Abstract
Background
There is need for information on the medical care seeking behaviour of Nigerian doctors.
Purpose
This work was therefore designed to study the medical care seeking behaviour of Nigerian doctors in Nigeria.
Methods
It was a cross-sectional survey among doctors in Nigeria.
Results
Data from 522 doctors were included in the analysis. Majority of them (80.5%) had one form of illness or the other in the year preceding the survey. Only 35% of them reportedly consulted another doctor during their illness. Most of the consultations (61.2%) were informal in the form of over the phone (45.6%), Corridor (33.3%) and home visit (21.1%) and just 18.4% of the consultations occurred within 24 h of onset of illness. A low 19.5% of them had a regular source of medical care. Screening for illnesses was generally below expectation. Just 6 out of the 436 (1.4%) male doctors had screened for prostate cancer while 39 out of 86 (45.3%) females had screened for cervical cancer. A significantly higher proportion of general practitioners (p = 0.01) and doctors above 45 years of age (P = 0.004) consulted informally. Higher proportion of general practitioners and resident doctors based their consultations on their familiarity with the doctors consulted (p = 0.001) and privacy during consultation (p = 0.001). Delay in consultation for more than 24 h after onset of illness was more likely in those above below the age of 45 years (p = 0.001).
Conclusion
This study has shown that Nigerian doctors are often reluctant patients who frequently tend to delay medical care. The teaching of appropriate medical care seeking behaviour should be incorporated into medical curriculum in Nigeria.
1 Introduction
Doctors are reluctant patients who tend to delay seeking help for their health problems and find it difficult to adopt the role of the patient.Citation1,Citation2 Although previous studies have suggested that doctors have lower standardised mortality rate than the general population, their rates of chronic illnesses and preventive health challenges are similar to the general community.Citation3 However, the rates of chronic sicknesses in doctors is likely underestimated since they may be overlooked because of self-medication and unwillingness of doctors to assume the role of a patient.Citation4 Sick doctors are exceptional patients because they have the knowledge and skills to be able to treat themselves, but unfortunately being exceptional does not necessarily ensure better care. Furthermore, doctors may be unwilling to consult their own colleagues in the usual way and either engage in self-treatment or seek an inadequate consultation with a colleague.Citation5 Many studies have also shown that when doctors experience ill health, they ignore the advice they offer to their patients.Citation6,Citation7 Consequently, the medical community has developed a culture in which working through illness and self-treating is the norm.Citation2,Citation8 The impact of illnesses may be further exasperated by a culture that discourages admission of health vulnerabilities among doctors.Citation9
Even when doctors do seek external care, evidence suggests they receive a lesser quality of care than lay patients.Citation9,Citation10
Many doctors find it difficult to enter the patient’s role for various personal and systemic reasons, such as time pressure, the stigmatizing nature of sickness, worries about bothering or letting down colleagues, fear of showing weakness or lack of medical knowledge, concerns about confidentiality and fear of restriction of medical licensing.Citation8,Citation9,Citation11,Citation12 The behaviour of doctors towards their own illnesses and their relationship with their colleagues endanger their health.
Studies on several aspects of doctors’ health problems have been published in various countries.Citation2, Citation4–Citation7 Although Agaba et al. published a study on health seeking behaviour of physician at Jos University Teaching Hospital in Nigeria, their report only captured specialists from a single centre and hence cannot be generalised to the entire doctors in Nigeria.Citation13 It is important to have information on the medical care seeking behaviour of Nigerian doctors so that proactive steps can be taken to address any issue relating to their medical care seeking behaviour. This work was therefore designed to study the medical care seeking behaviour of doctors in Nigeria.
2 Subjects and methods
The present study was a cross-sectional survey among doctors in Nigeria. We were unable to do online survey because of lack of reliable database for doctors in Nigeria. Data were collected at two different times. First sample collection was done among doctors in Ilorin, the Kwara state capital, by multistage sampling technique. Stratification was done based on hospital settings (private and public). Since there was no reliable database, participants were recruited during visits to the hospitals by trained assistances under the supervision of one of the co-authors (SAG). All consenting doctors in all the private hospitals in Ilorin metropolis were recruited into the study. A total of 58 consenting doctors from the private hospitals satisfactorily completed and returned the questionnaires (out of the 60 questionnaires administered). The public hospitals were stratified into departments and specialities. Thereafter, simple random sampling technique by balloting for ‘yes’ or ‘no’ was used to select eligible consenting respondents from the different departments. Those who selected ‘yes’ were recruited into the study. A total of 120 doctors were recruited from the public hospitals in Ilorin out of which 118 completed and returned the questionnaires.
