Abstract
Objective
The study aims to clarify the sensitivity of the CTU, and if is it coast effective and time effective to be used as first and the one-stop shop imaging modality for the diagnosis of the different ureteric diseases.
Patients and methods
400 patients with different urinary tract complaints (hematuria and/or renal colic) did triphasic CTU examinations, for diagnosis of suspected obstructive or traumatic ureteric uropathy from January 2014 to October 2016. These patients were filtered from a larger number of patients – who were presented with urinary tract complaints by plain KUB X ray and US, which showed no explaining kidneys or urinary bladder pathology.
Results
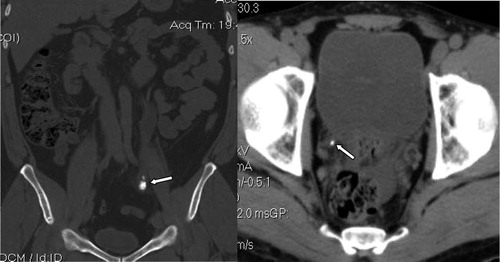
Ureteric duplication was detected in 5 (1.25%) patients, ectopic ureter in one patient (0.25%), UPJ stricture in 4 patients (1%), PUJ vascular impression in 2 patients (0.5%), ureteric calculus in 103 patients (25.75%), pyogenic ureteritis in 8 patients (2%), ureteritis cystica in one patient (0.25%) TCC in 3 patients (0.75%), PRPF in one patient (0.025%) and Trauma in one patient (0.025%).
Conclusion
CTU is very sensitive tool of imaging and could be confidently considered the one-stop shop imaging tool for accurate diagnosis of the different ureteric lesions.
Abbreviations:
- AGH
- Al-Mana General Hospital
- CTU
- computed tomography of the urinary tract
- ESWL
- extracorporeal shock wave lithotripsy
- HIV
- human immune-deficiency virus
- HU
- Hounsfield unit
- IVU
- intravenous urography
- MSCT
- multislic CT scan
- PRPF
- primary retroperitoneal fibrosis
- PUJ
- pelviureteric junction
- RTA
- road traffic accidents
- TCC
- transitional cell carcinoma
- UT
- urinary tract
- VUJ
- vesicoureteric junction
- VUR
- vesicoureteric reflux
1 Introduction
The ureter is responsible for a considerable share of the urinary tract complaints, which are renal colic or pain, hematuria and impaired renal functions. Being retroperitoneal in position, of thin caliber and long course; it is not always easy to diagnose ureteric lesions, by conventional imaging methods like plain KUB, US or even IVP. So, it is not uncommon to miss some ureteric lesions at its early presentation, which will be definitely reflected upon the outcome and prognosis of such disease. Also, its small caliber makes it possible for small ureteric lesions to completely obstruct its lumen causing obstructive nephropathy, with resultant impaired renal function.Citation1
Anatomically, the ureter is a long thin duct which connects urine from the kidney to the urinary bladder. Proximally, it arises from the renal pelvis at the pelviureteric junction (PUJ) and ends distally into the urinary bladder at the vesicoureteric junction (VUJ) (). It leads a complete retroperitoneal course, having around 25 cm length, with less than 3 mm caliber width. Histologically, it is lines with a layer of urothelium surrounded by a smooth muscle layer that allows peristaltic contractions. So, it may be normally not thoroughly opacified at CTU, as there may be some contracted non opacified segments at the time of the scan. However, the absence of an obstructive cause and lack of proximal dilatation is the clue to consider it a physiological not pathological phenomenon.Citation2
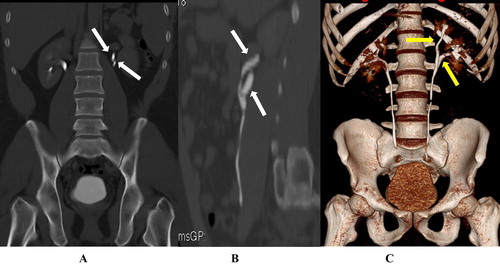
Fig. 1 (A) CRF, (B) SRF& (C) VR CTU showing: Left short segmental upper ureteric duplication (Arrows).
After advent of the multislic CT scan, CTU had been increasingly requested during the last decade as the first urinary tract imaging modality. With the continuously developing MSCT scan advances of CT urography, it is crucial for radiologists to be acquainted with the normal ureteral anatomy and the different ureteral pathologies. These pathologic findings at CT urography include congenital abnormalities, urolithiasis, inflammations, neoplastic lesions and course abnormalities. As any imaging technique, it has sensitivity and specificity scores as well as some advances and some limitations. Also, many technical points are important to be issued in attempt to get perfect study with no technical errors.Citation3,Citation4
2 Aim of the study
The study aims to clarify the sensitivity of the CTU for diagnosis of different ureteric diseases and if is it coast effective and time effective to be used as first UT imaging modality for different clinically suspected ureteric diseases.
