Abstract
Aim of work
The aim of the study was to assess the diagnostic performance of static MR urography in detection of post cystectomy complications & the ability of static fluid MR urography in visualization of urinary tract segments.
Material & methods
We prospectively reviewed 21 MR urograms with urinary diversion. The most common surgical procedures included Ileal conduit & Ileocecal neobladder diversion.
Magnetic resonance urography examinations were performed with 1.5-T MR scanners. T2 weighted (static fluid) MR urography techniques were done, in addition to conventional T1- and T2-weighted axial and coronal sequences. Urinary tract was divided in different parts: pelvicalyceal systems, upper, mid and lower ureteric segments & the reservoir or conduit Imaging features of the urinary collecting systems were evaluated for their visualization and complications detection.
Results
T2-weighted MR urography could demonstrate 95% of urinary tract segments & together with conventional MR sequences all urinary tract segments can be visualized. Urinary diversion related complications were encountered included in 15 patients (71.4%) & no urological complications were seen in 6 patients (28.6%).
Conclusion
Comprehensive T2-weighted MR urography is an effective imaging method for the visualization of the urinary system and detection of early and late postoperative complications in patients with urinary diversion.
1 Introduction
Bladder cancer represents 2–4% of all malignancies. It is a disease of elderly with a peak incidence during the seventh decade. Bladder cancer is three times more common in men than women.Citation1
Bladder cancer are divided into superficial & muscle invasive bladder cancer. Surgery plays major role in management of invasive urinary bladder cancer. Radical cystectomy is the standard operation for treatment of muscle invasive cancer bladder (stage T2 or higher) & superficial bladder carcinoma resistant to local treatment.Citation2
The expectations of post radical cystectomy has evolved from simple diversion to body preserving continent urinary diversion.Citation3
Radical cystectomy is a major operation. Various early and late complications may be seen following urinary diversion procedures.Citation4
Strict post-operative radiologic follow up starting at early postoperative period to assess integrity of diversion & detection of possible early complications. Later follow ups are needed to assess the capacity of the reservoirs, evaluation of upper urinary tract changes & detection of potential late complications of the procedure.Citation1
No post urinary diversion follow-up imaging protocols have been established. Different imaging modalities have been described as excretory urography, fluoroscopy-guided retrograde contrast studies, Ultrasonography & Computerized tomography urography.Citation5
MR urography is an evolving and promising technique in the evaluation of the urinary tract. MR urography is currently considered the method of choice for imaging of the renal parenchyma and the collecting systems in patients who cannot undergo routine radiographic studies such as patients with impaired renal function.Citation6
An MRI examination of the urinary collecting system is performed by two main methods: static-fluid urography with T2-weighted sequences, as used for MRCP, and excretory urography with T1-weighted sequences after IV contrast administration.Citation7
T2-weighted MR urography technique can visualize static fluids. It does not depend on renal function & does not require intravenous (I.V.) contrast so it can be used to evaluate urinary systems in poorly functioning kidneys.Citation5
Static MR urograms are obtained heavy T2-weighted sequences that exploit the long T2 relaxation time of urine. Sequences used closely resemble those used for T2-weighted MR cholangiopancreatography (MRCP). Heavily T2-weighted static-fluid MR urograms provide similar images to those obtained from conventional excretory urograms giving an overview of the urinary tract & quickly identifying the level of urinary tract obstruction.
Further conventional MRI sequences are needed to characterize the cause of obstruction.Citation8
The aim of the study was to assess the diagnostic performance of static MR urography in detection of post cystectomy complications & the ability of static fluid MR urography in visualization of urinary tract segments ().
