Abstract
The incidence of thyroid dysfunction in diabetic patients is higher than that of the general population. Undiagnosed thyroid dysfunction may affect the metabolic control and enhance cardiovascular, and other chronic complication risks in diabetic patients. Few studies have examined the relationship between subclinical hypothyroidism (SCH) and vascular complications of type 2 diabetes. Objectives: To find out the relationship between SCH and vascular complications in patients with Type 2 diabetes. Subjects and Methods: Our cross sectional study included 110 patients with type 2 DM (45 males and 65 females) who were followed at the Diabetes outpatient Clinics in the state of Kuwait during 6 months period. All patients subjected to complete clinical and laboratory data, including thyroid function tests, total cholesterol (TC), triglyceride (TG), HDL-C, LDL-C, urinary albumin, fundus examination, ECG, and Glycosylated hemoglobin. Results: Among 110 patients, 21 (19.1%) Patients had SCH. Patients with SCH were more significantly older, with longer duration of diabetes, higher HbA1c, total cholesterol and LDL-C than euthyroid group. However, gender (p = 0.076), BMI (p = 0.092), and smoking (P = 0.715) were not significantly different between the SCH and euthyroid groups. The SCH group had a higher prevalence of dyslipidemia (p = 0.017), diabetic nephropathy (p = 0.003) diabetic retinopathy (p = 0.004) and IHD (p = 0.011) than the euthyroid group while no significant difference in the prevalence of diabetic neuropathy (p = 0.420). Conclusions: SCH is a common endocrine disorder in patients with Type 2 diabetes. It could be associated with a higher prevalence of vascular complications in type 2 diabetes. We could not prove a relation between SCH and diabetic neuropathy.
1 Introduction
Subclinical hypothyroidism (SCH) is defined as an asymptomatic state that is characterized by high serum concentration of thyroid-stimulating hormone (TSH) and a normal serum concentration of thyroxine.Citation1 The incidence of thyroid dysfunction in diabetic patients is higher than that of the general population and up to a third of patients with type-1 diabetes (T1DM) and 4–17% in type- 2 diabetic patients. Undiagnosed thyroid dysfunction may affect metabolic control and enhance cardiovascular, and other chronic complication risks in diabetic patients.Citation2 The association between SCH and ischemic heart disease has been noticed in several studies, although the results have been inconsistentCitation3,Citation4 and very few studies have focused on the population with diabetes. Few studies have examined the relationship between subclinical hypothyroidism and microvascular complications in type 2 diabetic patients. To our knowledge, only three studies have investigated the association between SCH and microvascular complications in Type 2 diabetes. Both Yang et al.Citation5 and Kim et al.Citation6 found that SCH was associated with diabetic retinopathy, although not with nephropathy. By contrast, Chen et al.Citation7 reported that patients with Type 2 diabetes and SCH were at increased risk of nephropathy. Moreover, no study to our knowledge has examined the prevalence of neuropathy in association with subclinical hypothyroidism.
Owing to the paucity of data regarding the prevalence of SCH and its potential association with vascular complications in Type 2 diabetes, this study examined the relationship between SCH and vascular complications patients with Type 2 diabetes.
2 Methods
2.1 Patients
Our cross sectional study included 110 patients with type 2 DM (45 males and 65 females) who were followed at the Diabetes outpatient Clinics in the state of Kuwait during 6 months period were subjected to thyroid function test (FT3, FT4, TSH). Patients with known overt hypothyroidism, known overt or subclinical hyperthyroidism and type 1 diabetes mellitus, pregnancy, Postpartum women, patients with pituitary tumor, thyroid carcinoma or severe heart, liver, kidney and brain diseases were excluded from the study.
2.2 Thyroid function tests and definition
Serum thyrotropin (TSH) levels and free thyroxine levels were measured by chemiluminescent immunoassay. Subclinical hypothyroidism was defined as an elevated TSH level (>4.2 mIU/L) and a normal FT4 level (10–23 pmol/L). Euthyroidism was defined as normal levels of all three parameters: free triiodothyronine, free thyroxine and TSH.
