?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
“Selective peripheral neurotomies” (SPNs) are indicated for the treatment of refractory focal and multifocal spasticity of lower limbs in adults.
Objective
To evaluate the surgical results of selective peripheral neurotomies in 20 adult patients who had refractory focal & multifocal spasticity of the lower limbs, follow up period of one year.
Patients and Methods
Prospective study included 20 adult patients who had refractory spasticity of the lower limbs. Preoperative evaluation for muscle tone using Modified Ashworth Score (MAS), muscle power using Medical Research Council Scale (MRCS), functional assessment using Oswestry Functional Scale (OFS) and Range Of Motion (ROM) using manual goniometry were done for all patients. All cases underwent surgery in the form of SPN of tibial, obturator, sciatic and/or femoral nerves. Follow up of the patients was done at 10th day, 3, 6 months and one year postoperatively.
Results
The mean age of patients was 31.35 ± 12.42 years. There were statistically significant improvement of muscle tone, muscle power, functional assessment and range of motion between preoperative and one year postoperative values. Improvement of the muscle tone was from a preoperative Mean ± SD of 3.60 ± 0.68 on MAS to a postoperative 2.30 ± 0.86 at one year, improvement of muscle power on MRCS was from preoperative Mean ± SD 3.75 ± 1.08 to postoperative 4.08 ± 0.69 at one year, There was a functional improvement from a preoperative Mean ± SD of 3.0 ± 0.73 on OFS to 3.60 ± 0.60 at one year postoperatively. Also, there was a significant improvement between preoperative ROM Mean ± SD 61.25 ± 15.29 and one year postoperatively 72.25 ± 12.19.
Conclusions
Selective peripheral neurotomies could effectively improve muscle tone, muscle power, functional performance & range of motion in patients with refractory focal and multifocal spasticity in the lower limbs.
1 Introduction
Peripheral neurotomies (PNs) are old neurosurgical techniques that were introduced hundred years ago. Recently, the development of microsurgical techniques and electrophysiological monitoring lead to the reintroduction of PNs. PNs are dedicated for severe focal and multifocal spasticity, when injection of botulinum toxin becomes ineffective and surgery cannot be delayed any more.Citation1–Citation3
Peripheral neurotomies aim at restoring the balance between the muscle tone of agonist and antagonist muscles by lowering excessive spasticity. Spasticity is decreased in PNs by sectioning the efferent motor fibers of the stretch reflex of the nerve supplying the target muscle.Citation3
Surgery should be done so that the increased hypertonia is minimized without a drop of the useful muscle tone or loss of the motor and sensory residual functions. PNs can be done “selectively” by microsurgical dissection of the motor fascicles and their monitoring using intra-operative electrical nerve stimulation.Citation3–Citation8
Neurotomy consists of sectioning part of one or several motor fascicles of the nerves innervating the target muscle(s), in which spasticity is excessive. Motor branches should be targeted where they are isolated from the nerve trunk or they can be dissected and identified as motor fascicles within the nerve trunk before giving a known branch.Citation8
There is no standardized basis for the extent of the partial section. However, most experienced spasticity surgeons agree that motor fascicles sectioning must include 50–80% (usually 75%) of the fibers supplying a targeted muscle. Before doing any PN, nerve block test of the motor nerves innervating the target muscles is recommended.Citation7,Citation9
2 Aim of the work
The aim of this work was to evaluate the surgical results of “selective peripheral neurotomies” of tibial, obturator, sciatic and/or femoral nerves in 20 adult patients who had refractory focal and multifocal spasticity of the lower limbs.
3 Patients and methods
This was a prospective study which included 20 patients who had refractory focal or multifocal spasticity of the lower limbs. The study was done in the “Department of Neurosurgery, Ain-Shams University Hospitals, Cairo, Egypt” in the period between November 2014 and November 2016. Ethics committee approval for the study design and statistical methodology was obtained.
3.1 Inclusion criteria
Age > 18 years old.
Focal or multifocal spasticity refractory to optimal pharmacological andor physical therapy.
Positive anesthetic nerve block test.
3.2 Exclusion criteria
Negative anesthetic nerve block test.
Contraindication to surgery and
or anesthesia.
Selection and assessment of patients were performed carefully by assessment of muscle tone by “Modified Ashworth Score” (MAS),Citation10 motor power function using “Medical Research Council Scale” (MRCS),Citation11 function assessment by “Oswestry Function Scale” (OFS)Citation12 and range of motion (ROM) assessment by manual goniometry.
Assessment of MAS, MRCS and ROM were performed only for muscle groups involved in harmful spasticity (muscle groups that underwent neurosurgical intervention) and the mean of the scores were used for pre and post- operative statistical evaluation. For statistical analysis purposes, the grade of 1+ on the MAS was considered a 2, and 1 was added to the remaining grades, so the grades ranged from 0 to 5.
Visual gait analysis and videotaping were done for all selected patients with focal and multifocal lower limb spasticity to aid in differentiating harmful spasticity from functionally useful spasticity. Nerve blocks with 3 ml of 0.25% xylocaine were used for predicting the outcome of peripheral neurotomy insuring patients' satisfaction.
