Abstract
Introduction
Bone marrow aspiration (BMA) and bone marrow biopsy (BMB) is an indispensable diagnostic tool for evaluating haematological and non-haematological disorders and patient follow-up in present era. We have compared the advantages of trephine biopsy over bone marrow aspiration in these patients.
Aim and objective
To evaluate sensitivity and specificity of trephine biopsy test for haematological and non haematological disorder patients in comparison to bone marrow aspiration test.
Materials and method
In this 1 year prospective study (June 2014–May 2015), we evaluated the haematological and non-haematological disorder patients by BMA and BMB (aided with I.H.C. when ever needed). The sensitivity and specificity of the tests were calculated.
Results
Among, final 504 hemotological/non haematological disorder patients, 416 cases were diagnosed (+ve) in BMA test, where as it was 494 in BMB test and with chi2 test it was highly significant as p = 0.0001. It was concluded that True positive cases were 416, True negative were 9 cases, false negative 78 cases and false positive was in one case only. The sensitivity and specificity of bone marrow trephine biopsy test was 84% and 90% respectively.
Conclusion
BMB (aided with I.H.C) is a gold standard test for detecting different haematological and non hamatological disorders. In our study the sensitivity and specificity of BMB test was 84% and 90% respectively. When performed in association with BMA in the same sitting, significantly augments the chances of reaching a correct diagnosis.
1 Introduction
Bone marrow examination includes pathological examination of bone marrow aspiration (BMA) and bone marrow biopsy (BMB) specimens. Peripheral blood gives much of information regarding haematological disorders but many a times, “the assessment of haematopoesis with BMA and BMB” are highly required. BMA and BMB are an invaluable diagnostic tool for both haematological and non-haematological disorders. It is also routinely used for follow up of patients undergoing chemotherapy for hematolymphoid malignancies.Citation1 Marrow samples can be obtained from various sites. BMA and trephine BMB are commonly done from posterior superior iliac spine and iliac crest. BMA can be done from sternum with patient lying on his back, and pillow under the shoulder. Ideally it should not be done from sternum, because of risk of damaging vital organs. BMA can also be done from tibia in children up to 2 years of age.
BMA is the best tool for studying morphology, differential count and M:E ratio. It can be used for flowcytometry, cytogenetics as well as procedures like Polymerase chain reaction. whereas trephine BMB gives information regarding cellularity, architecture and focal lesions. Moreover, trephine biopsy is mandatory for staging of lymphomas.Citation2 Rarely marrow examination provides the only clue regarding occult malignancies.Citation3
BMB is not only the ‘clue’ for infiltration, but also provides pattern of involvement.Citation4 In earlier days surgical trephine biopsy was in practice. With introduction of needle trephine biopsy in late 1950s, things have become much simpler and minimally invasive.Citation4 However, trephine biopsy, unlike aspiration, demands more technical skills and is time consuming as well as a painful procedure. Interpretation depends on numerous factors like quality of tissue section and availability of ancillary techniques like immunohistochemistry, special staining and good coordination between hematopathologists and histopathologists.Citation5 Bone marrow procedures help in confirming the clinical diagnosis as well as some new diagnosis, which were not suspected previously. Few studies have analyzed the diagnostic accuracy of marrow aspirates with trephine biopsies.Citation1, Citation6–Citation8 Here, we compare these two tests i.e. BMB and BMA, to evaluate the sensitivity and specificity of BMB in haematological and non-haematological patients in the same sitting.
