Abstract
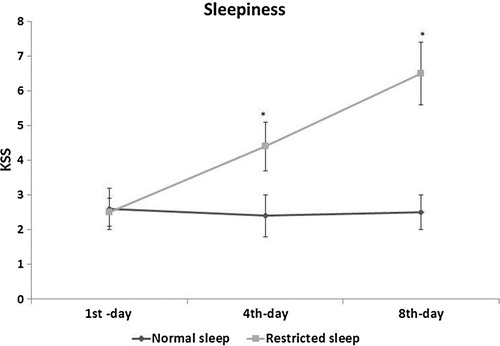
Previous studies have shown that night shift work is thought to be a risk factor for cardiovascular disease and inadequate sleep is a common feature of night shift work. Since it’s more difficult to maintain adequate sleep duration among night watchmen during their working schedule, hence the purpose of our present study was to investigate whether mental stress or fatigue over restricted sleep period in night shift, affects HRV, in order to elucidate on cardiac autonomic modulation among nigh watchmen. With the purpose of this, autonomic activity determined from the levels of the heart rate variability (HRV), and also measured, body mass index (BMI), body fat percentage from skin fold thickness (biceps, triceps, and sub-scapular, supra-iliac) among normal sleep watchmen) (n = 28) and restricted sleep watchmen (n = 28) at first (1st) day, fourth (4th) day and seventh (7th) day of restricted sleep period. We observed that among restricted sleep individuals, sleepiness was significant increase at 4th day and 7th day when compare to normal sleep individuals, and, there was significant increase in, mean NN, VLF, LF, LF(nu), LF/HF AND significant decrease in SDNN, RMSSD, TSP, HF, and HF(nu) at 4th and 7th day of restricted sleep period. In addition to, this variable was more significant increase on 7th day, when compare with 4th day. As well as there was significant negative correlation between LF(nu) and HF(nu) at subsequent 4th day [r (48) = −0.84; P = 0.01] and 7th day[r (48) = −0.95; P = 0.01] of restricted sleep period. However we didn’t observe any significant variation in BMI, and body fat percentage among restricted sleep individuals when compare to normal sleep individuals with in this restricted sleep periods. Hence we concluded that partial sleep loss may cause autonomic imbalance represented by increased sympathetic and decreased parasympathetic activity; as revealed by altered HRV indices observed in this study.
Keywords:
1 Introduction
Inadequate sleep is a common feature of shift work. Sleep loss during shift work is a growing problem in our modern society and may become a major threat for health and wellbeing in the near future and supposed to be a threat for cardiovascular disease (CVD).Citation1–Citation5 Sleep loss may be affecting stress system which plays a critical role in this adaptation.Citation6 Acute sleep loss may be associated with increased heart rate and blood pressure, and a shift of sympathovagal balance toward sympathetic dominance.Citation7,Citation8
The heart rate variability (HRV) analysis is a non-invasive diagnostic technique, has been proposed for the study of autonomic nervous system.Citation9 The heart rate (HR) is modulated by the combined effects of the sympathetic (SNS) and parasympathetic (PNS) nervous systems. Therefore, measurement of changes in HR (heart rate variability or HRV) provides information about cardiac autonomic functioning.Citation10 Slower HRV rhythms (LF) specify increased sympathetic and/or lower vagal activity, whereas faster HRV rhythms (HF) SPECIFY lower sympathetic and/or increased vagal activity. Citation10 Hence, the variability in heart rate, (with reduced heart rate variation), has been proposed as an independent prognostic marker for an imbalance of normal cardiac autonomic control mechanisms.Citation11
HRV is measured using: time-domain, frequency (spectral)-domain, and geometrical analysis methods. In time-domain, SD index and low frequency spectra can reflect a combination of sympathetic and parasympathetic activity while rMSSD, pNN50 and high frequency spectra represent the conditions of parasympathetic activity.
