1 Introduction
Incidence of extracranial carotid aneurysms is low.
Usually the lesion develops from internal carotid artery, whereas only 2% of lesions develop from the external artery.
The main causes are atherosclerosis and traumatic events.Citation1
Occasionally in Marfan syndrome an extracranial carotid aneurysm can occur.Citation2
Here we describe the case of a 62-year-old woman with an aneurysm of the right internal carotid artery, and revise the techniques used to treat it nowadays.
2 Case report
A 62 year-old woman, affected by Marfan Syndrome, was admitted to our Hospital due to an aneurysm of the right extracranial internal carotid artery.
In the past medical history we found clinical features of Marfan syndrome, both cardiac (mild aneurysmatic dilation of the aortic bulb with a diameter of 46 mm, mild-severe mitral insufficiency and mild tricuspid insufficiency) and ocular (glaucoma, right cataract and previous interventions for bilateral retinal rupture and left cataract). Medical history was nonetheless not significant like family history.
At the clinical examination the patient presented a right painless, elastic and pulsing laterocervical mass with a diameter of 2.5 cm.
The lesion was completely asymptomatic.
No previous history of neurological symptoms or cervical trauma was reported. No symptoms were identified possibly related to mycotic infections.
Diagnosis was made by US scan that demonstrated the origin from the carotid bifurcation, but did not identify the vessel mainly involved.
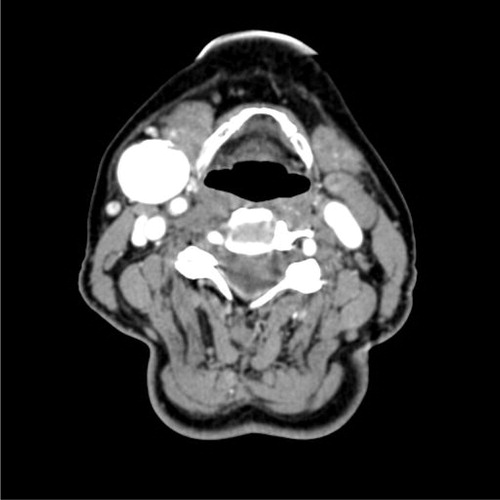
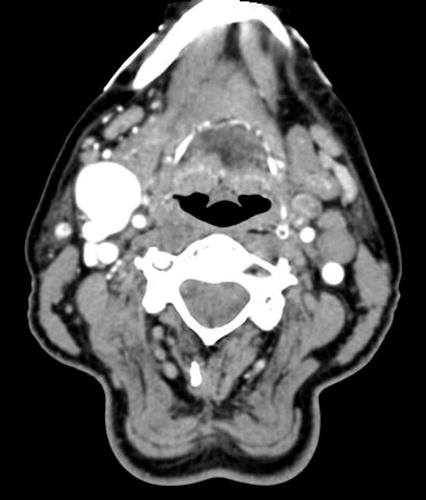
So the patient underwent a CT scan of the sovraortic trunks, that demonstrated a very coiled kinking of the right internal carotid artery, immediately after its origin along with an aneurysm 20 mm in diameter with an intraluminar thrombus. At the same level an atherosclerotic plaque was described, without hemodynamic interference. No other vascular lesions were identified (See and ).
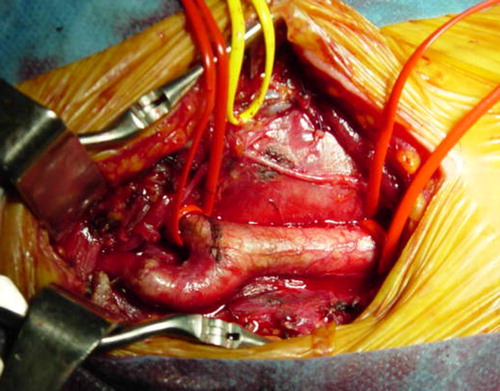
The patient underwent surgery under general anesthesia with intraoperative SEP (somatosensory evoked potential) monitoring. The procedure was performed through the usual laterocervical access, consisting of aneurysmectomy with end-to-end anastomosis (See –).
No neurological intraoperative or postoperative events were observed.
The postoperative course was uneventful and the patient was discharged after four days with antiplatelet agents.
At five years of follow up the patient is asymptomatic and still under antiplatelet agents; the Duplex Doppler Ultrasonography demonstrates a regular flow through the carotid artery.
Up to now the patient hasn’t presented new signs of Marfan syndrome.
3 Discussion
3.1 Incidence
As mentioned, incidence of extracranial carotid aneurysms is low.
DeBakey’s group described only 37 carotid aneurysms out of a total of 8500 aneurysms which underwent surgery over 20 years.Citation3
In a literature review Schechter reported 853 cases till 1977.Citation4
In more recent literature only case reports of no more than 2 patients are reported.
The first one to describe a successful intervention for carotid aneurysm (a proximal ligature) was Cooper in 1808: the patient died 13 years after the procedure.
The first reconstructive intervention was performed in 1952; since then the number of cases reported has increased significantly.
