Abstract
Gorham–Stout disease (GSD) is a rare osteolytic bone disease also known as vanishing bone disease. The pathogenesis of GSD is not well understood. Studies showed that lymphatic and blood endothelial cells in addition to macrophages secrete TNFα and IL-6 that stimulate osteoclast formation with osteolysis. Also TNFα secretion inhibits osteoblast differentiation and new bone formation. It is known that cytokines such as TNFα, IL-1 and complement system activation are responsible for inflammation and necrosis in the vessel wall at vasculitis. Both diseases have similar pathogenesis. Here, we presented a case of Gorham’s disease with involvement of bilateral humerus, systemic arterial thrombosis and mesenteric vasculitis.
1 Introduction
Gorham–Stout disease (GSD) is a rare osteolytic bone disease also known as vanishing bone disease. It is an musculoskeletal disorder characterized by spontaneous and progressive osteolysis, angiomatous proliferation and soft tissue swelling without new bone formation, although first description of a humerus osteolysis in 1838 by Jackson. Moreover, in 1955, Gorham and Stout published a paper, which correlated the massive osteolysis noted in the disease with hemangiomatosis.Citation1 The pathogenesis of GSD is not well understood. Studies showed that lymphatic and blood endothelial cells in addition to macrophages secrete TNFα, IL-1β and IL-6 that stimulate osteoclast formation with osteolysis.Citation2,Citation3 Also TNFα secreted by macrophage and endothelial cells inhibits osteoblast differentiation and new bone formation. Additionally, the signaling pathway of the receptor of the lymphangiogenic growth factor Platelet Derived Growth Factor BB(PDGFR-b) and vascular endothelial growth factor (VEGF) family has the critical role that could play in the pathogenetic mechanism of the disease.Citation4,Citation5 Besides the bone disease, also lymphatic vascular malformations involving the skin and the soft tissues can be adjacent to the diseased bone.Citation4 It can affect any part of the skeleton. The sites most affected are the cranium, shoulder and pelvis.Citation6 GSD shows no preference for gender or race and occurs more often in children and young adults. Although dissolution, fracture, fragmentation and disappearance of a part of a bone are typical at X-ray diagnosis of GSD is based on exclusion of other causes of osteolysis, such as infection, cancer, inflammatory and endocrine disorders.Citation7
Herein, we report a 50 years old female patient who had been presented with osteolysis of bilateral humerus, systemic thrombosis and mesenteric vasculitis.
2 Case report
A 50 year-old woman was admitted to the hospital having abdominal pain and anemia to find etiology of osteolysis of humerus. Her shoulder pain had started five years earlier with progressive loss of range of motion. She did not have any previous history of trauma but she was treated because of soft tissue infection. There were no document neither tissue nor blood culture positivity.
At the objective examination she presented with pain upon palpation of bilateral shoulder. She also could not raise left upper arm and right upper arm was limited to internal and external rotation, abduction and adduction. At her abdominal examination she had diffuse defence without rebound.
She underwent X-ray examination with the right and left shoulder (). X-ray showed the right humerus radiolucent foci (osteolytic lesions) and loss of tissue and left humerus proximal resorption of bone. MRI on bilateral humerus () also showed complete bone resorption of left humerus head and neck and scapula’s glenoid process and partial bone resorption of right humerus. Bilateral shoulder muscles widespread lipoid atrophy was seen. Her blood chemistry, parathyroid and thyroid hormone levels, serum immunoglobulins, complement levels, and tumor markers were all normal (). She had iron deficiency anemia and mild leukocytosis. Sedimentation rate was high and also she had anti nuclear anticor (ANA) positivity (1/320 titer). Lupus anticoagulants and hereditary thrombophilia tests were negative except for PAI heterozygosity (). Her Schirmer test was negative and salivary gland biopsy was normal. Her upper and lower endoscopy was normal except for gastritis.