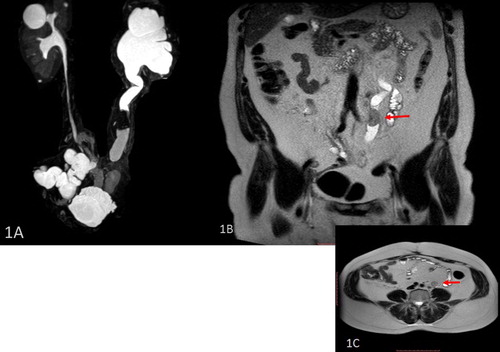
Fig. 1 A 54 years old male with urinary bladder cancer (Invasive TCC, grade III), underwent radical cystectomy and urinary diversion (ileal conduit). Follow up MRU 2 years postoperative was done. (1A) Coronal maximum intensity-projection MR urography images obtained from three-dimensional (3D) T2 turbo spin echo, (1B) coronal T2 WI & (1C) axial T2 WI sequences show a left intra-ureteric defect elicited in conventional MR sequences as soft tissue lesion (arrows) likely meta-synchronous Lesion (proved pathologically to be TCC grade III) with subsequent hydroureter & hydronephrosis .A pelvic cystic fluid collection is also noted.
2 Materials and methods
Institutional review board approval was obtained for this prospective study. The requirement for informed consent was waived.
21 patients underwent radical cystectomy & urinary diversions were examined using a 1.5 MR scanner (Acheiva, Philips Medical Systems, Netherlands) by using phased-array body coils. Our source was the surgical oncology department which referred urinary diversion patients presenting with a clinical complaint (e.g. decreased urine output).
The study was conducted at a specialized oncology Institute in the period from February 2013 to April 2014.
The patient's age ranged from 34 to 79 years old.
Estimated glomerular filtration rate (eGFR) values of all patients were calculated before the MR urography study using the Modification of Diet in Renal Disease Study Group equation in case of contrast injection was needed.
Demographics of the patients are illustrated in .
Table 1 Demographic, primary pathology, type of urinary diversion, laboratory features and MRI findings of the patients.
MRI examinations started with localizing sequences & continued with T2-weighted MR urograms obtained by single thick slab or maximum-intensity-projection (MIP) views generated from multiple thin slice three dimensional (3D) T2-weighted images. Conventional MRI sequences including axial and coronal T1 & T2-weighted were done if an abnormality was seen.
Single-shot fast spin-echo images were obtained each in 10 s, which allows multiple images of the urinary tract in different projections to be obtained sequentially in a relatively short period of time. Projections were obtained in coronal plane & each side of the urinary tract in sagittal plane.
3D high resolution T2 sequence is obtained via acquisition of multiple overlapping slices with slice thickness 1 mm & 0 gap then images are processed using Maximum intensity projection (MIP) parallel to vertical axis of the urinary tract with 10–20 degree angulation.
MR urography sequences allowed localization of the level and degree of obstruction ().
Table 2 MR urography sequences used in Philips Acheiva MR scanner.
For characterization of the presumed pathology conventional MR sequences were used axial T1 & T2 WIs as well as coronal T1 & T2 WIs.
The whole examination took about 12–13 min which could be modified to less time according to each patient.
The MR urography images were evaluated alone & in conjunction with conventional MR sequences for the ability of visualization of the different segments of the urinary tract.
We used a segmentation model similar to the one used by Battal et al. for the evaluation of the urinary diversions. The urinary collecting system was divided into 10 segments: right and left collecting systems, proximal, mid &distal thirds of both ureters as well as urinary conduit or reservoir which was considered as 2 segments in our study. So a full urinary diversion urinary tract will have a score of 10.
For detection of complications each case was evaluated independently by two radiologists, and a final diagnosis was reached by consensus. We searched for postoperative complications including leakage, fluid collections (as urinoma, abscess, lymphocele) fistula, ureteral stricture, Backpressure changes, listhiasis & tumor recurrence.
3 Results
We found that 85.7% of patients underwent urinary diversion were males (18 patients) and 14.3% were females (3 patients).
The most common indication of urinary diversion is cancer bladder encountering 95% of cases. The main cancer bladder pathological subtypes were Transitional cell carcinoma (TCC) and squamous cell carcinoma (SCC).