3 Patients and methods
3.1 Patients
400 patients with different urinary tract complaints (hematuria and/or renal colic) were referred to CT scan division of the radiology department of Al-Mana General Hospital (AGH), with a suspected ureteric obstructive uropathy from January 2014 to October 2016. These patients were filtered from a larger number of patients – who were presented with urinary tract complaints by plain KUB X ray and US, which showed no explaining kidneys or urinary bladder pathology. The study protocol was approved by the scientific and ethics committee in Al-Mana General Hospital (AGH). A signed consent was obtained from all study candidates, including detailed description of the technique with the rare possible drawbacks.
3.2 Technique
For CTU ureteric examination, there are worldwide three different used techniques; the triple phase, the dual split bolus phase and dual energy CT (DECT) one phase. In all techniques, adequate patient’s hydration is crucial before IV contrast administration. In our hospital protocol, we used to give 250 ml IV saline 0.9%, just before the start of the examination or 1000 ml oral distilled water 4 h before the examination. This generous pre-contrast hydration improves the diuresis, which helps to attain considerable or adequate filling of the collecting system with contrast and protects against the possible serious contrast induced nephropathy (CIN). This CIN could be explained by the usual decrease in renal perfusion which may last for 20 h following IV iodinated contrast administration, resulting in relative medullary hypoxemia and poor contrast elimination.Citation5–Citation7
We used to apply the triple phase technique as a routine CTU protocol in our department. First, a non-contrast phase was done, and then automated injection of 1.5 ml/kg intravenous nonionic contrast media (Omnipaque 300) as a single bolus. Nephrographic phase was allowed to run 100 s after the bolus, then after 10–15 min we used to run the last excretory phase. The whole study CT examinations were done through Philips Brilliance 64 CT Scanner, Philips Medical System, Nederland. B.V. Veenpulis 4–5, 4684 PC Best, Netherlands.
3.3 Post-processing and image interpretation
There are different post-processing data reconstructions programs that vary from place to place for the urinary tract CT examination, however there are some commonly shared and agreed protocols for ureteric examinations. Starting with evaluation of the initial non-contrast phase is the rule, as it detects the stones and the initially hyperdense abnormalities like blood clots. Also, it delineated the base line density of the lesion to determine the degree of its enhancement. After evaluation of the non-contrast phase, you could stop the examination with no going further ahead, if there is a hyperdense ureteric stone explaining the complaint of the patient, who was presented by acute renal colic. Hence, the importance for the technique to be supervised by the radiologist.Citation8,Citation9
Revision of the source images of the axial excretory phase is the second step we used to do after checking the non-contrast phase. It is advised to use wide window measures- like bone window sets- to review this excretory phase, as this helps to perfectly diagnose subtle lesions that may be hidden by contrast material at the narrow soft tissue window sets. In our protocols, we used to do manual windows adjustment with different window length and width figures to attain different densities of the excreted contrast material, which helps to minimize the messing errors. Also routinely we used to do different reformat sets in coronal and sagittal reconstructed images with the use of maximum intensity projection (MIP) tools. Despite time consuming, this multiplanar different windows revision helps much to increase the sensitivity of the examinations, in comparison with source images revision only.Citation9,Citation10
4 Results
Ureteric duplication was detected in 5 (1.25%) patients, ectopic ureter in one patient (0.25%), UPJ stricture in 4 patients (1%), PUJ vascular impression in 2 patients (0.5%), ureteric calculus in 103 patients (25.75%), pyogenic ureteritis in 8 patients (2%), ureteritis cystica in one patient (0.25%) TCC in 3 patients (0.75%), PRPF in one patient (0.025%) and Trauma in one patient (0.025%) (see ).
Table 1 Results of CTU examinations.