Frequency domain method is analyzed by studying the power spectral density. It provides information about the power distribution across frequencies.Citation9 The two key components are low-frequency band (LF) and high-frequency band (HF). LF is considered to be an indicator for sympathetic activity, in contradiction, HF is determined by vagal effect.Citation9 The LF/HF ratio has been derived from these values to show sympathovagal balance.Citation9
The sympathetic activation is considered to be the main mechanism involved in the development of cardiovascular diseases in sleep impairment.Citation12,Citation13 The impairment of HRV parameters with an increased incidence of adverse cardiovascular and metabolic disorders in sleep loss has been acknowledged.Citation14–Citation16 However, only limited studies have conveyed upon the dynamics of the autonomic nervous system during partial sleep loss or restricted sleep.Citation17–Citation19
Thus, the purpose of our present study was to investigate whether mental stress or fatigue over restricted sleep period for the duration of night shift among nigh watchmen, affects HRV, in order to elucidate on cardiac autonomic modulation.
2 Methods
2.1 Ethics declaration
The study was approved by the local research advisory committee of People College of Medical Science and Research Center (PCMS/OD/2015/1056). The study was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from each subject before the start of the study, and all evaluations were performed at completion of first (1st) day, fourth (4th) day and seventh (7th) day of restricted sleep period.
2.2 Study design
The study population consisted of 50 healthy good sleepers, night watch men ranging in age from 18 to 35 years and underwent a medical interview to ensure that they had a regular sleep/wake schedule. None of the subjects had cardiovascular complication such as hypertension, diabetes mellitus, and hyperlipidemia. The participants were divided into two groups.
Group I-(Normal sleep) (n = 28) - Twenty-eight watchman working in day time and used to have normal sleep in night (≥8 h).
Group II-(Restricted sleep) (n = 22) - Twenty-two watchman working in night time and used to have restricted sleep in night (≤3 h).
2.3 Protocol
2.3.1 Sleep schedule assessment
The participants were instructed to maintain a regular sleep–wake schedule and were monitored. No stimulant of any kind was allowed during the study. For the tests obtained in normal rested condition, instructed to participants to maintain normal sleep in night every day. In sleep restriction condition, participants were also instructed to sleep in night less than three hours (<3 h) for one week in their night shift schedule. All the participants were not allowed to sleep in day time. Participants slept at home and completed scheduled sleep diaries, regularly while at home, the duration of sleep was self-monitored. Total time in bed was recorded with a click button by the subject when getting into and out of bed. Participants reported less sleep during study duration which was also confirmed by monitors. After completion of one week study period, participants visited to the laboratory on the morning at 09:00 a.m for assessment. Each participant was tested after a normal sleep night and after a restricted sleep night in random order. The study was conducted in the department of physiology, peoples college of medical science and research center, Bhopal; India. All the measurement was assessed in the normal resting state, with abstinence from alcohol and caffeine at first (1st) day, fourth (4th) day and seventh (7th) day of restricted sleep period. All laboratory assessments were done in triplicate, at the end of study period.
The following clinical data were recorded: the Karolinska Sleepiness Scale (KSS),Citation20 body mass index (BMI)Citation21 and the percentage of body fatCitation22 was determined from the sum of the thickness of four skinfolds (biceps, triceps, suprailiac and subscapular) by using a Harpenden Skinfold Caliper (British Indicators, Burgess Hill, UK).
2.4 Measurement of HRV indices
To study the HRV, we performed 5-min of consecutive digitized electrocardiographic (ECG) signals recording after completion of restricted sleep periods at first (1st) day, fourth (4th) day and seventh (7th) day. All obtained beats (QRS complexes) were amplified further and reviewed on the analyzer screen to avoid any artificial labeling of the QRS complex. The analysis of HRV was performed by the Kubios HRV (version 1.1, Finland) software after research and correction of artifacts, in accordance with the guidelines issued by the European Society of Cardiology and The North American Society of Pacing and Electrophysiology in 1996.Citation9 We analyzed in time-domain variables: mean NN was the mean of RR intervals of normal sinus beats (mean RR, ms), and RMSSD was the square root of the mean of the sum of the squares of differences between adjacent RR intervals. The standard deviation of the RR-intervals (SDNN, ms), and the root mean square of the difference between successive normal intervals (RMSSD, ms).
In frequency domain analysis, the total spectral power (TSP) was calculated for very-low frequency (VLF, 0.00330.04 Hz), low-frequency (LF, 0.040.15 Hz), and high-frequency bands (HF, 0.15 0.40 Hz). The LF/HF ratio was also included in the statistics. Normalized values of HF (nuHF) and LF (nuLF) bands had been re-calculated using the formulas of nuLFLF/HFLF and nuHFHF/HFLF.