At present about 1% of the interventions performed on extracranial carotid artery are due to aneurysms.Citation1,Citation5
3.2 Etiology and natural history
The most relevant causes are atherosclerosis and traumatic events.
Atherosclerotic aneurysmsCitation6,Citation7 are usually found in hypertensive elderly patients. They are usually fusiform and involving the bifurcation more frequently than other sites. They can be bilateral and an intracranial carotid aneurysm with the same pathogenesis can coexist.
Traumatic eventsCitation5 represent the second more common cause. After a blunt trauma or a distractive trauma such as in case of sudden hyperextension of the neck along with rotation there can be a damage to the middle layer of the vessel. Traumatic aneurysms can also occur after carotid surgery. Aneurysms in such cases are more often saccular and they usually involve the common carotid or the distal part of internal carotid artery beyond the base of the skull. This happens because the carotid artery is quite fixed at the cranium in its passage through it, so that the distal tract is at a higher risk of damage.Citation8
Among less frequent causes there are syphilis, cystic medial necrosis, muscular hyperplasiaCitation9 and arteritis such as polyarteritis nodosa, Takayasu arteritis and Wegener arteritis.
We have to cite also mycoticCitation10 aneurysms, occasionally caused by infected embolism in a patient affected by bacterial endocarditis or more frequently by cellulitis or peritonsillarCitation11 or mastoid abscess.
Carotid aneurysms can also occur after irradiation for malignant tumors of the neck; they can be rarely congenital (in this latter case they are usually bilateral).Citation12,Citation13
Finally a carotid aneurysm can occur in Marfan Syndrome.
The loss of elastic tissue within the arterial wall with subsequent weakening is the pathogenic mechanism underlying aneurysms in Marfan syndrome.
Winslow recorded that 4 out of 5 patients treated conservatively died because of a complication: thrombosis, embolization or rupture.
3.3 Clinical presentation
As in the case here described, the more common clinical presentation of a carotid aneurysm is a pulsing, otherwise asymptomatic laterocervical mass.
Even if the aneurysm is rapidly expanding, the patient can remain asymptomatic.
In most cases, diagnosis is quite simple, but carotid aneurysms have to be differentiated from laterocervical lymphadenopathy, branchial cysts and tumors of carotid body.
In case of compression on oropharynx a carotid aneurysm can simulate a peritonsillar abscess.
Moreover every anatomical anomaly that pushes onto surface carotid bifurcation can be clinically similar to a carotid aneurysm.
3.4 Diagnosis
In the most difficult cases such as for the distal extracranial internal carotid aneurysms radiological exams are mandatory.
Diagnosis can be based on US scan and in some cases also CT scan and/or MRI.Citation5
Duplex Doppler Ultrasonography is the first exam to do because it demonstrates carotid bifurcation in almost all cases. A plain X-ray often detects a soft mass possibly with calcifications on its walls.
Even if CT scan or MRI are more important nowadays, diagnostic arteriography remains an important exam in order to establish the right kind of treatment. In fact, arteriography evaluates carotid bifurcation, morphology of lesion, proximal and distal necks, presence of stenosis or kinking.
3.5 Treatment
Treatment of such lesion is usually surgicalCitation14–Citation19: only a few patients undergo conservative treatment (usually patients with important contraindications to surgery with asymptomatic small aneurysms). In fact conservative treatment carries important morbidity, in most cases due to neurological complications or rupture.
Surgical treatment with only ligature was successfully performed for the first time more than 2 centuries ago and it had been the only working option till the half of the last century, when reconstructive surgery was introduced.
Ligature has a high risk of postoperative stroke independently on its site. Even in more recent literature, some authors report a mortality rate greater than 50% and a relative weight of neurological morbidity which is decreasing over time.
In symptomatic aneurysms, when a distal anastomosis or suture is not technically feasible, ligature is the only option.
Two methods have been designed in order to reduce risk of neurological complications after ligature: one consists of gradual occlusion of artery with Selverstone clamp in order to gain development of collateral vessels before complete occlusion is obtained. During this period anticoagulant agents are administered and at the end ligature is performed at the same site where clamp was positioned.
The other method is trying to estimate risk of cerebral damage before ligation, performing it only in patients with low risk. McIvor reported 5 cases of stroke (2 of them fatal) out of 16 patients treated with ligature after a negative balloon test.
Thus, current opinion is that, even with cautions, the high risk of cerebral damage after ligature mandates reconstructive surgery when not strictly contraindicated.
Among different reconstructive procedures the most diffuse is aneurysmectomy with end-to-end anastomosis. It is often feasible, but it requires an adequate length of the two arterial tracts to connect and a certain abundance of vascular tissue. It can permit also correction of associated lesions such as kinking (like in the case here reported). If the two arterial tracts to link after aneurysmectomy are not long enough, the carotid substitution with venous graft or prosthesis (for example PTFE) has to be performed.
Alternatively external carotid artery may be sectioned and its proximal part connected to the distal tract of internal carotid artery after aneurysmectomy.
In rare cases of mycotic aneurysm, antibiotics have to be administered and venous patch has to be preferred to prosthesis because of risk of infection.