5 Discussion
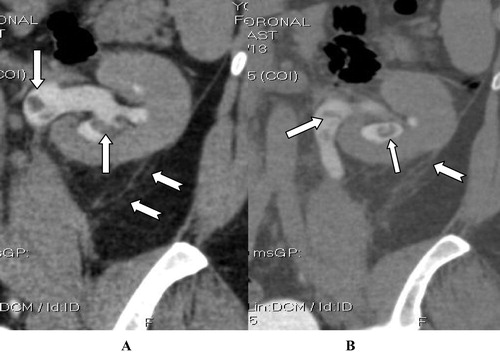
Different congenital anomalies and acquired ureteric abnormalities were diagnosed by triple phase CTU at this study. The congenital ureteric lesions included variable types of ureteric duplications, as they were reported in 5 patients (1.25%) (). The partial duplication is more common, and occurs when there is failure of fusion of the primitive separate upper and lower pole ureters. This leads to partially separated upper ureters with variable length, which unite before the vesicoureteric junction. Fortunately, partial duplications are much more common than complete duplications.Citation11,Citation12 The partial type is usually discovered incidentally with other abnormalities e.g. infection, calculus or neoplastic ().
Fig. 2 (A and B) CTU CRF excretory phase in another patient with longer duplication ureteric segments (Arrows); medially displaced by large left renal Bosniak IVcystic neoplastic lesion (Chevron).
Complete duplication of the ureters down to VUJ, where there are separate distal ureteric openings, is relatively uncommon. It is a known predisposing factor for some urinary tract diseases; like increased risk of repeated urinary tract infection, obstruction, and vesicoureteric reflux (VUR). According to Weigert-Meyer rule, the lower moiety ureter ends distally at a urinary bladder superolateral abnormal position, while the upper moiety ureter ends at an abnormal inferiomedial location. The lower moiety ureter is commonly associated with vesicoureteric reflux, due to abnormal higher position with lack of sphincteric control. The upper moiety distal ureteric end could be at the normal trigonal site, or not uncommonly at other ectopic vesical or extravesical sites.Citation13,Citation14
This ectopic distal ureteric termination may be also seen in non-duplicated ureters; as seen in one patient of this study (0.25%) (). The ectopic ureter in females usually presents with urinary incontinence due to the usual insertion of the ectopic feminine ureter below the external urethral sphincter. In contrast to males, whose ectopic ureter may insert on the posterior urethra, seminal vesicle, vas deferens, bladder neck, or prostate, hence it commonly has obstructed distal end. Males with ectopic ureter do not present with incontinence because unlike females, their ectopic ureter has a distal end superior to the level of the external urethral sphincter. Males with an ectopic ureter commonly present with a urinary tract infection. One of the beneficial applications of CTU is its higher sensitivity for accurate diagnosis of this duplication anomaly. It is much more sensitive than the conventional IVU, as it can clearly show it even in cases with non-functioning anomalous side kidney, which is not uncommon in the complete duplication type with ectopic ureteric orifices or severe VUR.Citation15
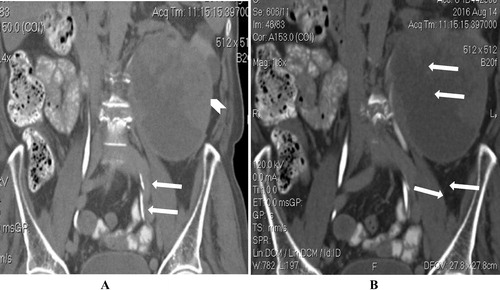
Fig. 3 Non-contrast CTU (impaired renal function) (A, B and C CRF), (D SRF) and (E and F axial cuts) showing ectopic left ureter (Arrows) with distal end at the left seminal vesicle superolateral corner (Curved arrow) and left full length hydroureter and severe left renal hydronephrosis (Notched arrow). Compare with the normal right vesicoureteric junction (Chevron in E and F).
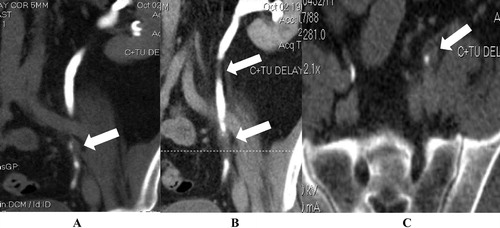
Inherited proximal ureteric spastic smooth muscle dysfunction at the level of the UPJ results in congenital UPJ stricture, which in turn results in impaired emptying of the renal pelvis and renal back pressure. This occurs due to an embryonic insult to the smooth muscle cells at the upper ureter, leading to proximal ureteric localized muscular dysfunction of different degrees. This in turn results in different degrees of hydronephrosis according to the severity of the stricture and the time of discovery. The rest of the ureter shows normal caliber, despite this uppermost segmental anomaly. This abnormality was seen in 4 patients of this study (1%) with different degrees of hydronephrosis and different ages of presentation averaging 14 years (). CTU images had confidently delineated the stricture point and excluded other ureteric obstructive etiology, as well as perfect severity determination.Citation16,Citation17 Extrinsic compression with the renal vessels – as seen in two patients (0.5%)- may give similar renal pelvis dilatation features in IVU study; hence the importance of CTU study which may affect the urologic management, particularly if an endoscopic repair is plannedCitation18,Citation19 (). Hence the importance of triphasic technique in CTU examinations which enables accurate evaluation of the opacified renal artery and vein in the arterial and nephrogenic phases, respectively which may be of limited efficacy if we used dual phase split bolus technique.Citation3,Citation17
Fig. 4 CTU Excretory phase (A and B) CRF, (C and D) SRF: showing localized PUJ stricture (Arrow). Marked dilatation of the right renal pelvis and calyces. A urine–contrast level is seen layering posteriorly in the dilated calyces. (Notched arrows in C and D). Normal caliber non- opacified ureter is seen (Chevron in D).