3 Statistical analysis
Data are expressed as Mean ± Standard deviation (SD). All data were analyzed with the SPSS for windows statistical package (version 20.0, SPSS Institute Inc., Cary, North Carolina. Statistical significance between the different groups was determined by the independent student ʻt’ test and the significance level was fixed at p ≤ 0.05 (95% confidence intervals). Finally, Pearson correlation coefficient was used to find correlation between two variables.
4 Results
4.1 Effect of restricted sleep on sleepiness and BMI
The data are summarized in () with mean ± SD. Among all normal and restricted sleep individuals, KSS score was comparable on 1st day of restricted sleep. However at subsequent on 4th day and 7th day of restricted sleep, there was significant increase in KSS score in restricted sleep individual when compare to normal sleep individuals indicating higher levels of sleepiness. In addition to, sleepiness level on 7th day was more significant increase, when compare with 4th day of restricted sleep period.
4.2 Effect of restricted sleep on BMI, skin fold and body fat percentage
The data are summarized in () with mean ± SD. Among all normal and restricted sleep individuals, however, we didn’t observe any significant variation in BMI, skin fold (biceps, triceps, and sub-scapular, supra-iliac) and body fat percentage among restricted sleep individuals when compare to normal sleep individuals with in this restricted sleep periods.
Table 1 Effect of restricted sleep on body mass index (BMI), skin fold and body fat percentage, where * significance change (p ≤ 0.05) compared with normal sleep and # – significance change (p ≤ 0.05) compared with 4th day.
4.3 Effect of restricted sleep on time-domain variables
The data are summarized in () with mean ± SD. The NN, SDNN and RMSSD were comparable in among all normal and restricted sleep individuals on 1st day and of restricted sleep. However at subsequent on 4th day and 7th day of restricted sleep period, NN was significantly increased and SDNN and RMSSD were significantly decreased in restricted sleep individuals when compare to normal sleep individuals. As well as, this variation was more significant change respectively on 7th day, when compare with 4th day of restricted sleep period.
Table 2 Effect of restricted sleep on time and frequency domain of HRV analysis. Where * significance change (p ≤ 0.05) compared with normal sleep and # – significance change (p ≤ 0.05) compared with 4th day.
4.4 Effect of restricted sleep on frequency domain variables
The data are summarized in (, and ) with mean ± SD. Among all normal and restricted sleep individuals, all frequency variable such as TSP, VLF, LF, HF, LF(nu), HF(nu) and LF/HF, were comparable on 1st day and of restricted sleep period. However at subsequent on 4th day and 7th day of restricted sleep period, VLF, LF, LF(nu), LF/HF were significantly increased and TSP, HF, HF(nu) were significantly decreased in restricted sleep individuals when compare to normal sleep individuals. In addition to this variation was more significant change respectively on 7th day, when compare with 4th day of restricted sleep period.
Fig. 2 Effect of restricted sleep on correlation between low frequency [LF(nu)and high frequency [HF(nu)] at 4th day of restricted sleep period.
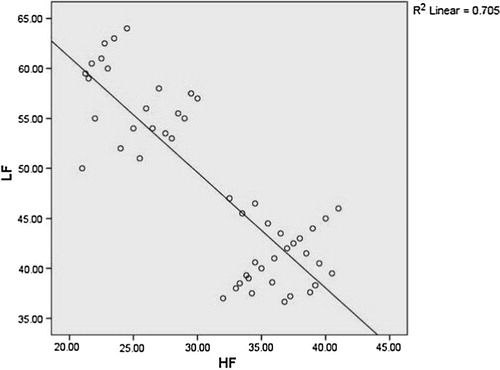
Fig. 3 Effect of restricted sleep on correlation between low frequency [LF(nu)and high frequency [HF(nu)] at 7th day of restricted sleep period.