2 Material and methods
This single centre prospective study was carried out, by the Department of Pathology (Lab Hematology), Department of Hemato-oncology and Stem cell transplantation, Medicine and Paediatrics in IMS & SUM Hospital from June 2014 to May 2015. This study was done for bone marrow examination on patients presenting with anemia, history of thrombocytopenia, leukopenia, pancytopenia, marked leucocytosis, bleeding/disseminated intravascular coagulation, fever and organomegaly. Both indoor and outdoor patients, showing features, raising suspicion of involvement of bone marrow by non haematological/haematological disorders were included. Relevant history, informed consent and other bio-datas were noted. Patients were investigated for routine complete blood count (CBC), peripheral blood smear comment (PSC), reticulocyte count, coagulation profile (prothrombin time, activated partial thromboplastin time, thrombin time, fibrinogen). Then BMA and trephine BMB were done for these patients at the same sitting. A total of 595 (570 + 25) cases of BMA along with trephine BMB were carried out. Out of which 25 tests were inadequate for assessment, hence excluded from the study. Adequacy of biopsy was based on the presence of at least 5–6 intertrabecular spaces. So the cohort comprised of 570 cases. Among them 66 cases were post induction marrows for assessment of remission. So, these 66 cases were excluded from this study. Finally, for comparison of trephine BMB with BMA tests a total of 504 cases were studied.
The clinical indications, physical findings and peripheral smear findings of patients were compiled. Under local anesthesia (2% xylocaine, 2% lignocaine) infiltration of periosteal region, the BMA and BMB were done from posterior superior iliac spine, by using jamshidi needle. Patient is made to lie on their side (lateral decubitus position). A Bone marrow aspiration needle was inserted through the skin with pressure until it abuts the bone. The needle was advanced through the bony cortex and in the marrow cavity with twisting motion of the hand and wrist of the clinician. After the needle tip reaches the marrow cavity, a syringe was attached to the back of the jamshidi needle and aspiration done. A twisting motion is performed during the aspiration to avoid excess content of blood in the sample. For BMA procedure, Jamshidi needle (13 G for children, 11 G for adults) and Illinois needle size 18 were used. Subsequently 0.25–0.5 ml aspirate was withdrawn using a 2 ml plastic syringe and smears were prepared immediately. Trephine BMB was done using Jamshidi biopsy needle and at the same incision but approximately 0.5–1.0 cm away from aspiration site to avoid getting a haemorrhagic biopsy. In patients of thrombocytopenia, 5 minof firm pressure was applied at the end of the procedure. At the same time patients were asked to lie down on their back for further 10–15 min for prolonged pressure. Aspiration smears were stained with Giemsa stain after being fixed in alcohol. Prussion blue stain for iron store assessment and grading was done routinely. Biopsy specimen was fixed using 10% buffered formalin and decalcified using 10% formic acid for 24 h and processed by preparing paraffin wax embedding sections. Histological sections were made approximately 1–2 µm thick. Haematoxylin and eosin (H&E) stain was used and reticulin fibres were stained with Gomori’s silver impregnation method routinely. Immuno histo chemistry (IHC) was done as and when required.
3 Results
Both BMA and trephine BMB tests were performed on all 504 cases of haematological and non-haematological patients. In BMA, 416 cases were diagnosed (positive) whereas in trephine BMB, it was 494 cases (). The chi-square statistic is 68.7673 and p-value is 0.0001. This result is significant at p ≤ 0.05.
Table 1 Cases diagnosed in BMA and BMB.
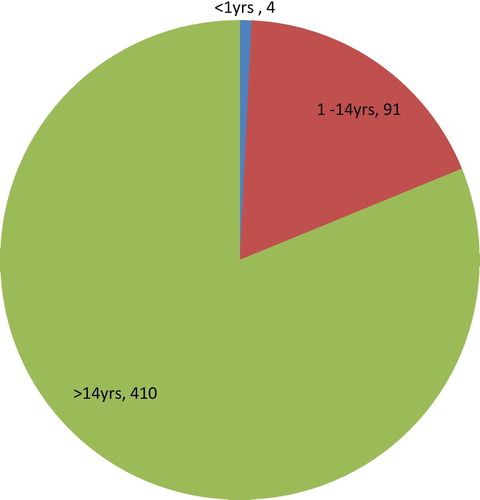
The 504 new cases were divided into 3 age group categories. 4 cases were below 1 yrs of age, 91 cases belonged to 1–14 yrs age group and 410 cases were above 14 yrs of age (). The cases were divided into groups according to the final diagnosis, after assessing the peripheral smears, bone marrow aspiration and trephine biopsy.
