Abstract
Purpose
To evaluate the role of MR Spectroscopy in verification and differentiation of different brain ring enhancing lesions, for better diagnostic purpose and management outcome.
Patients and methods
25 patients were included in this study, 15 of them were males and 10 were females, with age ranging between 21 and 75 (mean 46 ± 14). All patients were presented with variable symptoms, some of them have known primary disease entity and others presented with headache, visual disorders or disturbed level of consciousness. MRI was done to all the patients including conventional and contrast sequences, as well as MR Spectroscopy. Some did MR perfusion and DTI in order to further characterize their nature.
Histopathological findings and results of clinical follow up were our reference standard.
Results
Among the 25 patients, MR Spectroscopy was able to specify 22 lesions (88%), DTI was performed in 13 out of 25 lesions and MR perfusion was performed in 8 out of 25 lesions.
Conclusions
Characterization of ring enhancing lesions of the brain has increased accuracy by applying advanced MRI techniques. In this study, MR Spectroscopy combined with DTI and MR perfusion sequences in some cases improved verification of different ring enhancing brain lesions.
1 Introduction
Ring-enhancing intracranial lesions are considered as common and quite puzzling diagnostic dilemmaCitation1.
To diagnose such lesions; many imaging techniques, including computed tomography and magnetic resonance imaging (MRI) are usedCitation2.
These lesions may present as solitary or multiple on a brain MRI, and are characterized by a contrast enhancing halo with a non-enhancing centerCitation1.
It is still a challenge to differentiate different ring enhancing lesions like abscess, cystic glioblastomas and metastases even with the use of MRICitation3.
Clinical presentations are usually nonspecific and hardly lead to a final diagnosis. For therapy, it is essential to differentiate cerebral abscesses from cystic tumor to initiate adequate early medical and surgical treatmentsCitation3.
Intracranial ring enhancing lesions of different etiologies have a similar appearance on conventional MRI. Differential diagnosis of ring enhancing cystic mass lesions includes primary and secondary brain tumors, metastases, non-neoplastic cysts, and brain abscessesCitation4.
Routine brain MR imaging is very sensitive in the identification of ring enhancing lesions but it lags some specificity, for instance it cannot distinguish between neoplastic and non-neoplastic lesions, in a large percentage of these cases. Frequently, the differentiation of a tumor from an infection is quite difficult, based solely on conventional MRICitation5.
Diseases causing multiple ring-enhancing lesions of the brain are infectious, neoplastic, inflammatory or vascular in origin. Several types of primary and secondary brain neoplasms, such as glioblastomas, low-grade gliomas, lymphomas and brain metastases can also present as multiple ring-enhancing lesions. Many non-neoplastic neurological disorders can mimic brain neoplasms. These lesions may include tuberculosis, cysticercosis, demyelinating disorders, pyogenic abscess, toxoplasmosis, fungal infections, sarcoidosis, Behcet disease, radiation encephalopathy, and some vasculitic disordersCitation6.
Therefore, advanced MR techniques as proton Magnetic Resonance Spectroscopy (1HMRS), Perfusion weighted imaging and Diffusion tractography imaging (DTI) have been employed in the differential diagnosis of these lesions, with variable success ratesCitation7.
The purpose of this study was to examine intracranial ring enhancing mass lesions with advanced MRI techniques and to evaluate the contribution of these techniques to differential diagnosis. For this purpose conventional MR sequences, MR Spectroscopy, DTI and MR perfusion findings were described. The results were compared between different types of ring enhancing lesions for accurate characterization.
2 Patients and methods
2.1 Patient selection
25 patients were selected, between October 2014 and March 2015, 15 of them were males (60%) and, 10 were females (40%) with age range between 21 and 75 (mean 46 ± 14).
All patients were presented with variable symptoms, 8 of them with headache, 5 out of 25 were presented with limb weakness, and another 5 with disturbed level of consciousness, 4 out of 25 patients were presented with visual disorders, and 3 were already known to have primary brain tumor. 15 (60%) of cases were referred from neurologist, and 10 (40%) were referred from neurosurgeon. Other investigations were requested for further confirmation of the diagnosis like CSF aspiration for oligoclonal bands and inflammatory cells, tuberculin test, visual evoked potential as well as histopathology. The results of these investigations were our references to prove our diagnosis. All patients were subjected to MRI study.