2.3 Clinical examination and laboratory measurements
Relevant data about the patients were collected, including age, gender, duration of diabetes, history of hypertension, BMI, systolic and diastolic blood pressure, total cholesterol (TC), triglyceride (TG), HDL and LDL cholesterol. Glycosylated hemoglobin was measured using an ion-exchange HPLC (Merck-Hitachi9100).
2.4 Assessment of diabetic microvascular and macrovascular complication
The patients were diagnosed as having CAD if they had ischemic changes on a resting electrocardiogram (e.g., abnormal Q waves, ST segment depression or inverted T waves), a history of angina, myocardial infarction, or coronary angiography. Diabetic retinopathy was assessed by ophthalmologists and graded according to the International Clinical Classification of Diabetic Retinopathy.Citation8 Diabetic nephropathy was defined as history of diabetes with the presence of albuminuria, impaired glomerular filtration rate, or both.Citation9 A single morning urine sample for albuminuria was taken from subjects and albuminuria defined if equal to or more than 30 mcg/mg Creatinine (mcg/mg Cr).Citation10 Diabetic neuropathy was diagnosed based on abnormalities detected during neuropathic screening test (vibration sense testing, temperature sense, pain perception, monofilament testing and examination of reflexes).
2.5 Statistical analyses
Statistical analyses were performed using SPSS software version 16.0, and results were expressed as mean ± SD. To compare the means between two groups, Student’s t-test was used for normally distributed data and the Mann–Whitney test was used for non-normally distributed data. For categorical comparisons, the chi-square test was used. A P-value < 0.05 was considered to be statistically significant.
3 Result
Our cross sectional study include 110 patients (45 males and 65 females) with type 2 DM were enrolled in our study with the following characteristics, age, 58.9 ± 10.6 (mean ± SD) years; duration of DM, 17.7 ± 10.02 years; BMI, 31.8 ± 6.5 kg/m2; HbA1c, 8.4 ± 1.8%; TC, 4.08 ± 0.93 mmol/l; triglycerides (TG), 1.55 ± 0.76 mmol/l; HDL-C, 1.22 ± 0.38 mmol/l; LDL-C, 2.09 ± 0.75 mmol/l; TSH, 3.02 ± 1.93 mU/l;T4 (15.28 ± 2.07) pmol/l; urinary albumin creatinine ratio (185.27 ± 379.66) mcg/mg Cr. It was found that (105, 95.5%) of patients had dyslipidemia, (43, 39.1%) had diabetic retinopathy, (47, 42.7%) had diabetic nephropathy, (29, 26.4%) had diabetic neuropathy, (37, 33.6%) had IHD, (82, 74.5%) were hypertensive and (28, 25.5%) were smoker. Among 110 patients, 21 (19.1%) had SCH. Patients with SCH were significantly older, with longer duration of diabetes, higher HbA1c, total cholesterol and LDL-C than euthyroid group. However, gender (p = 0.076), BMI (p = 0.092), and smoking (P = 0.715) were not significantly different between the SCH and euthyroid groups (). The SCH group had a higher prevalence of dyslipidemia (p = 0.017), diabetic nephropathy (p = 0.003) diabetic retinopathy (p = 0.004) and IHD (p = 0.011) than the euthyroid group while no significant difference in the prevalence of diabetic neuropathy (p = 0.420) ( & ).
Figure 1 The prevalence of vascular complications in type 2 diabetes patients with and without subclinical hypothyroidism (SCH).
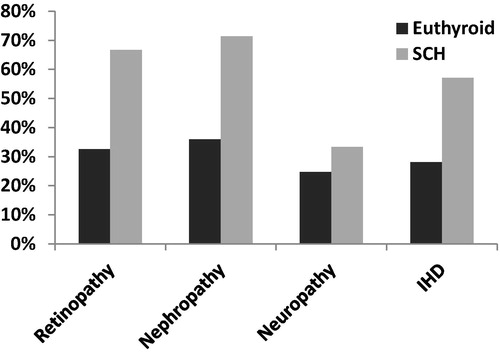
Table 1 Comparison between the participants with Euthyroid and SCH in type 2 diabetic patients regarding the different clinical parameters.