Figure 1 Bilateral humerus X-ray. X-ray showed that right humerus radiolucent foci(osteolytic lesions) and loss of tissue and left humerus proximal resorption of bone.
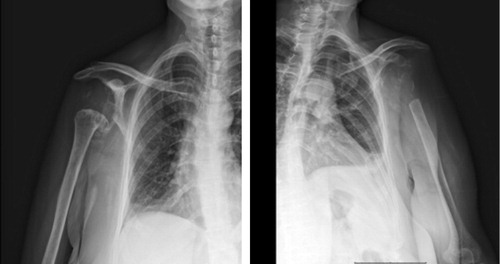
Figure 2 Bilateral humerus MRI of patients. MRI showed complete bone resorption of left humerus head and neck and scapula’s glenoid process and partial bone resorption of right humerus. Bilateral shoulder muscles widespread lipoid atrophy was seen.
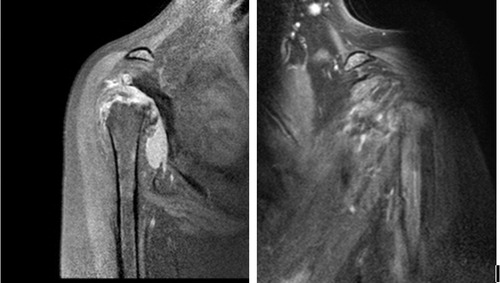
Table 1 Laboratory tests.
Table 2 Immunologic tests.
Thorax CT showed thrombus in right subclavian artery and aorta and third costa focal bone destruction with normal pulmonary parenchyma. Abdominal CT angiography showed thrombus in left common iliac artery, mesenteric vasculitis, ileal wall thickness and partial intestinal obstruction. To exclude hematologic malignancy bone marrow aspiration and biopsy were performed. It was negative for malignancy and dysplasia.
She underwent humerus biopsy and culture. Her biopsy was reported nonspecific minimal chronic inflammatory process. Tissue tuberculosis and aerobe culture were both negative.
We started 1 mg/kg/day metilprednizolone as a treatment of vasculitis. After one month follow-up she had no abdominal pain and her acute phase reactants were normal. The second month of discharge she admitted to emergency department with acute abdominal pain and diffuse abdominal defence and rebound. Her abdominal CT showed intestinal perforation. After surgery she died because of septic shock.
3 Discussion
GSD is a rare condition that is characterized by loss of bone matrix, which is replaced by fibrotic tissue and proliferation of vascular and lymphatic canals. There is no association between GSD and vasculitis and thrombosis in the literature. We can also not explain the bone findings of our patient with vasculitis. Patient’s X-ray and MRI findings are appropriate with GSD but lymphatic malformation and nonmalignant hyperproliferation of small vessels have not seen in bone biopsy taken from the patient. Presence of multiple thrombosis, mesenteric vasculitis and ANA positivity was considered systemic lupus erythematosus (SLE) but not enough to diagnose SLE to Systemic Lupus International collaborating clinics classification criteria for systemic lupus erythematosus.Citation8 In SLE, lupus vasculopathy is found in up to 40% patient especially woman and typically characterized by inflammation and necrosis in the vessel wall.Citation9 It is known that cytokines such as TNFα, IL-1 and complement system activation are responsible for inflammation and necrosis in the vessel wall.Citation10 Also TNFα, IL-1β and IL-6 stimulate osteoclast formation with osteolysis and the other way is TNFα inhibits osteoblast activation and new bone formation at GSD.Citation2,Citation3 Experimental animal models showed that, TNFα infusion was rapidly followed by thrombin generation and the study with the colorectal cancer patients also showed association between TNFα levels and venous thromboembolism risk.Citation11 Chronic inflammation or autoinflammatory diseases are also possible cause of thrombosis.Citation12
In a study conducted by Franchi et al. to find a diagnostic marker for GSD, CD105 expression was found to be significantly higher in GSD vessels compared to control group.Citation13 Similarly, CD105 (endoglin) expression was significantly higher in systemic vasculitis and the expression of it correlates with disease activity.Citation14–Citation16
As a major molecule in angiogenesis, VEGF also contributes to the regulation of the immune system.Citation17 Significantly increased levels of VEGF were demonstrated in activation of vasculitis as well as in GSD.Citation2,Citation3,Citation18
4 Conclusion
TNFα, IL-1β, IL-6, VEGF and CD105 have pathophysiological role both in the vasculitis and in the GSD. This common pathway increases the risk of coexistence of both diseases. Thrombosis may be the result of direct effect of cytokines such as TNFα or chronic inflammation or autoinflammation. To our knowledge this report is the first combination of GSD, arterial thrombosis and vasculitis in the literature. Perhaps it is a new entity on the basis of vasculopathy including vasculitis, thrombosis and GSD like disease.