The most common types of urinary diversions were orthotopic ileocecal neobladder replacement & ileal conduit procedures ().
MRU was performed in different postoperative periods from 3 weeks to 10 years postoperative.
Patients’ blood creatinine values ranged from 0.7 to 3.7 mg/dL and eGFR values ranged from 28 to 128 mL/min/1.73 m2. Patients eGFR values <30 mL/min/1.73 m2 were 30%, patients eGFR values between 30 & 60 mL/min/1.73 m2 were 33% of patients, patients eGFR values between >60 mL/min/1.73 m2 were 38% of patients.
According to the segmentation model 202 urinary segments were evaluated using the static fluid MR urography (180 segments for 18 patients with a complete urinary diversions having 10 segments each & 8 segments for 2 patient had ureteronephrocystectomies & one side uretero-cutaneous diversion having 4 segments each as well as 14 segments for 1 patient with left ureteric complete duplication).
192 segments were visualized via MRU sequences alone (95%).The non-visualized segments were distal ureteral segments at the site of insertion into the conduit or neobladder or at cutaneous exit. In combination with conventional MR sequences 100% of the ureteric segments were visualized ().
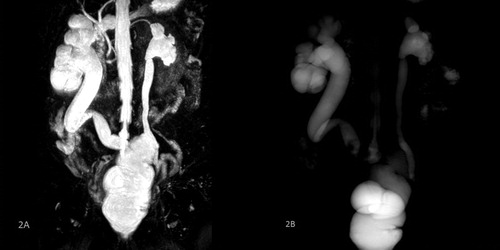
Fig. 2 A 61 years old male patient with urinary bladder cancer (Verrucoid SCC, grade I) underwent radical cystectomy, pelvic lymphadenectomy, rectal bladder & colostomy. MRU 1 year postoperative. (2A) Coronal maximum intensity-projection MR urography images obtained from three-dimensional (3D) T2 turbo spin echo & (2B) single shot MR urography image show right uretero-rectal bladder stricture with subsequent hydroureteronephrosis.
Urinary diversion related complications were encountered included in 15 patients (71.4%) & 6 patients (28.6%) had no urological complications. Urinary diversion related complications detected were fluid collections including urinary leakage and lymphoceles seen in 3 patients, tumoral recurrence in 4 patients with 2 of them showed local tumoral infiltration, 6 patients with ureteric strictures (2 unilateral & 2 bilateral), secondary fistula in 1 patient, urinary calculus in 1 patient & para-stomal hernia in 1 patient as well as chronic obstructive uropathy in 1 patient ().
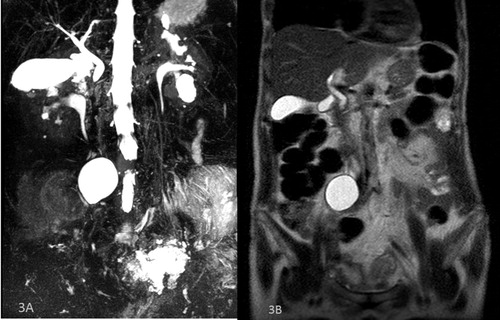
Fig. 3 A 59 years old male patient with cancer bladder (Infiltrating high grade TCC) underwent radical cystectomy, bilateral lymphadenectomy & ileal conduit. MRU is done 6 months postoperative. (3A) Coronal maximum intensity-projection MR urography images obtained from three-dimensional (3D) T2 turbo spin echo, & (3B) Coronal T2 WI show a cystic abdominal fluid collection (lymphocele).
Ureteric strictures were seen in 5 patients (3 patients had bilateral ureteric strictures,1 patient had unilateral ureteric stricture & 1 patient had 3 ureteric strictures in both ureters).
9 patients (16 side) had urinary back pressure changes 8 of these patients had an obstructing cause as stricture or tumoral recurrence) & 1 patient had bilateral back pressure changes with no obstructing cause ( and ).