2.2 Methods
Patients were examined with 1.5 T MR imaging unit (Siemens, symphony magnetom) with eight-channel head coil. All cases performed axial T1WI, T2WI, FLAIR sequences, sagittal T1WI and coronal T2WI. Sagittal T2WI for the cervical spine was done if multiple sclerosis (MS) was suspected to rule out any cord lesions. Intravenous Contrast enhanced images:
11 cases were referred only for conventional MRI, but when examined by the radiologist, Contrast enhanced sequences were requested for better delineation of the lesions.
Diffusion weighted images (DWI) and ADC map. MR Spectroscopy: was done based on contrast enhanced images, with voxel placement on the most enhancing part of the lesion.
DTI was performed in 13 out of 25 lesions and MR perfusion was performed in 8 out of 25 lesions.
2.3 Image interpretation
All data were referred to the PACS system to be interpreted by two experienced radiologists with at least 5 years’ experience in neuroradiology. The lesions were described regarding site, size, and intensity pattern on T1WI and T2WI, surrounding edema, enhancement pattern on contrast enhancing images. The pattern of MR Spectroscopy profiles was described. DTI and MR perfusion patterns were analyzed for the cases that did these sequences. A weekly meeting panel including radiologist with the referral neurologists and neurosurgeons was hold for cases discussion where the laboratory data were correlated with radiological finding to narrow the differential diagnosis and reach final diagnosis.
3 Results
We relayed on descriptive statistical method in our study results.
25 patients were selected, during the period from October 2015 till March 2016, 15 of them were males (60%) and, 10 were females (40%) with age range between 21 and 75 (mean age 46 ± 14).
Patients were presented with variable symptoms, 7 of them with headache, 4 out of 25 were presented with limb weakness, and another 4 with disturbed level of consciousness, 2 out of 25 patients were presented with visual disorders, and 3 were already known to have primary brain tumor ().
Table 1 The clinical presentation and final diagnosis of the examined population. MRS: MR spectroscopy. DTI: Diffusion Tensor Imaging.
15 (60%) of cases were referred from the Neurology clinic and 10 (40%) were referred from Neurosurgery clinic. Radiological studies together with other laboratory investigations were requested based on the clinical suspicion.
Laboratory investigations, including CSF aspiration for oligo clonal bands and inflammatory cells, tuberculin test, visual evoked potential as well as histopathology were requested for further confirmation of the diagnosis. The results of these investigations were our references to prove the diagnosis.
MRI of the brain without contrast were initially requested in 19 (76%) patients, MRI with contrast was initially requested in 6 (24%) patients. All patients with history of brain tumor did MRI with contrast study from the start. The images were interpreted by one Neuroradiologist and one general Radiologist for deciding the next step.
The final diagnosis was set in the initial examination in 10 cases (40%) (Anaplastic meningioma, subacute hematoma, basal meningeal tuberculosis and brain metastasis), but with a confidence level, about 80% based on the Radiologist subjective evaluation.
MR spectroscopy was requested for 22 out of 25 cases excluding the subacute hematoma. The results of MRS, as shown in , were diagnostic of malignant lesion in 11 cases (44%) (), benign etiology in 11 cases (44%). Cases of hematoma were not submitted to MRS examination.
Fig. 1 45 year old male patient with history of left parietal GBM submitted to surgical excision followed by radiotherapy, he presented with this enhancing parenchymal nodule in post contrast axial T1WI (A) that could be recurrence or radiation necrosis. MRS (B) revealed increase in Choline/NAA ratio and Choline/Cr ratio with mild reduced NAA/Cr ratio. (C) DTI revealed decreased FA value with increased ADC value within the enhancing nodule (arrow) denoting high cellularity of the lesion. (D) Is follow up post contrast T1 after 5 months showing progression in size of the lesion which proved to be recurrent Glioblastoma multiform (GBM).