Table 2 The prevalence of vascular complications in type 2 diabetic patients with and without SCH.
4 Discussion
Vascular endothelial dysfunction is supposed to be an important factor in the pathogenesis of microvascular and macrovascular complications in diabetes. Endothelial dysfunction has also been described in subclinical hypothyroidism as well as in those with upper normal TSH values.Citation11,Citation12 The association between microvascular complications and subclinical hypothyroidism and TSH values has not been comprehensively studied. Among the few studies done on the subject, the findings have been opposing. This is a cross-sectional study with a case control analysis which revealed that The prevalence of subclinical hypothyroidism in type 2 diabetic patients was 19.1%, and this is higher than data reported from another study done by Gao et al.Citation13 Our present data revealed that the prevalence of subclinical hypothyroidism was 4.5% in males and 14.5% in females with Type 2 diabetes. NHANES III, a population study, reported that the prevalence of subclinical hypothyroidism was 3.4% in males and 5.8% in females.Citation14 Perros et al. found that the occurrence of subclinical hypothyroidism was 3.3% in men and 4.6% in women with Type 2 diabetes.Citation15 The incidence of subclinical hypothyroidism in our study was greater than those of both these studies and revealed a dominance of females. The patients with SCH had a significant longer duration of diabetes in comparison to the euthyroid group (p = 0.007). In contrast, Kim et al. didn’t found any significant difference in the duration of diabetes between euthyroid and SCH patients.Citation6 Although obesity affects hypothalamic-pituitary-thyroid axis directly or indirectly leading to variations in thyroid function tests,Citation16 there was no significant difference in BMI between SCH diabetic patients and euthyroid group (P = 0.092). In this cross-sectional analysis of type 2 diabetes mellitus, subclinical hypothyroidism was associated with a higher frequency of microvascular (diabetic nephropathy, and retinopathy) and macrovascular complication (IHD). Our result differed from those of Chen et al. study which showed that type 2 diabetic patients with subclinical hypothyroidism are associated with an increased risk of nephropathy and cardiovascular events, but not with retinopathy.Citation7 While Kim et al. showed that SCH was associated with sight-threatening diabetic retinopathy, but not associated with diabetic nephropathy. However, he did not analyze the relationship between SCH and prevalence of macrovascular complications. kim et al. explained the link between SCH and diabetic retinopathy by insulin resistance that was higher in the SCH than the euthyroid group.Citation6 In contrast to, Gao et al. concluded that there is no association between subclinical hypothyroidism, and microvascular complications in type 2 diabetes.Citation17 It is known that thyroid hormone plays an important role in kidney growth and preservation of many of its functions.Citation18,Citation19 In other words, the glomerular filtration rate in hypothyroid patients is approximately one-third lower than the corresponding values in euthyroid individuals.Citation20 Suher et al. suggested that subjects with hypothyroidism may have increased urinary albumin excretion rateCitation21 which came consistence to our result as there was a significant increase in the mean of albuminuria in patients with SCH. Moreover, a study done in Japan by Yasuda et al., subclinical hypothyroidism was associated with albuminuria in type 2 diabetic patients and the TSH level was found to be an independent risk factor for the presence of albuminuria.Citation22 In our study, the prevalence of IHD was significantly higher in patients with SCH than in patients without SCH. Jia et al. provides evidence that SCH in patients with Type 2 diabetes is associated with a high prevalence of CHD.Citation23 This issue can be explained by Overt thyroid hormone deficiency which leads to increases in total cholesterol and LDL–C levelsCitation24 which is evident in our result. Also, thyroid hormone deficiency can also damage vascular function directly.Citation25,Citation26 Furthermore, several researchers have stated that SCH impairs the relaxation of vascular smooth muscle cells, thereby inducing increased arterial stiffness and systemic vascular resistanceCitation25, as well as changes in endothelial function due to decreased nitric oxide availability.Citation26,Citation27 Endothelial dysfunction in SCH could be due to inflammation.Citation28 A higher levels of IL-6, TNF-alpha and high-sensitive C-reactive protein (hs-CRP) in patients with SCH were found. In addition, a low grade chronic inflammation in patients with SCH can also be explained by the autoimmune thyroiditis.Citation29 Although, Hollander et al. demonstrated that renal function was better in 32 patients with hypothyroidism after thyroxine treatment,Citation30 our study was observational, and it does not follow the impact of treatment of subclinical hypothyroidism on risk reduction of diabetic vascular complication. Whether the management of patients with subclinical hypothyroidism affects important cardiovascular outcomes remains an unanswered question.Citation31,Citation32 Chu and Crapo suggested that there was a little or no benefit of thyroxine therapy in most patients with subclinical hypothyroidism.Citation33 However, they also concluded that thyroxine treatment may be beneficial in selected patients with certain clinical circumstances.Citation34
5 Conclusion
SCH is a common endocrine disorder in patients with Type 2 diabetes. It could be associated with a higher prevalence of vascular complication in type 2 diabetes. But, we could not prove a relation between SCH and diabetic neuropathy.