Fig. 4 A 58 years old male patient with cancer bladder (TCC) (Urothelial with squamous differentiation) underwent radical cystectomy, left radical nephrectomy & ileocecal neobladder. MRU 5 years postoperative. (4A) Coronal maximum intensity-projection MR urography images obtained from three-dimensional (3D) T2 turbo spin echo, & (4B) Coronal T2 WI show neobladder mass lesion (recurrence), right upper ureteric stenotic segment and ureteroneobladder stricture.
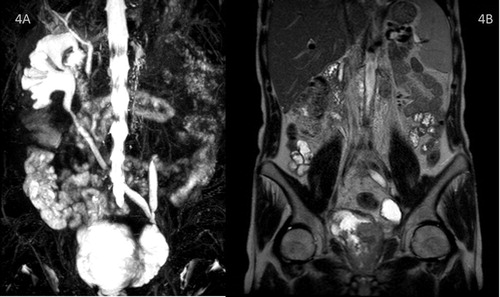
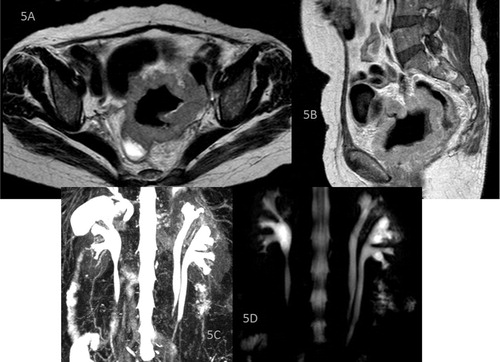
Fig. 5 A 64 years old female with urinary bladder cancer (SCC grade II) underwent anterior pelvic exentration & urinary diversion (Ileal conduit) MRU 1 year postoperative. (5A) Axial T2 WI, (5B) sagittal T1 WI, (5C) Coronal maximum intensity-projection MR urography images obtained from three-dimensional (3D) T2 turbo spin echo & (5D) single shot MR urography image show recurrent pelvic mass with rectal invasion and rectal fistula. Left ureteric complete duplication is noted in the MRU sequences.
Non urologic findings as ascites, pleural effusion and hepatic metastases were seen in 4 patients.
4 Discussion
The main indication for radical cystectomy is a muscle-invasive (stage T2 or higher) bladder tumor or high-risk high-grade noninvasive muscle disease.Citation4
Postoperative surgical complications are divided into early & late complications.Citation9,Citation10
Because of these potential complications, patients with urinary diversion require a proper radiological assessment starting from preoperative period continuing to postoperative period.Citation1
Main radiological investigations previously used were excretory urography and fluoroscopy-guided retrograde contrast studies.
Later with the evolution of multi-detector Computed tomography devices CT urography & CT conduitogram became new the techniques for identifying both normal postoperative findings and complications after urinary diversion.Citation5
However, the drawback of conventional fluoroscopic studies, CT urography & excretory MR urography are the inability to use contrast agents in patients with compromised renal function and in case of ureteral obstruction in which contrast excretion may be too low to allow visualization of the collecting system. Another drawback is increased radiation exposure in multiphasic studies.
As urinary diversion patients are more exposed to being with impaired renal functions, ureteral obstruction & need frequent follow ups, Static fluid MR urography plays an important role.
Initial MR urography sequences allowed localization of the level and degree of obstruction.
Single thick slab allowed quick identification of the level of urinary tract obstruction.
3D high resolution T2 sequence consumed a longer duration but provided a more detailed visualization of the urinary tract column of fluid.
The obstruction & the back pressure changes (hydroureteronephrosis) are indirect signs for the pathology.
T2 MR urography techniques alone will not be able to characterize the presumed pathology.
For characterization of the presumed pathology conventional MR sequences including axial T1 & T2 WIs as well as coronal T1 & T2 WIs in addition to contrast injection in selected cases.
In conventional MR sequences we recommend a maximum field of view to cover the whole urinary tract in addition to surrounding tissues as well as abdominal & pelvic viscera to characterize the urological & non urological postoperative complications & to visualize urinary tract segments missed on T2 MR urographic techniques.