The second sample collection was done among consenting doctors from other parts of Nigeria (excluding doctors from Kwara state) during the Annual National Conference of the National postgraduate Medical College of Nigeria and the West African College of Physicians and Surgeons. Consecutive conference participants who were willing to participate in the study were recruited at arrival for the conferences. A total of 174 doctors returned completed questionnaires (out of 175 administered) during the conference of National Postgraduate Medical College of Nigeria while 172 doctors out of the 175 contacted during the West Africa College of Physicians and Surgeons participated in the study by returning completed questionnaires.
The minimum sample size was estimated using the formula, n = Z2Pq/E2 where Z is standard normal deviate = 1.96 at p = 0.05, P = proportion in the target population estimated to have a population characteristics (set at 0.5 for this study), q = (1−P) and E = acceptable margin of error. We assumed a response rate of about 80% and the minimum sample size was estimated to be about 500. We administered 540 questionnaires out of which 522 were completed and returned.
A self-administered structured questionnaire adapted from previous studiesCitation4,Citation11 was used to collect data from the respondents. The questionnaire sought to obtain information on age, gender, areas of specialisation, types of illness experienced in the preceding year, whether or not another doctor was consulted, nature of consultation (formal or informal), and reasons for choice of doctors consulted. The participants were also asked whether they had regular source of medical care and finally, whether they had screened for diabetes mellitus, HIV, cancers (cervical cancer for females and prostate cancer for males), hypertension and hyperlipidemia.
Data analysis was done by SPSS version 15.0. The age was summarised as mean ± standard deviation while frequencies and percentages were used to describe the categorical variables. Test of significance for comparison of the different categories (professional category and age groups) was done using the Chi-square test. Significance level was set at P value < 0.05.
Ethical approval for this study was obtained from the Ethical Review Committee of the University of Ilorin Teaching Hospital.
3 Results
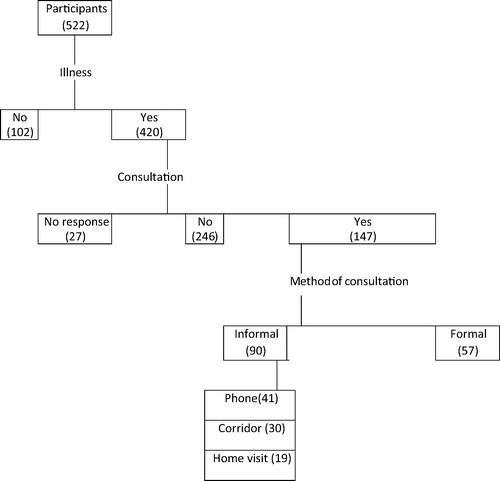
The flow chart for the participants is shown in . Males constituted 83.5% of the studied doctors. Majority of them (78.7%) were married. The mean age was 39.3 ± 9.4 years with a range of 26–61 years. Two hundred and six (39.5%) were in the >25 − <45 year age group, and 284 (54.4%) were >45 years while 32 (6.1%) did not indicate their age. More than two third (342; 65.5%) of them were specialists while the rest were general practitioners (92; 17.2%) and resident doctors in training (88; 17.3%).
As shown in , majority of them (420; 80.5%) reported that they had one form of illness or the other in the year preceding the survey. Only 35% of them reportedly consulted another doctor during their illness whereas 58.6% (246) did not do that and 6.4% failed to indicate whether or not they consulted any doctor. Most of the consultations (90; 61.2%) were informal in the form of over the phone (41; 45.6%), Corridor (30; 33.3%) and home visit (19; 21.1%). Thirty-two (21.8%) of the consultations were based on the expertise of the physicians consulted and just 18.4% (27) of the consultations occurred within 24 h of onset of illness. The various reasons for delay or failure to consult are shown in .
Table 1 Characteristics of the participating doctors.
Of the 522 doctors surveyed, less than one fifth of them (19.5%) had a regular source of medical care. Screening for illnesses such as diabetes, HIV, cancers, hypertension and hyperlipidemia is also highlighted in . Just six out of the 436 male doctors had screened for prostate cancer while 39 out of 86 (45.3%) females had screened for cervical cancer.
(A and B) highlights the health seeking behaviour of the doctors according to their professional category and age groups. A significantly higher proportion of general practitioners consulted informally (p = 0.01) especially over the phone (p = 0.001). Similarly, higher proportion of doctors above 45 years of age consulted over the phone (p = 0.004) compared with those below 45 years (A).
Table 2 Health seeking behaviour of the studied doctors according to their professional category and age groups.
On the reason for the choice of doctors consulted, higher proportion of general practitioners and resident doctors based their consultations on their familiarity with the doctors consulted (p = 0.001) and privacy during consultation (p = 0.001). Delay in consultation for more than 24 h after onset of illness was more likely in those below the age of 45 years (p = 0.001) as highlighted in A.