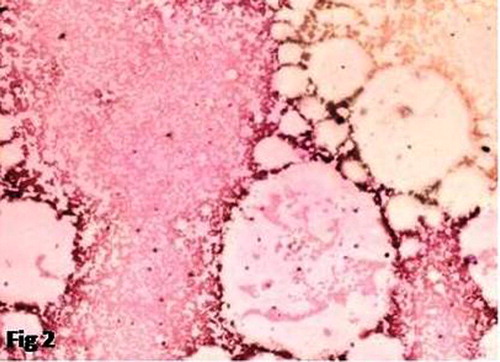
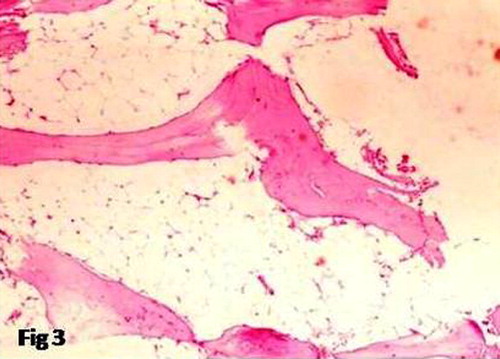
Acute leukemia was the largest group comprising of 128 cases. Bone marrow aspiration was in agreement with trephine biopsy in 110 cases but was inadequate in 18 cases which had tightly packed marrow with blasts on biopsy. Aplastic anemia was the next single largest group with 45 cases. Biopsy in aplastic anemia is of utmost importance for definitive diagnosis. 6 cases showed diluted/non diagnostic aspirates which were diagnosed on only trephine biopsy ( and ). One case diagnosed in aspiration as hypoplastic marrow suggestive of aplastic anemia, showed focal increase in immature precursors and diagnosis was revised to hypoplastic myelodysplastic syndrome (MDS) in biopsy.
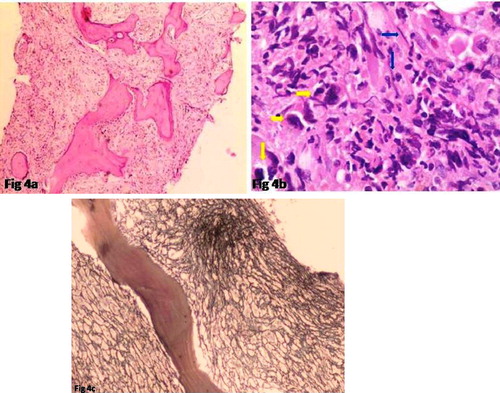
Out of 52 Myeloproliferative neoplasm cases of MPN, 42 cases were of CML, 2 cases of Essential thrombocythemia (ET), 1 case of Polycythemia vera (PV), 3 cases of Chronic Eosinophilic Leukemia/Hypereosinophilic syndrome (CEL/HES) and 4 cases were of Myelofibrosis. Poor aspiration material was found in 9 cases of CML. Fibrosis was increased in 7 cases. All 4 cases of Myelofibrosis showed dry tap, trephine showed marked fibrosis and atypical bizarre megakaryocytes (a–c).
Fig. 4 (a) BMB showing hypocellularity & Fibrosis, H&E (10 × 10), (b) 40 × 10, yellow arrow-bizarre megakaryocytes, blue arrow-fibrosis, (c) 10 × 10 increased reticulin fibrosis of myelofibrosis.
