Abstract
Background
Vaginal adenosis is a rare benign condition with a small percentage of patients at risk of vaginal adenocarcinoma.
Case
A 34 year old woman presented with paravaginal swelling resembling Bartholin’s cyst. Vaginal examination revealed a cystic, fluctuant and non-tender mass on the right lateral vaginal wall measuring 6 by 5 cm. The cervix, uterus, adnexa and Pouch of Douglas (POD) were normal. She had paravaginal cyst excision and histology showed stratified cuboidal epithelial cells with proliferation of numerous glands of small caliber within its wall that are separated by scanty stroma and consistent with vaginal adenosis. No other lesion was found on the genital tract.
Conclusion
Excision and histology is required in suspicious cases of paravaginal cyst to rule out vaginal adenosis, a potential precursor of vaginal adenocarcinoma. Counseling and follow up will help detect early occurrence of adenocarcinoma.
1 Introduction
Vaginal adenosis is defined by the presence of metaplastic cervical or endometrial epithelium within the vaginal wall, considered as derived from Mullerian epithelium islets in later life.Citation1 It is a benign vaginal lesion attributed to intrauterine and neonatal exposure to diethylstilbesterol (DES), other progestogens and non-steroidal estrogens.Citation1,Citation2 They also occur in otherwise healthy women and in some cases have been considered to be idiopathic or congenital.Citation1–Citation3 They are sometimes considered as precancerous lesions as clear cell adenocarcinoma patients have these lesions in close proximity to atypical tuboendometrial glands.Citation2–Citation4 Post pubertal lesions have also been observed to grow de novo.Citation5
Tasuku Mariya et al. reported a case of vesicovaginal fistula caused by vaginal adenosis in a Japanese woman.Citation6 Sedlacek and colleague also documented vulva and vaginal adenosis occurring following CO2 laser treatment.Citation7
Diagnosis can be made from colposcopically directed biopsy of lesion or histology of paravaginal cyst as seen in this case. We present a case of vaginal adenosis resembling Bartholin’s cyst on clinical examination in a young woman who has not been prenatally exposed to DES. However, to our knowledge, no case of vaginal adenosis resembling Batholin’s cyst has been reported in sub-Saharan Africa. We therefore find it necessary to add this report to the existing literature.
2 Case description
A 34 yr old P2+0, 2 alive woman presented in our Gynecological clinic with a 2 year history of vaginal growth which has been progressively increasing in size. The swelling was not painful and there was no vaginal discharge or bleeding. There was superficial dyspareunia but no dysmenorrhea or menorrhagia. There was no past history of in utero exposure to DES, vulva/vaginal warts or perineal surgery. She had never used any hormonal contraceptive or fertility drugs in the past. She is also not currently on any hormonal medication.
Her first confinement was 13 years prior to presentation when she had caesarean delivery for cephalopelvic disproportion. She had a repeat elective caesarean delivery 2 years prior to presentation on account of one previous CS with borderline pelvis.
There was no history of chronic medical disorder. She is married in a monogamous setting with no history of multiple sexual partners. She does not smoke cigarette nor drink alcohol.
Examination revealed a young woman, not pale, afebrile, anicteric, with no pedal edema. Her blood pressure was 110/60 mmHg and chest was clinically clear. There was a healed Pfannenstiel scar on the anterior abdominal wall. Vaginal examination revealed a cystic, fluctuant and non-tender mass on the right lateral vaginal wall measuring 6 by 5 cm (). The cervix, uterus, adnexa and POD were normal. A diagnosis of paravaginal cyst was made to rule out Bartholins cyst. Complete blood count, urinalysis, electrolyte and urea were normal.
Fig. A1 Cystic, fluctuant and non-tender mass on the right lateral vaginal wall measuring 6 cm by 5 cm.

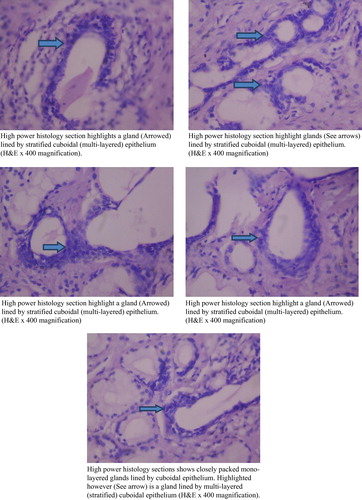
She had excision of the paravaginal cyst () with closure of the vaginal wall using Vicryl 1 sutures under regional anaesthesia (saddle block). She was discharged the second day post-surgery. Histology showed stratified cuboidal epithelial cells with proliferation of numerous glands of small caliber within its wall that are separated by scanty stroma. These glands are lined by single layer of cuboidal epithelial cells that are attenuated in areas. Histologic diagnosis was vaginal adenosis with no evidence of malignancy (–). She did well postoperatively and at present is on follow up in the Gynecological clinic.
Fig. B1 Low power histologic view of the paravaginal cyst showing predominantly proliferation of numerous small glands of small caliber separated by scanty stroma (H&E ×40 magnification).