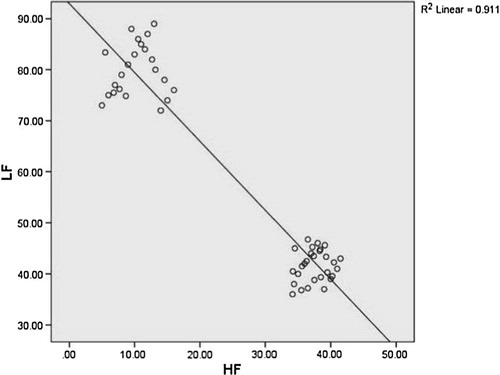
Among all normal and restricted sleep individuals, there was significant negative correlation between LF(nu) and HF(nu) at subsequent 4th day [r (48) = −0.84; P = 0.01] and 7th day[r (48) = −0.95; P = 0.01] of restricted sleep period.
5 Discussion
Partial sleep loss (sleep restriction) and/or accumulated sleep debt has been linked to health problems, including metabolic and cardiovascular disease.Citation23,Citation24 Shift work may possibly have unfavorable effects on autonomic balance, increasing cardiac sympathetic and decreasing parasympathetic activity.Citation25,Citation26 The main aim of this study was to test the hypothesis that partial sleep loss (sleep restriction) during night shift among night watchmen may be associated with an impaired cardiac autonomic modulation. Measurements of heart rate variability (HRV) are increasingly being used as a marker of cardiac autonomic activity during sleepCitation14 and we are conscious that the use of time-domain measurements of heart rate variability as a tool to evaluate the autonomic input to the heart has its limitations, especially when applied to short-term recordings. The foremost limit of time-domain parameters is that they do not provide information about quantitative changes in the activity of each of its two components separately (sympathetic and parasympathetic). On the contrary, power spectral analysis of heart rate variability would provide more quantitative information regarding this.Citation9 However, time and frequency domain measures are strongly interrelated, i.e. for every frequency domain measure there is a time domain measurement that strongly correlates with it (>0.85).Citation27 Even though it is assumed that sleep loss and the risk for CVD are interconnected,Citation28,Citation29 however, only a small number of studies have reported higher sympathetic activity after partial sleep loss (sleep restriction).Citation17–Citation19
The previous study of HRV based on ECG monitoring, observed that mental stress after sleep deprivation for 4 weeks, in healthy college students induces autonomic imbalance and altered HRV indices with an increase in norepinephrine.Citation15 This study reveals that sleep loss associated with mechanisms of chronic mental and physical stress-induces cardiovascular events.Citation15 Slow rhythms of HRV (LF) indicate increased sympathetic and/or lower vagal activity, wakefulness characteristics, whereas fast rhythms of HRV (HF) indicate lower sympathetic and/or increased parasympathetic and vagal activity, sleepy characteristics. Sleep-deprived subjects were exposed to real field driving conditions and ECG and EEG data were collected. A lower ratio of low frequency to high frequency components (LF/HF), and lower LF values were reported on the occurrence of driving errors. sleep-deprived drivers were lower in LF/HF and LF along with driving errors (related to sleepiness) than in those with no driving errors.Citation30 Cardiovascular autonomic modulation were also observed in normal subjects after 36-h sleep loss and shown increased LF and LF/HF as well as decreased HF as per baroreflex sensitivity, which is a measure of the ability of the HR to respond for changes in blood pressure.Citation19 In addition to, one night of sleep loss has been also associated with decreased baroreflex sensitivity in normal individuals.Citation24
There have been a controlled laboratory-based investigations of the autonomic effect of acute sleep loss.Citation14 In the present study, the alteration of HRV indices and a shift of sympathovagal balance toward sympathetic dominance is in consistent with those of earlier reports observed in young men after sleep restriction.Citation19 The observation of the present study also reliable with work concerning sleep restriction over the course of 6 nights results in decreased glucose tolerance and increased sympathetic modulation as evaluated by HRV analysis.Citation18 Similarly, long-term nighttime nurses were found to have higher LF and LF/HF when compared with regular shift nurses, supporting the current hypothesis that disturbed sleep affects cardiac SNS regulation.Citation31 In another study, found that, individuals with frequent nightmares shown significantly higher LF and LF/HF, and lower HF when compare with healthy subjects.Citation32
Sleep loss may also altered the response of the sympathetic–adreno medullary (SAM) system and the hypothalamic–pituitary–adrenocortical (HPA) axis in addition to distressing the autonomic branch of the stress response system.Citation6 The alteration in HPA axis response not only occurs after total sleep deprivation for a continuous period of two days, but it also gradually develops over time with chronic partial sleep restriction.Citation33 This sleep loss not only affects the basal activity of HPA axis but also its subsequent response to a psychological stressor. Rats subjected to prolonged total sleep deprivation or chronic partial sleep deprivation exhibited an altered HPA axis response to restraint stress.Citation33 and also induces a higher occurrence of ventricular premature beats.Citation34,Citation35
Some of the previous studies have observed; there is a significant positive association between short sleep duration and higher BMI along with obesity.Citation36–Citation38 However, our results are not consistent with higher BMI as well as with obesity within this period of restricted sleep, since we didn’t observe any significant change in BMI and body fat percentage in restricted sleep individuals, when compare to normal sleep individuals.