5 Conflict of interest
The authors declare that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 25 May 2016
References
- Y.LiuD.-R.ZhongP.-R.ZhouGorham–Stout disease: radiological, histological, and clinical features of 12 cases and review of literatureClin Rheumatol2014111
- T.FaruqiN.DhawanJ.BahlMolecular, phenotypic aspects and therapeutic horizons of rare genetic bone disordersBioMed Res Int2014
- S.ColucciG.TarabolettiL.PrimoGorham–Stout syndrome: a monocyte-mediated cytokine propelled diseaseJ Bone Miner Res2122006207218
- J.HagendoornT.P.PaderaT.I.YockPlatelet-derived growth factor receptor-β in Gorham’s diseaseNat Clin Pract Oncol3122006693697
- R.VenkatramaniN.S.MaP.PitukcheewanontGorham’s disease and diffuse lymphangiomatosis in children and adolescentsPediatr Blood Cancer5642011667670
- P.SáP.MarquesC.OliveiraGorham’s disease: clinical caseRevista Brasileira de Ortopedia (English Edition)5022015239242
- V.S.NikolaouD.ChytasD.KorresVanishing bone disease (Gorham–Stout syndrome): a review of a rare entityWorld J Orthoped552014694
- M.PetriA.M.OrbaiG.S.AlarcónDerivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosusArthritis Rheum648201226772686
- M.Veller16· Pathophysiology and principles of management of vasculitides and Raynaud’s syndromeMech Vasc2952011
- H.M.BelmontS.B.AbramsonJ.LiePathology and pathogenesis of vascular injury in systemic lupus erythematosus. Interactions of inflammatory cells and activated endotheliumArthritis Rheum3911996922
- M.RoselliP.FerroniC.RolfoTNF-α gene promoter polymorphisms and risk of venous thromboembolism in gastrointestinal cancer patients undergoing chemotherapyAnn Oncol2013 mdt251
- M.La ReginaF.OrlandiniR.MannaAutoinflammatory diseases: a possible cause of thrombosis?Thrombosis J131201519
- A.FranchiF.BertoniP.BacchiniCD105/endoglin expression in Gorham disease of boneJ Clin Pathol6222009163167
- U.ErdbrueggerM.GrossheimB.HertelDiagnostic role of endothelial microparticles in vasculitisRheumatology4712200818201825
- P.BroganV.ShahC.BrachetEndothelial and platelet microparticles in vasculitis of the youngArthritis Rheum5032004927936
- P.A.BroganM.J.DillonEndothelial microparticles and the diagnosis of the vasculitidesInt Med4312200411151119
- Y.HamamichiF.IchidaX.YuNeutrophils and mononuclear cells express vascular endothelial growth factor in acute Kawasaki disease: its possible role in progression of coronary artery lesionsPediatr Res49120017480
- G.G.SongJ.-H.KimY.H.LeeVascular endothelial growth factor gene polymorphisms and vasculitis susceptibility: a meta-analysisHum Immunol7562014541548