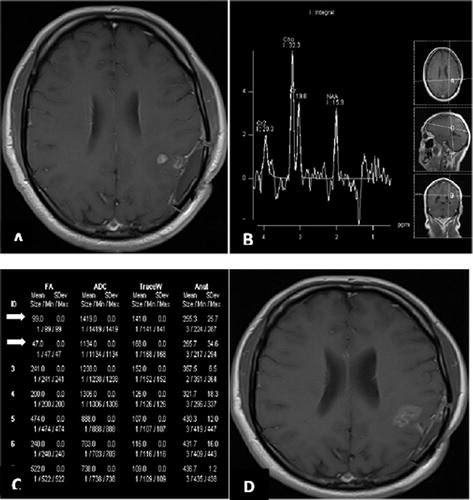
Table 2 Characteristics of MRS in different ring enhancing brain lesions: NAA: N-acetyl aspartate. Cho: Choline. Cr: Creatinine.
Moreover, MRS reached the final diagnosis in 8 (32%) cases of these benign lesions including all cases of tuberculosis, meningioma and multiple sclerosis ().
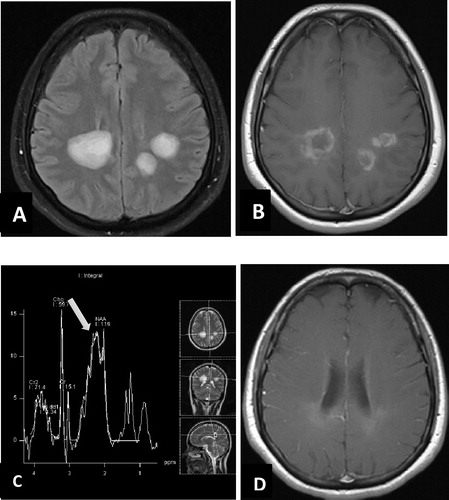
Fig. 2 35 year old female patient with multiple patches of deep white matter hyperintensity on axial FLAIR (A), in post contrast axial T1WI (B) these lesions show irregular ring like marginal enhancement, no perifocal edema or mass effect, MR spectroscopy TE 30 from the lesion (C) shows mild elevation of choline/NAA ratio, marked elevation of glutamine peak at 2.1–2.5 ppm (arrow), large lactate peak at 1.3 ppm, and lipid peak at 0.9 ppm, suggesting tumefactive demyelination process. (D) 2 year follow up post contrast axial T1WI after medical treatment of MS shows remarkable regression.
Finally MR perfusion was done for 2 cases (8%) of recurrent GBM to evaluate the areas of hyper perfusion inside the tumor and to differentiate active recurrent tumor tissue that revealed high perfusion values from necrosis that revealed low perfusion values.
Preoperative DTI was done for 5 cases (2%) including cases of brain stem glioma and fungal abscess for mapping of the affected fibres.
4 Discussion
Brain ring enhancing lesions remain diagnostic challenge as they have wide range of differential diagnoses. New MRI modalities play an important role in verification of brain ring enhancing lesions, preoperative mapping and follow up as well.
Our work was unique in studying wide variety of lesions using different MRI modalities for better accurate verification. In our study, abscess showed absence of Cho, Cr, and NAA and increased concentrations of various amino acids (acetate, alanine, lactate) in MRS, while in glioma, there was high choline/NAA ratio, high choline in the surrounding oedema, this was supported by a study done by Lai et al.Citation8 in 2002 that showed increased amino acids, lactates and lipids in abscess and it showed also peaks of lipids and lactates in cystic glioma in addition to the peak of choline and high choline/NAA ratio.
Another study was elicited by Lai et al.Citation9 in 2008 and found that the Cho levels of rim-enhancing regions of abscesses were significantly lower than those of the rim enhancing GBM. Also they noted that the Cho/Cr ratio is lower than that often seen in GBM. These findings again supported our findings.
In 2001, Hartmann et al.Citation10 strongly suggested that the diagnosis of a brain abscess can be made if there is restricted diffusion within a cystic ring-enhancing cerebral lesion with low ADC values. Yet, the ADC values between and within different studies varied widely. It is possible that variable concentrations of inflammatory cells and bacteria, different etiologic organisms, and the age of the abscess with variable viscosity of the abscess fluid were responsible for these conflicting data.
The present study demonstrates that brain abscess cavity shows regions of increased FA values with restricted mean diffusivity compared with other cystic intracranial lesions. With an increasing use of DTI in surgical planning of brain-tumor resection, one may become more careful in interpreting these changes as oriented axonal fibers.