Hence, In view of these, data observed in this study, support the hypothesis that partial sleep loss (sleep restriction) may alters autonomic balance and shift toward sympathetic prevalence because increased low frequency spectral power is an indicator of increased sympathetic nervous system activity and this could be due to either an increase in sympathetic activity or a reduction in parasympathetic tone (or both) or may be an increases the sensitivity to stress-related ectopic activity, mainly consisting in ventricular premature beats. However, further research is needed to investigate the biological mechanisms that link short sleep duration and sympathetic dominance.
6 Conclusions
We conclude that partial sleep loss may cause autonomic imbalance represented by increased sympathetic and decreased parasympathetic activity; as revealed by altered HRV indices observed in this study. These conditions during sleep restriction may lead to increased risk for the development of cardiovascular disorders that are related to increased sympathetic nervous system activity. Therefore, this knowledge will be useful, to enabling risk factors to be modified and the potential to improve health outcomes among night watchmen with early accomplishment.
7 Limitations
The study was based only on men, therefore not allowing a study of the differences according to gender and we didn’t measure the cortisol level to assess the level of mental stress.
8 Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We gratefully acknowledge the financial support provided by the People’s University, Bhopal, India.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 31 May 2017
References
- D.De BacquerM.Van RisseghemE.ClaysF.KittelG.De BackerL.BraeckmanRotating shift work and the metabolic syndrome: a prospective studyInt J Epidemiol382009848854
- T.EllingsenA.BenerA.GehaniStudy of shift work and risk of coronary eventsThe journal of the Royal Society for the Promotion of Health1272007265267
- Y.EsquirolV.BongardL.MabileShift work and metabolic syndrome: respective impacts of job strain, physical activity, and dietary rhythmsChronobiol Int262009544559
- B.H.KarlssonA.K.KnutssonB.O.LindahlL.S.AlfredssonMetabolic disturbances in male workers with rotating three-shift work. Results of the WOLF studyInt Arch Occup Environ Health762003424430
- S.SookoianC.GemmaT.Fernandez GianottiEffects of rotating shift work on biomarkers of metabolic syndrome and inflammationJ Int Med2612007285292
- A.SgoifoB.BuwaldaM.RoosEffects of sleep deprivation on cardiac autonomic and pituitary-adrenocortical stress reactivity in ratsPsychoneuroendocrinology312006197208
- P.LusardiA.MugelliniP.PretiEffects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjectsAm J Hypertens91996503505
- O.TochikuboA.IkedaE.MiyajimaM.IshiiEffects of insufficient sleep on blood pressure monitored by a new multibiomedical recorderHypertension27199613181324
- T.ForceHeart rate variability Standards of measurement, physiological interpretation, and clinical use task force of the European society of cardiology and the North American society of pacing and electrophysiologyEur Heart J171996354381
- J.SztajzelHeart rate variability: a noninvasive electrocardiographic method to measure the autonomic nervous systemSwiss Med Weekly1342004514522
- J.M.DekkerR.S.CrowA.R.FolsomLow heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes The ARIC StudyCirculation102200012391244
- N.GammoudiR.B.CheikhM.A.SaafiG.SaklyM.DoguiCardiac autonomic control in the obstructive sleep apneaLibyan J Med102015
- J.M.MarinS.J.CarrizoE.VicenteA.G.AgustiLong-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational studyThe Lancet365200510461053
- P.K.SteinY.PuHeart rate variability, sleep and sleep disordersSleep Med Rev1620124766