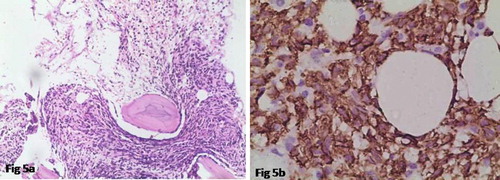
A total 41 cases of lymphoma were analyzed, of which 8 cases were Hodgkin’s lymphoma, and 33 cases were NHL. Out of 33 cases of NHL, few cases showed occasional atypical cell in marrow aspirate (but not diagnostic of marrow infiltration by lymphoma). In BMB, four cases of low grade B cell lymphoma (a and b), 1 case of Follicular lymphoma were detected. One case of Burkitt lymphoma diagnosed on IHC and unfortunately 02 cases could not be typed. None of the Hodgkins lymphoma showed marrow infiltration in aspiration. Among the total, Chronic lymphocytic leukemia (CLL/SLL) comprised of 16 cases. All cases of CCL/SLL were diagnosed in BMA. Among 42 cases of multiple myeloma (plasma cell dyscrasia) 41 cases were detected in BMA. One case of aspiration showed hypercellular marrow with poor cell trails showing occasional plasma cells and biopsy was diagnosed to be of multiple myeloma with marked plasmacytosis. Six cases of metastasis were encountered in biopsy out of which 2 (33.3%) were missed in aspiration.
Fig. 5 (a) 10 × 10 small cell lymphoma involving marrow, (b) 40 × 10 I.H.C.-lymphoma involving marrow, CD20 +ve.
Out of four cases, two cases showed granulomas in both aspiration and biopsy. Whereas two cases showed granulomas in biopsy only (missed in aspiration). Out of 25 cases of MDS, aspiration and biopsy correlated in 20 cases, in rest 5 cases, diagnosis was done in biopsy only. In Immune Thrombocytopenic purpura (ITP), there were 100% concordance between aspiration and biopsy. Out of 5 cases of Pure Red Cell Aplasia (PRCA), trephine biopsy of one case showed presence of paratrabecular collection of lymphoid cells pointing towards the possibility of lymphoma as a probable cause of PRCA (Secondary PRCA). However, the patient was lost to follow up. One non diagnostic/diluted aspiration with focal necrosis showed extensive necrosis in bone marrow trephine biopsy. The details are given in . From the above 2 tests i.e. BMA and BMB for detection of haematological and non-haematologic disorder, it was revealed that 416 cases were diagnosed/positive in both tests. Hence true positive cases were 416. In the same way, true negative, false negative and false positive cases were determined (). The sensitivity and specificity of the trephine BMB test were 84% and 90% respectively. The statistical probabilities were determined with SPSS 20 software and documented ( and ).
Table 2 Number of entities in bone marrow aspiration and bone marrow biopsy.
Table 3 Statistical probability of BMA and BMB tests.
Table 4 Computed probability value of different statistics tests.
4 Discussion
Bone marrow aspiration and biopsy at a single sitting are complementary to each other and therefore should be used together for diagnosis. Out of total aspirate smears, some cases were inadequate for evaluation. According to Bird and Jacobs,Citation8 marked increase in reticulin in both acute lymphoblastic and acute myeloblastic leukemia may lead to dry tap. In present study, 3 out of 18 cases of acute leukemia presenting with dry tap showed increase in fibrosis in trephine sections. So a dry tap or inadequate aspiration should not be dismissed as a result of faulty technique but should always be accompanied by trephine biopsy to arrive at a conclusive diagnosis.
In some cases of acute leukemia, adequate bone marrow aspirate cannot be obtained due to extreme cellularity and compactness of the marrow.Citation8 These are the cases where bone marrow trephine biopsy has primary diagnostic value. An important limitation of using marrow aspiration alone is mixing of marrow elements with sinusoidal blood which does not allow accurate estimation of cellularity.