Recommendation
Routine screening of thyroid function in type 2 diabetic patients is necessary; and the treatment of subclinical hypothyroidism might have a considerable effect on the prevention or clinical course of vascular complications in type 2 diabetes.
Limitation of the study
Firstly, our study was observational, and it does not follow the effect of treatment of subclinical hypothyroidism on risk reduction of diabetic vascular complication. Secondly, there is a need for further study with a case matched control to be compared to the major variables like age, duration of DM, glycemic control, and lipid profile. Thirdly, the screening tests for diabetic nephropathy were done once; ideally these should be repeated for confirmation. Finally, we did not evaluate the other macrovascular complications of diabetes such as cerebrovascular and peripheral vascular diseases.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 31 December 2016
References
- M.HelfandC.C.RedfernClinical guideline, part 2. Screening for thyroid disease: an update. American College of PhysiciansAnn Intern Med1291998144158
- R.KadiyalaR.PeterO.E.OkosiemeThyroid dysfunction in patients with diabetes: clinical implications and screening strategiesInt J Clin Pract64201011301139
- A.E.HakH.A.PolsT.J.VisserH.A.DrexhageA.HofmanJ.C.WittemanSubclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam StudyAnn Intern Med1322000270278
- A.R.CappolaL.P.FriedA.M.ArnoldM.D.DaneseThyroid status, cardiovascular risk, and mortality in older adultsJAMA295200610331041
- J.K.YangW.LiuJ.ShiY.B.LiAn association between subclinical hypothyroidism and sight-threatening diabetic retinopathy in type 2 diabetic patientsDiabetes Care33201010181020
- B.Y.KimC.H.KimC.H.JungJ.O.MokK.I.SuhS.K.KangAssociation between subclinical hypothyroidism and severe diabetic retinopathy in Korean patients with type 2 diabetesEndocr J58201110651070
- H.S.ChenT.E.WuT.S.JapR.A.LuSubclinical hypothyroidism is a risk factor for nephropathy and cardiovascular diseases in Type 2 diabetic patientsDiabetic Med: J Br Diabetic Assoc24200713361344
- C.P.WilkinsonF.L.Ferris3rdR.E.KleinP.P.LeeProposed international clinical diabetic retinopathy and diabetic macular edema disease severity scalesOphthalmology110200316771682
- J.ChenDiabetic nephropathy: scope of the problemE.V.LermaV.BatumanDiabetes and kidney diseasevol. 20142014914
- Summary of Revisions for the 2013 Clinical Practice Recommendations Diabetes Care 2013 Jan; 36 (Suppl 1): S3–S3. http://https://doi.org/10.2337/dc13-S003.