- B.TakaseT.AkimaK.SatomuraT.MastuiM.IshiharaA.KuritaEffects of chronic sleep deprivation on autonomic activity by examining heart rate variability, plasma catecholamine, and intracellular magnesium levelsBiomed Pharmacother582004S35S39
- H.P.Van DongenG.MaislinJ.M.MullingtonD.F.DingesThe cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivationSleep-New York Then Westchester262003117129
- F.SauvetG.LeftheriotisD.Gomez-MerinoEffect of acute sleep deprivation on vascular function in healthy subjectsJ Appl Physiol10820106875
- K.SpiegelR.LeproultE.Van CauterImpact of sleep debt on metabolic and endocrine functionThe Lancet354199914351439
- X.ZhongH.J.HiltonG.J.GatesIncreased sympathetic and decreased parasympathetic cardiovascular modulation in normal humans with acute sleep deprivationJ Appl Physiol98200520242032
- L.ReynerJ.HorneFalling asleep whilst driving: are drivers aware of prior sleepiness?Int J Legal Med1111998120123
- S.KleinD.B.AllisonS.B.HeymsfieldWaist circumference and cardiometabolic risk: a consensus statement from shaping America's health: association for weight management and obesity prevention; NAASO, the obesity society; the American society for nutrition; and the American diabetes associationObesity15200710611067
- J.DurninJ.WomersleyBody fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 yearsBr J Nutr3219747797
- N.T.AyasD.P.WhiteJ.E.MansonA prospective study of sleep duration and coronary heart disease in womenArch Int Med1632003205209
- Y.OgawaT.KanbayashiY.SaitoTotal sleep deprivation elevates blood pressure through arterial baroreflex resetting: a study with microneurographic techniqueSleep-New York then Westchester262003986989
- A.L.HolmesH.J.BurgessK.McCullochDaytime cardiac autonomic activity during one week of continuous night shiftJ Hum Ergol302001223228
- L.Van AmelsvoortE.SchoutenA.MaanC.SwenneF.KokOccupational determinants of heart rate variabilityInt Arch Occup Environ Health732000255262
- P.K.SteinM.S.BosnerR.E.KleigerB.M.CongerHeart rate variability: a measure of cardiac autonomic toneAm Heart J127199413761381
- J.E.GangwischS.B.HeymsfieldB.Boden-AlbalaShort sleep duration as a risk factor for hypertension analyses of the first national health and nutrition examination surveyHypertension472006833839
- S.TaheriL.LinD.AustinT.YoungE.MignotShort sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass indexPLoS Med12004e62
- Michail E, Kokonozi A, Chouvarda I, Maglaveras N, eds. EEG and HRV markers of sleepiness and loss of control during car driving. In: Engineering in medicine and biology society, 2008 EMBS 2008 30th annual international conference of the IEEE; 2008: IEEE.
- M.-H.ChungT.B.KuoN.HsuSleep and autonomic nervous system changes—enhanced cardiac sympathetic modulations during sleep in permanent night shift nursesScand J Work Environ Health2009180187
- T.NielsenT.PaquetteE.SolomonovaChanges in cardiac variability after REM sleep deprivation in recurrent nightmaresSleep332010113122
- P.MeerloM.KoehlK.Van der BorghtF.TurekSleep restriction alters the hypothalamic-pituitary-adrenal response to stressJ Neuroendocrinol142002397402
- A.SgoifoS.F.De BoerC.WestenbroekIncidence of arrhythmias and heart rate variability in wild-type rats exposed to social stressAmerican Journal of Physiology-Heart and Circulatory Physiology.2731997H1754H1760
- A.SgoifoJ.KoolhaasS.De BoerSocial stress, autonomic neural activation, and cardiac activity in ratsNeurosci Biobehav Rev231999915923
- K.L.KnutsonE.Van CauterAssociations between sleep loss and increased risk of obesity and diabetesAnn N Y Acad Sci11292008287304
- M.SinghC.DrakeT.RoehrsD.HudgelT.RothThe association between obesity and short sleep duration: a population-based studyJ Clin Sleep Med12005357363
- R.D.VoronaM.P.WinnT.W.BabineauOverweight and obese patients in a primary care population report less sleep than patients with a normal body mass indexArch Intern Med16520052530