The urinary systems segments of all patients could be properly assessed by comprehensive MRI examination combining T2-weighted MR urography technique to conventional MR sequences.
Urinary diversion related complications were encountered included in 15 patients (71.4%) & 6 patients (28.6%) had no urological complications. The relatively high rate of complications is due to refereed patients are symptomatic patients or patients with lost follow up over several years.
Complications encountered included ureteral strictures, being the most common complication occurring in 9 strictures on 8 sides of 5 patients. The stricture sites usually occur at the uretero-enteric anastomotic site, regardless of the type of ureteral re-implantation procedure.
We detected fluid collections in 3 of cases with complications .Fluid collections were mainly lymphoceles which were seen in patients who have undergone lymphadenectomy in conjunction with radical cystectomy for the treatment of a malignant bladder condition. The MR finding of a homogeneous fluid collection with a very thin wall, in a location near the surgical clips, were suggestive of the diagnosis of lymphocele.
We found also, local tumor recurrence may manifest with various patterns: It may appear as a pelvic soft-tissue mass or an obstructing ureteral stricture (commonly in association with a soft-tissue mass) or urethral stump recurrence.
Non urinary diversion related findings as hepato-splenomegaly, splenomegaly, ascites, pleural effusion, parastomal colostomy hernia and hepatic metastases were also seen.
A secondary fistula was seen in 1 patient where fistulous track occurred from recurrent pelvic mass invasion of rectum.
Advantages of MR urography include the lack of ionizing radiation & the lack of use of contrast agents also T2-weighted MR urography sequences alone can be obtained in a very short time and have high ability in visualizing urinary tract in patients with urinary diversion.
Our study has some limitations. Firstly, the number of patients in this study was limited. However, all types of diversion procedures were included. Secondly, no comparison to other imaging modality.
5 Conclusion
Radical cystectomy is a major surgical procedure with high risk of development of complications requiring proper preoperative preparation; follow up at both the early and late post-operative period.
Formal guidelines for follow-up after urinary diversion has not yet been established so what we suggest is a follow-up strategy addressing early and late postoperative complications.
An initial radiological assessment in the first three months is advised followed by a constant interval (six months) radiological follow ups.
The choice of the proper imaging modality used varies for each patient depends on inputs from clinical, laboratory & operative data as well as different specifications of each imaging modality.
Static fluid MR Urography is an effective alternative to excretory contrast studies in urinary diversion patients avoiding the use of ionizing radiation or use of contrast agents as they need frequent follow ups & usually have poor renal function.
Conflicts of interest statement
No conflicts of interests for any of the authors.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 16 June 2017
References
- S.MorcosH.ThomsenUrogenital imaging: a problem-oriented approach2009John Wiley & Sons
- P.BassiF.PaganoSurgical management. Invasive bladder cancer2007Springer107118
- J.B.DowdMethods of urinary diversionAORN J2319763744
- V.CataláM.SolàJ.SamaniegoCT findings in urinary diversion after radical cystectomy: postsurgical anatomy and complications 1Radiographics292009461476
- B.BattalM.KocaogluV.AkgunE.AydurM.DayancT.IlicaFeasibility of MR urography in patients with urinary diversionJ Med Imag Radiat Oncol552011542
- M.MemarsadeghiM.RiccabonaG.Heinz-PeerMR urography: principles, examination techniques, indicationsDer Radiologe452005915923
- O.J.O'ConnorP.McLaughlinM.M.MaherMR urographyAm J Roentgenol19532010W201W206
- J.R.LeyendeckerC.E.BarnesR.J.ZagoriaMR urography: techniques and clinical applications 1Radiographics2820082346
- R.E.HautmannH.Abol-EneinK.HafezUrinary diversionUrology6920071749
- E.W.GerharzA.RoosenW.MånssonComplications and quality of life following urinary diversion after cystectomyEAU Update Series32005156168