All surgeries were performed under general anesthesia and without long-acting muscle relaxants so that the motor responses elicited by nerve stimulation of motor branches could be detected.
Microsurgical resection of at least 50% of the targeted motor branches was performed. The surgical planning was taken in a multidisciplinary approach for each patient, depending on the degree of preoperative spasticity, the functional performance, and the presence of muscle or bony deformities.
Tibial neurotomy was indicated for spastic foot deformity, sciatic neurotomy for hamstring hypertonia, obturator neurotomy for adductor spasm, and femoral neurotomy for hypertonic quadriceps femoris.Citation13,Citation14
Post-operative evaluation visits were scheduled at the 10th day, 3rd month, 6th month and one year; evaluation measures were recorded for each patient for statistical comparison with the pre-operative measurements.
3.3 Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. The Kolmogorov-Smirnov test was used to verify the normality of distribution Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level. We used Wilcoxon signed ranks test for abnormally distributed quantitative variables, to compare between two periods.Citation15,Citation16
4 Results
Twenty patients were included in this study; 13 males (65%), the mean age was 31.35 ± 12.42 years. Eleven patients (55%) had paraparesis, seven patients (35%) had hemiparesis, and two patients (10%) had quadriparesis. Different etiologies of spasticity in this study were described in ().
Table 1 Distribution of different etiologies of spasticity in this study.
A total of 60 selective peripheral neurotomies were performed: 28 were tibial, 15 were obturator, 15 were sciatic, and 2 were femoral neurotomies. Multiple level neurotomies were done as a single staged surgery.
Orthopedic surgeries for muscle contracture were done simultaneously with neurotomies in six patients (30%).
4.1 Muscle tone
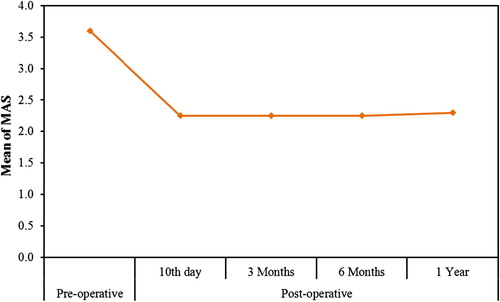
There was a marked reduction of the muscle tone from a preoperative mean MAS of 3.60 ± 0.68 to a postoperative score of 2.25 ± 0.79 at the 10th day, 3 months, 6 months and 2.30 ± 0.86 at one year postoperatively (p < 0.001) ( and ).
Table 2 The change in the muscle tone (MAS) through the study period.
4.2 Muscle power
There was no statistically significant difference between preoperative evaluation and the 6th month follow up assessment (p = 0.066). However, there was a statistically significant change at the one year follow up assessment (p = 0.041) ().
Table 3 The change in the muscle power according to MRCS through the study period.
Five patients (25%) showed improvement on MRCS. However, a decrease of 1–2 grades in muscle power by MRCS in the operated limb was found in almost all patients in the early post-operative period. This may be related either to surgical manipulations of the nerves or to the pre-existing weakness (due to UMNL) became unmasked after resolving of spasticity. Power and selective motor control then improved later, especially after regular rehabilitation.
4.3 Range of motion
There was a statistically significant change in the joints ROM at the 6th months and the one year follow up assessment (p < 0.001) ().
Table 4 The change in the joint ROM thorough the study period.
4.4 Functional assessment
The changes in the mean OFS was significant at the 6th month and one year evaluation visits (p < 0.001). Twelve patients (60%) showed functional improvement of 1 grade on OFS by the end of the first year post-operatively, while the remaining eight patients (40%) did not show any functional improvement ().
Table 5 The change in the Oswestry Functional Scale through the study period.
4.5 Complications
Two patients who were subjected to selective tibial neurotomies had paresthesias of the lateral aspect of the leg and foot. Gabapentin was prescribed for both of them and they showed improvement of symptoms by the 3rd month post-operative evaluation visit.
5 Discussion
Spasticity is referred to increased tone of the muscle due to hyper-excitable stretch reflex. This hyperactive spinal reflex is the result of the loss of inhibitory signals from the descending supraspinal control. It is a component of the upper motor neuron syndrome and may be associated with muscle weakness and absence of selective motor control.Citation13
Treatment of spasticity is not indicated just for the presence of stiffness because sometimes spasticity is helpful to the patient to maintain balance and to compensate for muscle weakness. Taking this in mind, spasticity should only be treated when hypertonia leads to more functional losses, reducing locomotion, enhancing deformities, or causing pain (i.e. harmful spasticity).Citation13
The technological advances in microsurgical techniques have made PN more selective by finely dissecting the fascicles using microsurgery and by using intra-operative electrical stimulation for mapping to better identify the function of the individual nerve fascicles.Citation7–Citation9
In this study, SPNs were performed for 20 adult patients with refractory lower limb spasticity. Almost all patients showed improvement post operatively in the10th day which continued all through the follow up period of one year.
