201011451150
- T.RagoF.SantiniM.ScutariElastography: new developments in ultrasound for predicting malignancy in thyroid nodulesJ Clin Endocrinol Metab92200729172922
- C.-P.NingS.-Q.JiangT.ZhangThe value of strain ratio in differential diagnosis of thyroid solid nodulesEur J Radiol8122012286291
- E.S.CibasS.Z.AliConference NCITFSotS. The Bethesda system for reporting thyroid cytopathologyAm J Clin Pathol1322009658665
- G.Leidig-BrucknerG.CichorowskiP.SattlerEvaluation of thyroid nodules – combined use of 99mTc-methylisobutylnitrile scintigraphy and aspiration cytology to assess risk of malignancy and stratify patients for surgical or nonsurgical therapy – a retrospective cohort studyClin Endocrinol (Oxf)7652012749758
- D.DeandreisA.Al GhuzlanA.AuperinIs 18F-fluorodeoxyglucose–PET/CT useful for the presurgical characterization of thyroid nodules with indeterminate fine needle aspiration cytology?Thyroid2222012165172
- D.S.CooperG.M.DohertyB.R.HaugenAmerican thyroid association guidelines taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancerThyroid1622006109142
- R.PaschkeL.HegedusE.AlexanderThyroid nodule guidelines: agreement, disagreement and need for future researchNat Rev Endocrinol72011354361
- P.TrimboliR.GuglielmiS.MontiUltrasound sensitivity for thyroid malignancy is increased by real-time elastography: a prospective multicenter studyJ Clin Endocrinol Metab9712201245244530
- C.AsteriaA.GiovanardiA.PizzocaroUS-elastography in the differential diagnosis of benign and malignant thyroid nodulesThyroid1852008523531
- F.S.FerrariA.MegliolaA.ScorzelliUltrasound examination using a contrast agent and elastography in the evaluation of single thyroid nodules: preliminary resultsJ Ultrasound1120084754
- C.AsteriaA.GiovanardiA.PizzocaroUS-elastography in the differential diagnosis of benign and malignant thyroid nodulesThyroid182008523531
- W.PhuttharakC.SomboonpornG.HongdomnernDiagnostic performance of gray-scale versus combined gray-scale with colour doppler ultrasonography in the diagnosis of malignancy in thyroid nodulesAsian Pac J Cancer Prev102009759764
- R.E.MohamedK.A.AbodewanDiagnostic utility of real-time ultrasound elastography for prediction of malignancy in solid thyroid nodulesEgypt J Radiol Nucl Med44120133343
- C.ShuzhenComparison analysis between conventional ultrasonography and ultrasound elastography of thyroid nodulesEur J Radiol81201218061811
- M.C.FratesC.B.BensonJ.W.CharboneauManagement of thyroid nodules detected at US: society of radiologists in ultrasound consensus conference statementRadiology2372005794800
- J.K.HoangW.K.LeeM.LeeUS features of thyroid malignancy: pearls and pitfalls 1Radiographics272007847
- G.AnilA.HegdeF.H.ChongThyroid nodules: risk stratification for malignancy with ultrasound and guided biopsyCancer Imag: Off Publ Int Cancer Imag Soc112011209223
- W.J.MoonJ.H.BaekS.L.JungUltrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendationsKorean J Radiol122011114
- J.A.BonavitaJ.MayoJ.BabbPattern recognition of benign nodules at ultrasound of the thyroid: which nodules can be left alone?AJR Am J Roentgenol1932009207213
- M.DigheU.BaeM.L.RichardsonDifferential diagnosis of thyroid nodules with US elastography using carotid artery pulsationRadiology24822008662669
- U.BaeM.DigheT.DubinskyUltrasound thyroid elastography using carotid artery pulsation: preliminary studyJ Ultrasound Med2662007797805
- Y.HongX.LiuZ.LiReal-time ultrasound elastography in the differential diagnosis of benign and malignant thyroid nodulesJ Ultrasound Med: Off J Am Inst Ultrasound Med282009861867
- A.M.McNicolPathology of thyroid tumoursSurgery (Oxf)25112007458462
- T.RagoG.Di CoscioF.BasoloCombined clinical, thyroid ultrasound and cytological features help to predict thyroid malignancy in follicular and Hϋrthle cell thyroid lesions: results from a series of 505 consecutive patientsClin Endocrinol (Oxf)66120071320
- Z.V.MaizlinS.M.WisemanP.VoraHurthle cell neoplasms of the thyroid: sonographic appearance and histologic characteristicsJ Ultrasound Med2752008751757
- V.CantisaniV.D’AndreaF.BiancariProspective evaluation of multiparametric ultrasound and quantitative elastosonography in the differential diagnosis of benign and malignant thyroid nodules: preliminary experienceEur J Radiol81201226782683
- R.KagoyaH.MonobeH.TojimaUtility of elastography for differential diagnosis of benign and malignant thyroid nodulesOtolaryngol Head Neck Surg14322010230234
