Abstract
We report a case of Broken Heart Syndrome in a 56 year old Postmenopausal woman suffered while undergoing simple biopsy procedure for vocal cord polyp that lead to physical, mental and financial burden both for the patient as well as the doctors. A team of cardiologists based on clinical and echocardiographic findings made the diagnosis of this case.
1 Introduction
Broken Heart Syndrome also known as the Transient Left Ventricular Apical Ballooning Syndrome (TLVAB), Tako-Tsubo Cardiomyopathy, Stress CardiomyopathyCitation1 is an acute reversible left ventricular dysfunction in the absence of obstructive atherosclerotic coronary artery disease due to emotional or physical stressCitation2 usually affecting elderly post menopausal women.Citation3 It mimics acute myocardial Infarction and acute coronary syndrome with characteristics features of typical chest pain, pulmonary edema, diaphoresis, cardiogenic shock along with ST elevation in electrocardiogram and raised cardiac enzymes.Citation4 The pathophysiology of this syndrome involves coronary vascular dysfunction due to excessive sympathetic stimulation. This syndrome is characterized by a sudden onset of transient akinesia/hypokinesia of the left ventricle often involving all three major coronary artery territories in the absence of significant coronary artery stenosis.Citation4 This syndrome is widely misdiagnosed as acute myocardial infarction by physicians that lead to unnecessary interventions.Citation5 As this syndrome is an Intra-operative complicationCitation5 due to stress, it has become a miserable experience for the anaesthetists, just as in our case. Beta-blockersCitation5 and intensive care is the prime mode of treatment, which provides good recovery and relatively rare deaths.
2 Case presentation
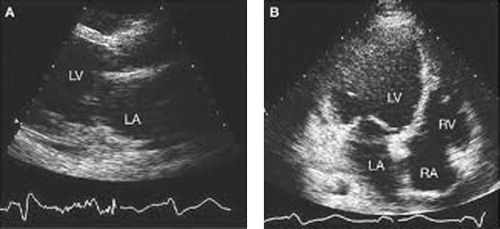
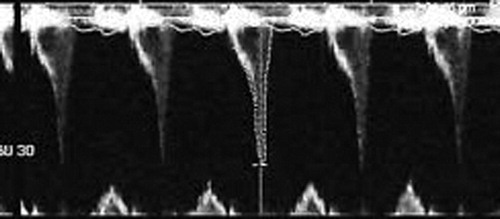
A 56-year old post-menopausal woman was presented to Otorhinolaryngology outdoor in National Institute of Medical Science, Jaipur with complaints of hoarseness of voice since 3 months. On laryngoscopic examination she was diagnosed with vocal cord polyp for which biopsy was planned to rule out malignancy. She was posted for biopsy in O.T. (Operation Theatre) next day. During elective intubation, patient suddenly became hemodynamically unstable and suffered Cardio-Pulmonary arrest for which she was resuscitated, revived and shifted to medical ICU (Intensive Care Unit) for further management. Patient was brought to us in cardiogenic shock (HR – 140/min, BP – 100/40 mm of Hg), frank ST elevation in anterior chest leads, raised cardiac enzymes (Troponin-T, CPK-MB, SGPT). 2D-Echo (Two dimensional echocardiography) findings reveal – akinetic LAD (Left Anterior Descending) territory with EF-35%, Central venous pressure was 19 mmHg and arterial blood gas analysis revealed metabolic acidosis (pH – 7.23, HCO3− – 12 meq/L). On auscultation bilateral coarse crepitation’s heard with normal heart sounds. However patient remained conscious co-operative with preserved urine output.