In lymphomas, cytomorphology combined with immunophenotyping, were used for primary diagnostic approach. All cases of Non Hodgkin’s Lymphoma (NHL) showed evidence of marrow involvement in biopsy. In corresponding aspiration smears only some smears showed occasional atypical cell, non conclusive of lymphoma involving marrow. None of the Hodgkin’s lymphoma showed infiltration in aspiration. Various studies have reported marrow infiltration in lymphoma ranging from 27.1 to 55.1%.Citation9,Citation10 In our case all CLL/SLL cases (16) were diagnosed in aspiration and also in biopsy. In Aplastic anemia, diagnosis was confirmed only after trephine biopsy, where as some cases were missed in BMA. Trephine biopsy is the only tool for accurate assessment of cellularity of the marrow, hence is of utmost importance in diagnosing Aplastic anemia.Citation11 In CMPDs, other than Myelofibrosis, peripheral smears and aspirates were adequate for diagnosis but trephine biopsy added information about fibrosis, cellularity and morphology of megakaryocytes. Also it is of paramount importance to assess the residual disease. In some cases, the methods are complementary and thus both are needed, as described by Sabharwal et al.Citation12 In Multiple myeloma 41 out of 42 (97.6%) cases of were diagnosed in bone marrow aspirates alone. One case where the plasma cells were sparsely scattered in a diluted marrow showed compact masses of plasma cells in biopsy. Our study correlated well with the study done by Pileri et al.Citation13 where they detected myeloma simultaneously in all bone marrow aspirates and biopsies. As per FarhiCitation14 plasma cell myeloma, particularly in cases with low infiltration degree, were more reliably diagnosed in the biopsy. Granulomas showed higher detection rate in trephine biopsy than aspiration and correlated well with other studies. No benefits were obtained in cases of erythroid hyperplasia and reactive marrow. In a study, the BMA alone had a sensitivity of 86.8% in detecting residual leukemia and of 82.3%, 82.5% and 94.2% for interim, EOI and ‘other marrows’, respectively. Despite the high concordance between the BMA and the BMTB the poor sensitivity of the BMA in detecting residual leukemia, particularly at EOI, may lead to an overestimation of the complete remission rates which may have therapeutic and clinical trial implications.Citation15 From an Australian study, it was revealed that specificity was 100%; sensitivity 82–91%, positive predictive value 100% and negative predictive value 90–95%.Citation16 The quantitative assessment of neuroblastoma cells is recommended to provide data from which evidence-based numerical criteria for the reporting of bone marrow response can be realized. This is particularly important in the minimal disease setting and when neuroblastoma detection in bone marrow is intermittent, where clinical impact has yet to be validated.Citation17–Citation19 Acute leukemias are characterized by neoplastic proliferation of hematopoietic stem cells and accumulation of blasts and immature cells in bone marrow. We applied a selective panel of immunohistochemical markers on bone marrow trephine tissue sections and observed their utility in diagnosis and typing of acute leukemia.Citation19 A good bone marrow (BM) sample is essential in evaluating many haematologic disorders. An unsuccessful BM aspiration (BMA) procedure precludes a successful flow cytometric immunophenotyping (FCI) in most haematologic malignancies. Apart from FCI, most ancillary diagnostic techniques in haematology are less informative. We describe the feasibility of FCI in vortex-dislodged cell preparation obtained from unfixed trephine biopsy (TB) specimens. It reveals efficient procedure which could be effectively utilized in resource-limited centers and reduce the frequency of repeat BMA procedures.Citation20,Citation21 Most guidelines suggest that only the bone marrow aspirate (BMA) is necessary to assess residual disease following intensive chemotherapy for Acute Myeloid Leukemia (AML) with the bone marrow trephine biopsy (BMTB) recommended in cases of a poor quality BMA.Citation22
However there were some limitations in our study. We could not analyze the role played by flowcytometers and cytogenetics, routinely done in this era for all cases of Acute Leukemia and MDS. Also, lack of use of IHC routinely in cases of NHL due to financial constraints might have hampered the accuracy of detection of infiltration.
5 Conclusion
Bone marrow trephine biopsy is gold standard and more informative in assessment of cellularity, pattern, extent of tumor infiltration and follow up (especially) of leukemia/lymphomas. It is an indispensable tool for diagnosis of Aplastic Anemia. However, it provides less additive information in most Acute Leukemias and non neoplastic pathologies except for Granulomas. Since, both procedures can be done in the same sitting, obtaining adequate biopsy material along with aspirate sample is strongly recommended. In our study, we got high sensitivity and specificity rate in trephine BMB test. Last, but not the least, interpretation of biopsy should be carried out not in isolation but keeping in mind the aspiration findings, as morphology is best assessed in aspiration smears.
Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 5 May 2017
References
- P.Ch.ToiR.G.VargheseR.RaiComparative evaluation of simultaneous bone marrow aspiration and bone marrow biopsy: an institutional experienceIndian J Hematol Blood Transfus2620104144
- F.FendM.KremerDiagnosis and classification of malignant lymphoma and related entities in the bone marrow trephine biopsyPathobiology742007133143
- F.OzkalemkasR.AliV.OzkocamanThe bone marrow aspirate and biopsy in the diagnosis of unsuspected nonhematologic malignancy: a clinical study of 19 casesBMC Cancer52005144
- PatelDiagnostic role of bone marrow aspiration and trephine biopsy in haematological practiceGujrat Med J7020153741
- B.J.BainBone marrow trephine biopsyJ Clin Pathol542001737742
- S.ChandraH.ChandraComparison of bone marrow aspirates cytology, touch imprints cytology and trephine biopsy for bone marrow evaluationHematol Rep32011e222
- T.A.KhanI.A.KhanK.MahmoodDiagnostic role of bone marrow aspiration and trephine biopsy in haematological practiceJ Postgrand Med Inst2822014217221
- A.R.BirdP.JacobsTrephine biopsy of bone marrowS Afr Med J641983271276
- S.KumarA.R.RauR.NaikBone marrow biopsy in non-Hodgkin lymphoma: a morphological studyIndian J Pathol Microbiol522009332338
- F.MoidL.DepalmaComparison of relative value of bone marrow aspirates and bone marrow trephine biopsies in the diagnosis of solid tumour metastasis and Hodgkin LymphomaArch Pathol Lab Med1292005497501
- R.MilosevicG.JankovicN.AntonijevicHistopathologic characteristics of bone marrow in patients of aplastic anemiaSrp Arh Colok Lek1282000200204
- B.D.SabharwalV.MalhotraS.ArunaR.GrewalComparative evaluation of bone marrow aspirate particle smears, imprints and biopsy sectionsJ Postgrad Med361990194198
- S.PileriS.PoggiP.BaglioniHistology and immunohistology of bone marrow biopsy in multiple myelomaEur J HematolSuppl. 511989 952–911
- D.C.FarhiBone marrow granulomas, clinicopathological findings in 72 cases and review of the literatureHematol Pathol219884350
- L.SainiJ.BrandweinR.TurnerIncremental value of the bone marrow trephine biopsy in detecting residual leukemia following treatment for Acute Myeloid LeukemiaLeuk Res4520164752
- P.SubashchandraboseL.R.MadanagopaalS.T.MadhukarDiagnosis and classification of acute leukemia in bone marrow trephine biopsies-utility of a selected panel of minimal immunohistochemical markersInt J Hematol-Oncol Stem Cell Res2015
- M.NaegeleL.LepplaC.Kiote-SchmidtTrained clinical nurse specialists proficiently obtain bone marrow aspirates and trephine biopsies in a nearly painless procedure—a prospective evaluation studyAnn Hematol949201515771584
- S.SreedharanunniM.U.SachdevaN.KumarSpectrum of diseases diagnosed on bone marrow examination of 285 infants in a single tertiary care centerHematology2032015175181
- S.GoyalU.R.SinghU.RusiaComparative evaluation of bone marrow aspirate with trephine biopsy in hematological disorders and determination of optimum trephine length in lymphoma infiltrationMediterr J Hematol Infect Dis6120132014002
- V.SovaniC.HarveyA.P.HaynesA.K.McMillanD.M.ClarkS.R.O'ConnorBone marrow trephine biopsy involvement by lymphoma: review of histopathological features in 511 specimens and correlation with diagnostic biopsy, aspirate and peripheral blood findingsJ Clin Pathol102013 jclinpath-2013
- M.KaurA.P.RanaS.KapoorA.PuriDiagnostic value of bone marrow aspiration and biopsy in routine hematology practiceJ Clin Diagn Res: JCDR882014FC13
- J.M.RayaS.Montes-MorenoA.AcevedoPathology reporting of bone marrow biopsy in myelofibrosis; application of the Delphi consensus process to the development of a standardised diagnostic reportJ Clin Pathol72014 jclinpath-2014