Other procedures with limited indications have to be mentioned. Wrapping consists in enveloping the aneurysm in cellophane sleeves or plastic material in order to limit its expansion: it is an obsolete technique that doesn’t reduce the risk of embolization.
Matas’ endoaneurysmorraphy is nowadays useful when a distal anastomosis is not feasible, maintaining temporarily a shunt in the internal carotid artery.
Even endovascular procedures such as stenting or embolization with spirals have been mentioned.Citation17,Citation19,Citation20
3.6 Complications
Except for nerve lesions or local infections, the only serious complication after this kind of surgery is cerebral ischemic damage related to ligature, clamping or embolization.
In order to reduce this complication it’s important to handle carefully the aneurysm during dissection.
Continuos intraoperative EEG and SEP monitoring, evaluation of back pressures and some anesthesiologic cautions are useful to reduce risk of cerebral damage related to clamping.
Risk of cerebral damage is significative even if its estimation is difficult: simple ligature is followed by cerebral damage in 30% of cases, but its incidence is lower after reconstructive surgery.
Neurological complications may vary from massive fatal stroke to minimal accidents with partial or complete functional recovery. Sometimes cerebral damage becomes evident after a long time since surgery. This may relate to occlusion of the reconstruction or late embolization determining distal thrombosis of internal carotid or its branches.
4 Conclusions
Extracranial internal carotid aneurysms are uncommon but they have particular relevance especially because of the risks of cerebral embolic events or (more rarely) rupture. Nowadays surgery is the gold standard of treatment, with specific reference to reconstructive techniques.
Conflict of interest
The authors declare that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
References
- R.El-SabroutD.A.CooleyExtracranial carotid artery aneurysms: Texas Heart Institute experienceJ Vasc Surg312000702712
- R.SztajzelS.HefftC.GirardetMarfan’s syndrome and multiple extracranial aneurysmsCerebrovasc Dis112001346349
- C.H.McCollumW.G.WheelerG.P.NoonAneurysms of the extracranial carotid artery. Twenty-one years’ experienceAm J Surg1371979196200
- D.C.SchechterCervical carotid aneurysms: Part IN Y State J Med791979892901
- J.NordanstigJ.GelinN.JensenK.OsterbergS.StrömbergNational experience with extracranial carotid artery aneurysms: epidemiology, surgical treatment strategy, and treatment outcomeAnn Vasc Surg282014882886
- R.M.ZwolakW.M.WhitehouseJrJ.E.KnakeAtherosclerotic extracranial carotid artery aneurysmsJ Vascular Surg11984415422
- Kaczynski J, Wilczynska M, Blaszczynski M, Fligelstone L. Extracranial saccular atherosclerotic aneurysm of the internal carotid artery (ICA) treated by an oblique end-to-end primary anastomosis. BMJ Case Reports; 2013.
- J.DownerM.NadarajahE.BriggsP.WrigleyW.McAuliffeThe location of origin of spontaneous extracranial internal carotid artery dissection is adjacent to the skull baseJ Med Imaging Radiat Oncol582014408414
- M.A.BartoliG.Sarlon-BartoliB.ChetailleSaccular aneurysm and kink of the extracranial internal carotid artery secondary to fibromuscular dysplasiaJ Vasc Surg62201513261327
- J.B.O’ConnellS.DarcyT.ReilExtracranial internal carotid artery mycotic aneurysmVasc Endovasc Surg432009410415
- J.BrzostA.M.CyranM.WaniewskaM.J.SzczepanskiInternal carotid artery aneurysm mimicking peritonsillar abscessCase Rep Otolaryngol20152015389298
- J.D.KakisisT.G.GiannakopoulosK.MoulakakisC.D.LiapisExtracranial internal carotid artery aneurysmJ Vasc Surg6020141358
- O.GulelM.ElmaliH.T.KeceligilU.YildirimR.UnalGiant extracranial internal carotid artery aneurysmAnn Thorac Surg972014e23
- E.RossetJ.N.AlbertiniP.E.MagnanSurgical treatment of extracranial internal carotid artery aneurysmsJ Vasc Surg312000713723
- N.AttigahS.KülkensN.ZausigSurgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year periodEur Vasc Endovasc Surg372009127133
- G.FaggioliA.FreyrieA.StellaExtracranial internal carotid artery aneurysms: results of a surgical series with longterm follow-upJ Vasc Surg231996587595
- D.AngilettaR.PulliD.MarinazzoSurgical and endovascular treatment of extracranial carotid artery aneurysms: early and long-term results of a single centerAnn Vasc Surg282014 659–64PMID
- G.T.FankhauserW.M.StoneR.J.FowlSurgical and medical management of extracranial carotid artery aneurysmJ Vasc Surg6122015389393
- P.SzopinskiP.CiostekM.KielarA series of 15 patients with extracranial carotid artery aneurysms: surgical and endovascular treatmentEur J Vasc Endovasc Surg292005256261
- J.C.WelleweerdG.J.de BorstD.de GrootBare metal stents for treatment of extracranial internal carotid artery aneurysms: long-term resultsJ Endovasc Ther222015130134