Gupta et al.Citation11 and Shetty et al.Citation12 studied MRS in differentiation between tuberculoma versus neurocystocercosis and found that MRS of brain tuberculomas commonly detects peaks of lipids attributable to large lipid fractions in tuberculosis bacillus. It will also have increased choline levels and decreased N acetyl aspartate and creatine levels. The choline/ creatine ratio was greater than 1 in all tuberculomas but not in cysticerci .The Proton-MRS allows for non-invasive identification of tuberculoma with high specificity and may allow early instalment of targeted antimicrobial treatment.
These findings were matched with that in our study, when we elicited that in tuberculosis, there are prominent decrease NAA/Cr and slight decrease Cho/NAA, while Lipid/lactate peaks are usually elevated while in cystocercosis, Choline is slightly elevated, lactate and succinate are elevated and NAA.
Different studies highlighted diagnostic difficulties with conventional investigations in ring enhancing lesions in the brain and role of MRS, DWI and other advanced sequences in order to reach accurate diagnosis.
5 Conclusion
Ring enhancing lesions of the brain remain a diagnostic challenging dilemma including a wide differential diagnosis of neoplastic and non-neoplastic lesions. MRI stands as the main diagnostic imaging modality, using conventional as well as advanced sequences can help in accurate verification and differentiation between these lesions for better diagnostic accuracy. Using DTI preoperatively helps to increase postoperative outcome.
Pitfall: The study population is less in number as we were very strict in our inclusion criteria for the purpose of results accuracy. This will give chance to more new research fields in the future with increasing study population number.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 25 May 2017
References
- JG.SmirniotopoulosFM.MurphyEJ.RushingJH.ReesJW.SchroederPatterns of contrast enhancement in the brain and meningesRadiographics272007525551 ISSN 0271–5333
- R.K.GargM.K.SinhaMultiple ring-enhancing lesions of the brainJ Postgr Med562010307316 Department of Neurology, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
- WernerReicheVolkerSchuchardtThomasHagenKamil A.IIyasovPeterBillmannJohannesWeberDifferential diagnosis of intracranial ring enhancing cystic mass lesions—role of diffusion-weighted imaging (DWI) and diffusion-tensor imaging (DTI)Clin Neurol Neurosurg11232010218225
- K.RudreshM.V.KrishnaKarthikJomySebastinClinical and aetiological profile of ring-enhancing lesions on CT brainJIACM92008100102
- http://www.intechopen.com.:. Kapsalaki Eftychia, Gotsis Efstathios D, Tsougos Ioannis, Fountas Konstantinos N. The role of magnetic resonance spectroscopy in the diagnosis of ring enhancing lesions, October 2008; p. 145–158.
- RK.GargMK.SinhaMultiple ring-enhancing lesions of the brainJ Postgr Med562010307316
- Murali B, Baxi B, Spv V. Differential diagnosis of ring enhancing lesions in contrast enhanced CT and MRI with histopathological correlation: Indian study. doi: http://doi:10.1594/ecr2013/C-1234.
- Ping H.LaiJih T.HoWei L.ChenBrain abscess and necrotic brain tumor discrimination with proton MR spectroscopy and diffusion-weighted imagingAm J Neuroradiol23200213691377
- P.H.LaiH.H.WengC.Y.ChenIn vivo differentiation of aerobic brain abscesses and necrotic glioblastomas multiforme using proton MR spectroscopic imagingAJNR29200815111518
- MariusHartmannOlavJansenSabineHeilandClemensSommerKristinMu¨nkelKlausSartorRestricted diffusion within ring enhancement is not pathognomonic for brain abscessAJNR AJNR Am J Neuroradiol22200117381742
- Rakesh K.GuptaKhader M.HasanAsht M.MishraHigh fractional anisotropy in brain abscesses versus other cystic intracranial lesionsAm J Neuroradiol26200511071114
- Shetty Guruprasada, Avabratha Kadke Shreedhara, Rai Boodyar Sanjeev. Ring-enhancing lesions in the brain: a diagnostic dilemma. Iran J Child Neurol 2014; 8: 61–4.