In agreement with our study, Rousseaux et al.Citation17 reported a lasting drop in spasticity (2.5 points on the MAS).
In the current study, the muscle tone showed a statistically significant decrease on MAS which unmasked underlying motor power in about 25% of patients. This explains how removing the harmful spasticity can allow the muscle to function better with improvement of the active movements and of gait and balance in ambulatory patients. The discomfort caused by spasticity is relieved too.
In this study, there were two patients (10%) suffering from transient paresthesias following tibial neurotomy which may be due to potential damage to the sural nerve. This result was in agreement with Buffenoir et al.Citation18, who reported that 5.45% of his patients developed transient paresthesias.
After tone lowering by neurosurgical interventions for spasticity, some patients may have residual fixed muscle contractures or bony deformities that, if not corrected at the same time of neurotomy, should be fixed in another session.
Improvement in MRCS and OFS are more evident at 6 months and 1 year follow-up visits. This result was in accordance with FouadCitation19 who stated that the outcome of PN also intimately depends on the postoperative care after a successful surgery and physical therapy beginning on the second postoperative day. So rapidly the patient should undergo a program of physical and occupational therapy for at least six months.
6 Limitations of the study
The number of patients included in this study is too small for comparing cerebral and spinal origin spasticity. So, we need further research to address the difference in outcome of “selective peripheral neurotomy” between spasticity of cerebral origin and spasticity of spinal origin.
7 Conclusions
A multidisciplinary program for the treatment of disabling spasticity resistant to physical and medical therapy has to be tailored to the individual problems of each patient to avoid insufficient surgery or the loss of motor power in the target muscles.
Selective peripheral neurotomies could effectively improve muscle tone, power, range of motion & functional performance in adult patients with refractory focal or multifocal spasticity of the lower limbs. Multilevel “selective peripheral neurotomies” can be combined for the treatment of one patient in one staged surgery.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 8 July 2017
References
- A.StoffelThe treatment of spastic contracturesAm J Orthop Surg2101913611644
- P.FilipettiP.DecqL’apport des blocs anesthésiques dans l’évaluation du patient spastiqueNeurochirurgie492003226238
- C.GrosLa chirurgie de la spasticitéNeurochirurgie231972316388
- M.SindouB.AbdennebiD.BoissonM.EyssetieA.GoutelleTraitement du pied spastique par la neurotomie selective du nerf tibialNeurochirurgie311985189197
- P.MertensLes neurotomies périphériques dans le traitement des troubles spastiques des membres PhD Thesis1987Faculty of Medicine, University of LyonLyon
- C.GrosSpasticity: Clinical classification and surgical treatmentΗ.KrayenbühlJ.BrihayeF.LoewV.LogueS.MingrinoB.PertuisetAdvances and technical standards in neurosurgeryvol. 61979SpringerNew York, Wien5597
- M.SindouP.MertensSelective neurotomy of the tibial nerve for treatment of the spastic footNeurosurgery231988738744
- P.MertensM.SindouSelective peripheral neurotomies for the treatment of spasticityM.SindouR.AbbottY.KeravelNeurosurgery for spasticity: a multidisciplinary approach1991SpringerNew York, Wien119132
- P.MertensM.SindouSurgical management of spasticityM.P.BarnesG.R.JohnsonUpper motor neurone syndrome and spasticity: clinical management and neurophysiology2nd ed.2008Cambridge University PressCambridge193213
- R.BohannonM.SmithInterrater reliability of a modified Ashworth scale of muscle spasticityPhysTher6721987206207
- M.A.JamesUse of the medical research council muscle strength grading system in the upper extremityJ Hand Surg3222007154156
- P.DecqP.FilipettiJ.LefaucheurEvaluation of Spasticity in adultsOper Tech Neurosurg72005100108
- P.DecqE.CunyP.FilipettiA.FeveY.KeravelLes neurotomies périphériques dans le traitement de la spasticité. Indications, technique et resultats aux membres inferieursNeurochir4431998175182
- P.DecqM.ShinJ.Carrillo-RuizSurgery in the peripheral nerves for lower limb spasticityOper Tech Neurosurg72005136146
- S.KotzN.BalakrishnanC.B.ReadB.VidakovicEncyclopedia of statistical sciences2nd ed.2006Wiley-InterscienceHoboken, N.J.
- L.A.KirkpatrickB.C.FeeneyA simple guide to IBM SPSS statistics for version 20.0Student ed.2013Wadsworth, Cengage LearningBelmont, Calif.
- M.RousseauxN.BuissetW.DaveluyO.KozlowskiS.BlondLong-term effect of tibial nerve neurotomy in stroke patients with lower limb spasticityJ Neurol Sci27820097176
- k.BuffenoirT.RoujeauF.LapierreP.MeneiSpastic equinus foot: Multicenter study of the long-term results of tibial neurotomyNeurosurgery55200411301137
- W.FouadSelective neurotomy of the tibial nerve for treatment of spastic footAlex J Med472011325331