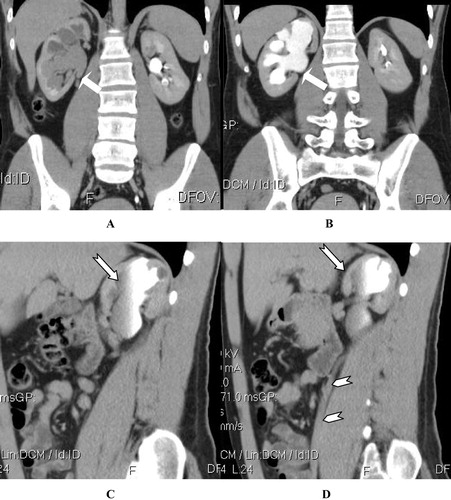
Fig. 5 CTU (A) Axial arterial phase (B) excretory phase showing left renal hydronephrosis on top of renal vessels impression over the left VUJ (Arrows) with urine contrast fluid level (chevron in B). (C and D) CMPR showing the left renal vessels (arrows) and the left gonadal vessels are seen impinging and encircling the left PUJ (Chevron).

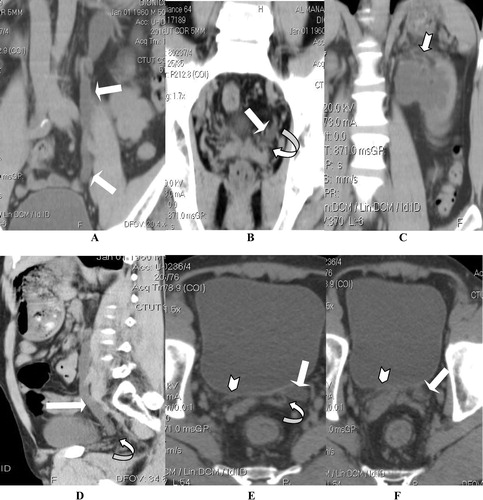
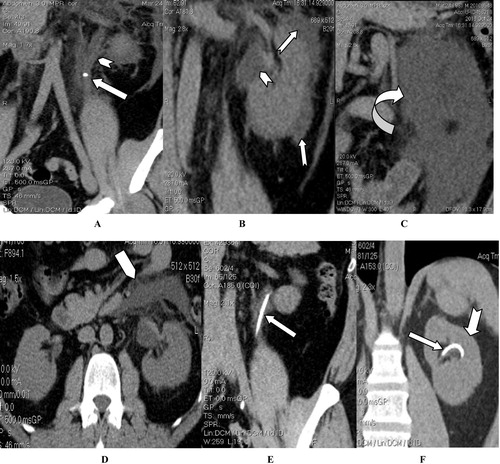
As well known, the most commonly encountered acquired ureteric disease is the ureteric calculus, which was seen in 103 patients of this study candidates (25.75%). Their usual clinical presenting symptoms were: acute renal colic or vague loin pain together with gross or microscopic hematuria. Also, few of them with right ureteric stones were presented with appendicitis like symptoms as right lower abdominal pain with nausea and vomiting. At the non-contrast phase of CTU, all types urinary tract calculi (of different chemical structures) usually give high attenuation densities; >200 HU. The ureteric calculi are commonly seen at the sites of physiological ureteral narrowing, which are the UPJ, pelvic brim, and VUJ (). The only exception of this density is the indinavir induced soft stones which are induced by such protease inhibitor anti HIV drug. So these softer stones may be missed in the non-contrast scans and seen only in the excretory phase as filling defects that got some other differential diagnosis excluded by clear clinical and pharmacological history intake.Citation20–Citation22
Fig. 6 Non contrast CTU (A) CMPR (B) axial images in another patient showing left distal ureteric hyperdense stones (Arrow in A) and left vesicoureteric junction (Arrow in B), which are the common sites for ureteric stones arrest.