Various reasons were given for delay or failure to consult another doctor for treatment during illness. A significantly higher proportion of general practitioners delayed because they did not consider their illness serious (p = 0.001) and did initial self-treatment (p = 0.03). Similarly, higher proportion of those above 45 years delayed because of initial self-treatment (p = 0.003) whereas lack of time (p = 0.001) and concern about confidentiality (p = 0.001) were the reasons in a higher proportion of resident doctors. This is displayed in B.
presents the information on screening for diseases among the doctors according to their professional category and age groups. Significantly higher proportion of those above 45 years reported that they had screened for diabetes (p = 0.001) and HIV (p = 0.001) while higher proportion of those below 45 years had screened for hypertension. The general practitioners were more likely to have ordered the screening for themselves (p = 0.001) whereas the screening was ordered by another doctor in a significantly higher proportion of those above 45 years (p = 0.001).
Table 3 Screening for diseases among the Doctors according to their professional category and age groups.
4 Discussion
Our study has clearly shown that the medical care seeking behaviour of Nigerian doctors is below expectation and contrary to the advice they offer to their patients. In spite of the fact that about 80% of the doctors surveyed disclosed that they had one form of illness or the other in the year preceding our survey, a ridiculously low 35% of them reportedly consulted another colleague for treatment. Even then, more than two-third of the consultations were informal.
Our findings confirm previous reports that doctors are usually perturbed when they adopt the role of patient and they often jettison the advice they offer to their patients when they themselves experience ill health.Citation2,Citation14,Citation15 The rate of informal consultations in our study is higher than that reported earlier by Campbell and DelvaCitation16 as well as Rennert et al.Citation7 Informal consultations appear to be commoner than formal care, usually in the form of corridor consultations.Citation7,Citation16,Citation17 Informal consultations (such as on the corridor, over the phone or even in the colleague’s home) are inappropriate, unprofessional, lack objectivity, and may lead to wrong diagnosis, unsatisfactory quality of care, ineffective treatment and worsening of the illness with dangerous consequences. Another disturbing finding from this study is the fact that only about 1 in 5 of those that consulted a doctor based their consultations on the expertise of the doctor consulted. Factors such as familiarity/closeness to the doctors consulted, privacy and other unimportant reasons were given priority, especially by the general practitioners and resident doctors, when choosing the doctors consulted. This behaviour is unexpected from doctors who should understand that consultation is more related to the nature of illness/expertise of the doctor.
Despite the low rate of consultations during illness, more than 80% of the doctors delayed consultations for more than 24 h (even beyond 2 weeks) for various reasons such as illness not considered serious, initial self-treatment, lack of time and concern about confidentiality. This is further worsened by the fact that these unexpected behaviours were commoner in the specialists and older doctors. Self-treatment, lack of time and concern about confidentiality have been widely reported as significant barriers to doctors’ access to quality medical care.Citation7,Citation11,Citation18–Citation20 Apart from encouraging delay in seeking timely care, these factors also tend to augment informal consultations. These factors may also promote the culture of working through illness and late presentation with serious consequences.Citation13,Citation21,Citation22
An unacceptably low 19.5% of the doctors reportedly have regular source of medical care. This is exceptionally low compared to reports from Campbell and Delva, Davidson and Schattner, as well as Forsythe et al. but similar to those of Schneider et al.Citation5,Citation16,Citation18,Citation23 The disparity is likely to be a reflection of the different national health systems in the countries where the studies were conducted. In our country, there is lack of policy on patient registration with a general practitioner unlike in the UK where the national health system requires compulsory patient registration with a general practitioner.
Doctors generally counsel their patients on the need for preventive measures and hence one expects them to take it serious for themselves. Our study however reveals that Nigerian doctors do not adhere strictly to the advice they give to patients. Screening for diseases was less than expected among the doctors surveyed. The highest percentages of screening were for hypertension, HIV and diabetes but unfortunately they were all less than 80%. One would have expected at least more than 90% of the doctors to have been screened for these diseases. The fact that the screening for these diseases was less than expected is not good enough but the fact that screening for cancers was abysmally low is of serious concern. Only 1.4% of the 436 males surveyed had reportedly screened for prostate cancer and less than 50% of the females had ever screened for cervical cancer. Being a doctor does not remove the preventive need of an individual and one would have expected doctors to show good example by practising what they advise their patients to do. This suggests that having knowledge of what should be done does not necessarily imply that correct thing will be done. We also observed that more than one third of the doctors, especially general practitioners and younger doctors ordered the screening for themselves. This is also worrisome because they may choose not to take appropriate steps if they consider the results of the screening as being unfavourable. For example, if the screening for HIV is positive, they may keep the results to themselves rather than seeking appropriate timely care.