Her treatment was started with dopamine and dobutamine support to increase the cardiac output, guarded intravenous fluids with diuretics with strict monitoring of central venous pressure (CVP) maintaining it between 8 and 12 mmHg, routine arterial blood gas analysis and serum electrolytes in addition to cardio-protective dual anti-platelet drugs like aspirin and clopidogrel, statin, Low molecular weight Heparin along with broad spectrum antibiotic. Later patient was taken on Intra Aortic Balloon Pump support. After continuous monitoring for 48 h, patient showed improvement as her chest became clear and ionotropic supports came down and beta-blockers were added to treatment regimen. On 3rd day, her 2D-Echo was repeated which raised our eyebrows, as cardiac activity was absolutely normal (No regional wall motion abnormalities-RWMA, Ejection Fraction – 55%). She was shifted to catheterization laboratory for coronary arteriography, which further added to our surprise list as normal coronaries. Patient showed drastic improvement and was discharged on simple beta-blockers on day-7. The team of Cardiologists diagnosed this as ‘Broken Heart Syndrome’.
3 Discussion
Broken Heart Syndrome/Stress induced Cardiomyopathy is an acute reversible condition first recognized in 1990s. 90% of the patients were women preferably post-menopausal between ages of 66 and 80 years.Citation6 The mechanism of myocardial dysfunction in stress induced cardiomyopathy has not been fully elucidated, but a leading hypothesis suggests that a catecholamine surge resulting in regional microvascular dysfunction in susceptible patients, accompanied by cellular calcium overload.Citation7 The most common area involved is left ventricle (LV) apex (hence the synonym apical ballooning syndrome), however RWMA (Regional Wall Motion Abnormality) is also seen in mid ventricular/other ventricular walls with compensatory hyperdynamic contraction of the basal LV segments with associated apical LV dyskinesia results in acute left ventricular outflow tract obstruction as in this case because of systolic anterior motion of the mitral valve with associated outflow tract gradient and hypotension.
The long term prognosis is good with mortality around 1–2% due to rare complications such as irreversible cardiogenic shock, LV rupture or embolization of LV thrombi, fatal arrhythmias and complete heart block.Citation8 The association of this disease with QT interval prolongation in electrocardiogram has been noted hence drugs prolonging QT should be avoided along with strict monitoring of electrolyte levels. Recurrence is seen in 2–5% cases.Citation9 Long term management with Beta-blockers is advised as treatment strategy to suppress cathecolamine surge and there is no need of anti-platelets and anti-coagulants (see and ).
4 Conclusion
Although rare, it is serious intra-operative complication which may lead to death if not managed properly. Hence operating surgeon, anaesthetist and attending physician/cardiologist should always keep this in mind while managing sudden cardiac dysfunction as an intraoperative complication. This is a disorder with very good prognosis with proper treatment guidelines as well as fatal prognosis with misdiagnosis/under diagnosis.
Acknowledgement
Thanks to Department of Medicine, Department of Cardiology, nursing Staff for their extra-ordinary care shown towards this patient.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 9 March 2017
References
- P.R.HansenStress induced “Tako-Tsubo” cardiomyopathy: you can die from a broken heart!Ugeskr Laeger169200712091211
- I.S.WittsteinAcute stress cardiomyopathyCurr Heart Fail Rep220086168
- P.Hedberg“Broken heart” or Takotsubo cardiomyopathy mostly in postmenopausal women. Stress induced condition resembling acute myocardial infarctionLakartidningen104200732773282
- S.MiddlemostTakotsubo cardiomyopathy: acute and reversible cardiomyopathy mimicking acute myocardial infarctionCardiovasc J Afr1920083338
- S.LiuPerioperative transient left ventricular apical ballooning syndrome: Takotsubo cardiomyopathy: a reviewJ Clin Anesth2220106470
- A.DeshmukhG.KumarS.PantPrevalence of Takotsubo cardiomyopathy in United StatesAm Heart J164201266
- I.S.WittsteinStress cardiomyopathy: a syndrome of catecholamine mediated myocardial stunning?Cell Mol Neurobiol322012847
- F.F.SyedS.J.AsirvathamJ.FrancisArrythmia occurence with Takotsubo cardiomyopathy: a literature reviewEuropace132011780788
- G.ParodiB.BellandiS.Del PaceNatural history of Takotsubo cardiomyopathyChest1392011887892