Fig. B2 Medium power view of the lesion show proliferation of numerous glands of small caliber (arrow) lined by single to bi-layered cuboidal epithelial cells within its wall that are attenuated in areas. They are separated by intervening scanty stroma. (H & E ×100 magnification).

Fig. B3 (a) High power histology section highlights a gland (Arrowed) lined by stratified cuboidal (multi-layered) epithelium (H&E ×400 magnification). (b) High power histology section highlight glands (See arrows) lined by stratified cuboidal (multi-layered) epithelium. (H&E ×400 magnification). (c) High power histology section highlight a gland (Arrowed) lined by stratified cuboidal (multi-layered) epithelium. (H&E ×400 magnification). (d) High power histology sections shows closely packed mono-layered glands lined by cuboidal epithelium. Highlighted however (See arrow) is a gland lined by multi-layered (stratified) cuboidal epithelium (H&E ×400 magnification).
3 Discussion
Vaginal adenosis has become uncommon since the use of DES was stopped by FDA in 1971.Citation8 Absence of any other etiological factor for vaginal adenosis in this patient signifies that its occurrence was most likely spontaneous, possibly from remnant of Mullerian epithelium.
Nearly all women who are exposed to DES especially before 16 weeks gestation during their mothers’ pregnancy will develop vaginal adenosis.Citation8 It is a recognized risk factor for development of vaginal cancer.Citation2–Citation4 Although, DES exposed daughters have an increased risk of developing clear cell adenocarcinoma, women do not have to be exposed to DES to develop this cancer.
This case is important for two reasons. First, is the clinical resemblance of the paravaginal cyst to Bartholin’s duct cyst. This may lower the threshold of a clinician to perform excisional biopsy and histology. Secondly, simple incision and drainage with marsupialization may be performed in such instances thereby missing important diagnosis that has malignant potential.
The clinical presentation of Paravaginal cyst and Bartholin’s cyst are similar as exemplified in this case with vaginal growth and dyspaerunia. The anatomic location of the Paravaginal cyst in this case is also similar to where Batholin’s cysts are usually sited.
Enlargement of Bartholin’s duct cyst in a postmenopausal woman although rare, may signify a malignant process. Despite that this particular case occurred in a woman of reproductive age, it is an eye opener to the importance of careful assessment of any paravaginal or Bartholin’s cyst before intervention. Surgery via cyst excision where indicated with histology of excised tissue(s), in order to avoid missing the diagnosis with grave consequences if there is malignant tendency is of paramount importance.
Excisional biopsy was adequate for cure in this patient; however, in the presence of premalignant or malignant lesion on biopsy, treatment should be aggressive and should involve a Gynecological oncologist. Further evaluation for vulva, vaginal and cervical lesions in this patient revealed no abnormality. This was necessary because there may be concomitant genital lesions occurring with vaginal adenosis that will require treatment.
4 Conclusion
Vaginal adenosis should be considered in any patient presenting with paravaginal cyst. Proper evaluation, excision of the cyst and histology will be helpful in diagnosis, prognosis and further treatment.
Disclosure and conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this manuscript. All authors have approved the final article. The patient in this study gave informed consent for the photographs and photomicrographs used in this manuscript.
Acknowledgements
Special thanks to the medical and paramedical team of health workers who participated in the management of this woman.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 2 June 2017
References
- C.KranlB.ZelgerH.KoflerK.HeimN.SeppP.FritschVulval and vaginal adenosisBr J Dermatol1391998128131
- R.J.KurmanR.E.ScullyThe incidence and histogenesis of vaginal adenosisHum Path51974265276
- A.L.HerbstR.E.ScullyAdenocarcinoma of the vagina in adolescence. A report of 7 cases including 6 clear-cell carcinomas (so called mesonephromas)Cancer251970745757
- A.StaflR.F.MattinglyVaginal adenosis: a precancerous lesion?Am J Obstet Gynecol1201974666667 PMID 4422247
- A.KafkashA.KayikeiogluA.AydinA.BuhurVaginal adenosis without DES exposure: a case reportJ Turgut Ozal Med Center31996356358
- T.MariyaT.SuzukiS.HabataDevelopment of vesicovaginal fistula caused by vaginal adenosis: a case reportOpen J Obstet Gynecol32013435437
- T.V.SedlacekJ.M.RivaA.B.MagenC.E.ManganM.F.CunnaneVaginal and vulva adenosis: an unsuspected side effect of CO2 laser vaporizationJ Reprod Med3519909951001
- G.B.SharpP.ColeVaginal bleeding and diethylstilbesterol exposure during pregnancy; Relationship to genital tract adenocarcinoma and vaginal adenosisAm J Obstet Gynaecol16219909941001