- S.La VigneraR.CondorelliE.VicariA.E.CalogeroEndothelial dysfunction and subclinical hypothyroidism: a brief reviewJ Endocrinol Invest35201296103
- B.BiondiM.GalderisiL.PaganoM.SidiropulosEndothelial-mediated coronary flow reserve in patients with mild thyroid hormone deficiencyEur J Endocrinol/Eur Fed Endocr Soc1612009323329
- FengGaoN.P.PoulléMohammad IshraqZafarRajaAdeel ShafqatAssociation among subclinical hypothyroidism, TSH levels and microvascular complications in Type 2 diabetic patientsIOSR J Dent Med Sci (IOSR-JDMS)1320140106 e-ISSN: 2279-0853, p-ISSN: 2279-0861. Ver VI (Mar 2014)
- J.G.HollowellN.W.StaehlingW.D.FlandersW.H.HannonSerum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III)J Clin Endocrinol Metab872002489499
- P.PerrosR.J.McCrimmonG.ShawB.M.FrierFrequency of thyroid dysfunction in diabetic patients: value of annual screeningDiabetic Med: J Br Diabetic Assoc121995622627
- H.BilginO.PirgonThyroid function in obese children with non-alcoholic fatty liver diseaseJ Clin Res Pediat Endocrinol62014152157
- FengGaoN.P.PoulléMohammad IshraqZafarRajaAdeel ShafqatAssociation among subclinical hypothyroidism, TSH levels and microvascular complications in Type 2 diabetic patientsIOSR J Dent Med Sci (IOSR-JDMS)1320140106 Ver. VI. (Mar.)
- A.I.KatzD.S.EmmanouelM.D.LindheimerThyroid hormone and the kidneyNephron151975223249
- E.AlgunC.TopalM.OzturkM.R.SekerogluA.DurmusUrinary beta-2 microglobulin in renal dysfunction associated with hypothyroidismInt J Clin Pract582004240243
- M.A.SingerOf mice and men and elephants: metabolic rate sets glomerular filtration rateAm J Kidney Dis: Off J Natl Kidney Found372001164178
- M.SuherE.KocN.AtaC.EnsariRelation of thyroid disfunction, thyroid autoantibodies, and renal functionRen Fail272005739742
- T.YasudaH.KanetoA.KurodaT.YamamotoSubclinical hypothyroidism is independently associated with albuminuria in people with type 2 diabetesDiabetes Res Clin Pract942011e75e77
- F.JiaJ.TianF.DengG.YangSubclinical hypothyroidism and the associations with macrovascular complications and chronic kidney disease in patients with Type 2 diabetesDiabetic Med201510.1111/dme.12724
- A.R.CappolaP.W.LadensonHypothyroidism and atherosclerosisJ Clin Endocrinol Metab88200324382444
- P.J.OwenR.SabitJ.H.LazarusThyroid disease and vascular functionThyroid: Off J Am Thyroid Assoc172007519524
- S.TaddeiN.CaraccioA.VirdisA.DardanoImpaired endothelium-dependent vasodilatation in subclinical hypothyroidism: beneficial effect of levothyroxine therapyJ Clin Endocrinol Metab88200337313737
- S.RazviL.IngoeG.KeekaC.OatesC.McMillanJ.U.WeaverThe beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trialJ Clin Endocrinol Metab92200717151723
- A.D.HingoraniJ.CrossR.K.KharbandaM.J.MullenAcute systemic inflammation impairs endothelium-dependent dilatation in humansCirculation1022000994999
- E.E.TuremenB.CetinarslanT.SahinZ.CanturkI.TarkunEndothelial dysfunction and low grade chronic inflammation in subclinical hypothyroidism due to autoimmune thyroiditisEndocr J582011349354
- J.G.den HollanderR.W.WulkanM.J.MantelA.BerghoutCorrelation between severity of thyroid dysfunction and renal functionClin Endocrinol622005423427
- M.I.SurksE.OrtizG.H.DanielsC.T.SawinSubclinical thyroid disease: scientific review and guidelines for diagnosis and managementJAMA2912004228238
- H.GharibR.M.TuttleH.J.BaskinL.H.FishP.A.SingerM.T.McDermottSubclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine SocietyJ Clin Endocrinol Metab902005581585 discussion 6–7
- J.W.ChuL.M.CrapoThe treatment of subclinical hypothyroidism is seldom necessaryJ Clin Endocrinol Metab86200145914599
- J.W.ChuL.M.CrapoShould mild subclinical hypothyroidism be treated?Am J Med1122002422423