The age and sex distribution of this report are reflective of the Nigerian doctors but the professional category is skewed to the specialists owing to the method of data collection. We decided to collect a sizeable proportion of the data during the annual conferences of the postgraduate colleges in Ilorin so as to capture doctors from all over Nigeria as much as possible. Skewed nature of the survey participants will definitely limit the generalisability of our study results. It is also important to emphasise that this study was based on self-report of the participants who were present during the survey. They might have under- or over-reported their behaviour and the impact of report from other doctors who were not captured is difficult to predict. In spite of these shortcomings, we have been able to report on the behaviour of Nigerian doctors when they experience ill health as well as their adherence to screening for diseases. We are able to confirm that Nigerian doctors are not better than their counterparts elsewhere especially as regards their medical care seeking behaviour in health and sickness.
Conclusion: Our study has shown that Nigerian doctors are often reluctant patients who tend to delay seeking medical care. We recommend that they should avoid informal consultations, avoid delay in seeking medical care when ill, avoid working through illness, have their own general practitioners/source of regular medical care, and imbibe preventive health cultures through appropriate screening for diseases. The teaching of appropriate health-seeking behaviour should be part of medical curriculum in Nigeria.
Conflict of interest
None.
Funding
Study funded by the researchers.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 14 May 2016
References
- R.TyssenHealth problems and use of health services among physicians: a review article with particular emphasis on Norwegian studiesInd Health452007599610
- C.M.LinC.H.YangG.C.SungC.Y.LiRisks and causes of hospitalizations among physicians in TaiwanHealth Services Res4322008675692
- M.P.KayG.K.MitchellC.B.Del MarDoctors do not look after their own physical healthMed J Aust18172004368370
- A.J.MontgomeryC.BradleyA.RochfoprtE.PanagopoulouA review of self-medication in physicians and medical studentsOccup Med6172011490497
- M.SchneiderM.B.GallacchtC.GoehringB.KunziP.A.BovierPersonal use of medical care and drugs among Swiss primary care physiciansSwiss Med Wkly1372007121126
- H.GranthamDoctors as patient. Part 2: the realities of life as a patientAust Fam Physician312002179181
- M.RennertL.HagoelL.EpsteinG.ShifroniThe care of family physicians and their families: a study of health and help-seeking behaviourFam Pract719909699
- W.T.ThompsonM.E.CupplesC.H.SibbettD.I.SkanT.BradleyChallenge of culture, conscience, and contract to general practitioners care of their own health: qualitative studyBMJ3232001728731
- C.CenterM.DavisT.DeltreD.E.FordW.HansbroughH.HendinConfronting depression and suicide in physiciansJAMA289200331613166
- F.FoxM.HarrisG.TaylorK.RodhamJ.SuttonB.RobinsonWhat happens when doctors are patients? Qualitative study of GPsBr J Gen Pract592009811818
- E.O.RosvoldE.BjertnessIllness behaviour among Norwegian physiciansScand J Public Health302002125132
- E.O.RosvoldR.TyssenShould physicians’ self-prescribing be restricted by law?Lancet365200513721374
- P.A.AgabaA.N.OchekeM.O.AkanbiC.A.DaniyamS.O.UgoyaE.N.OkekeHealth seeking behaviour of physicians at Jos university teaching hospitalNig Med J52220119094
- E.FrommeR.HebertJ.CarreseSelf-doctoring: a qualitative study of physicians with cancerJ Fam Pract5342004299306
- M.GardnerJ.OgdenDo GPs practice what they preach? A questionnaire study of GPs’ treatments for themselves and their patientsPatient Educ Counselling562004112115
- S.CampbellD.DelvaPhysician do not heal thyself. Survey of personal health practices among medical residentsCan Fam Physician49200311211127
- P.BaldwinM.DoddR.M.WrateYoung doctors’ health-II. Health and health behaviourSoc Sci Med45119974144
- S.DavidsonP.SchattnerDoctors’ health-seeking behaviour: a questionnaire surveyMed J Aust17962003302305
- C.McKevittM.MorganAnomalous patients: the experiences of doctors with an illnessSociol Health Illn1951997644667
- G.N.UallachainAttitudes towards self-health care: a survey of GP traineesIr Med J10062007489491
- E.HemG.StokkeR.TyssenN.T.GronvoldP.VaglumO.EkebergSelf-prescribing among young Norwegian doctors: a nine-year follow-up study of a nationwide sampleBMC Med320051610.1186/1741-7015-3-16 Available from: http://www.biomedcentral.com/1741-7015/3/16 (Accessed May 2013)
- S.A.SchneckDoctoring doctors and their familiesJAMA280199820392042
- M.ForsytheM.CalnanB.WallDoctors as patients: postal survey examining consultants and general practitioners adherence to guidelinesBMJ31972101999605608