These common hyperdense calculi are often obscured by the high attenuation of excreted contrast agent at the excretory phases of CT urography, especially if small and non-obstructive, as they will not be identified as filling defects. Non-enhanced CT is therefore the preferred modality for diagnosing ureteral calculi, and contrast administration is not generally indicated. In some cases, especially in ureteric stones passers, there may be associated calcular induced ureteritis with localized peri-calcular thickened edematous short ureteric segment, clearly seen in CTU as soft-tissue rim sign.Citation23 Spontaneous rupture of the urinary collecting system with urine extravasation in the perirenal space or in the retroperitoneal space is an uncommon complication of obstructive uropathy, seen in 2 patients (). It is usually associated with ureteral obstruction by calculi. As urine extravasates into the retroperitoneum, it can cause lipolysis of the surrounding fat with resultant encapsulation of urine, forming an encysted urine collection. Also, it may be seen as a complication to other varieties of obstructive or traumatic uropathy e.g. UPJ stricture, retroperitoneal fibrosis, retroperitoneal malignancy including renal pelvis or ureteric tumors, all causes of bladder outlet obstruction, iatrogenic (e.g. ESWL or ureteroscopy) or traumatic. US examinations and IVU without delayed films could simply miss the diagnosis of urinoma, while CTU or MRI is the diagnostic modality of choice.Citation24 Also CTU is a perfect imaging modality for monitoring the therapeutic response of these urinomas after the usual therapeutic intervention, which is double J ureteric catheter insertion ().
Fig. 7 (A) Non contrast CTU-CRF showing right PUJ stone with secondary back pressure and huge sized right paranephric minimally hyperdense collection (Arrow), which is clearly confirmed with MRI T2w axial images (B) to be collection of intermediate T2w signal (Arrow in B).
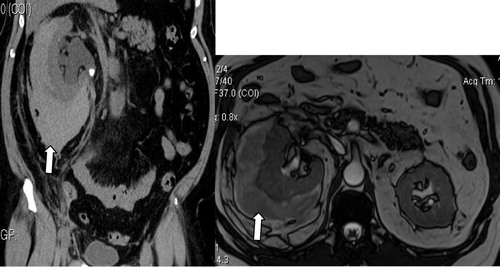
Fig. 8 Non contrast phase of CTU (A–C) CRF and (D) axial cuts showing left upper ureteric stone (Arrow) with 2ry left upper hydroureter and hydronephrosis (Chevron) with perinephric fluid collection (Notched arrows), anterior paranephric (Pentagon) and distal retroperitoneal urinoma (Curved arrow). (E&F) Post ureteric DJ catheter insertion (Arrow) and resolution of the perinephric collection (Notched arrow).
Pyogenic ureteric infection was diagnosed in 8 patients (2%), through identification of the typical CT radiological signs in conjunction with the clinical picture and laboratory results. The radiological CT signs of acute ureteritis include edematous ureteral wall mural thickening with postcontrast enhancement and periureteral fat planes stranding. Long standing uncontrolled ureteritis may end with long segmental ureteral stricture, as seen in one patient in this study, which frequently needs ureteroscopic proof of not being neoplastic strictureCitation25 (). Pyeloureteritis cystica, which is a chronic form of ureteritis, had been seen in only two old diabetic patients (0.5%) (). Ureteritis cystica usually develops secondary to chronic repeated urothelial irritation by frequent calcular passage with or without infectious diseases. Histologically, there will be multiple submucosal epithelial-lined cysts representing cystic Brunn cell nests, surrounded with lymphocytic infiltrates. Their CTU examinations (excretory phase) showed multiple uniform small cystic filling defects in the renal pelvis and the affected ureter (averaging few millimeters). However, similar or nearby presentation could be seen in more serious pathological conditions, like multifocal TCC or malakoplakia. Sometimes because of the small volume of the cysts, they can’t be reliably differentiated from small TCC soft tissue masses on CTU basis. Some radiological signs may support the diagnosis of pyeloureteritis cystica rather than TCC; such as being more numerous and tendency for upper ureteric affection, however ureteroscopic biopsy is still often needed.Citation26
Fig. 9 CTU non contrast axial (A), arterial phase (B), zoomed excretory phase (C) and CRF excretory phase (D) showing: left upper ureteric inflammatory process see as localized long segmental wall thickening (Arrow in A), with post contrast enhancement (Arrow in B), and paraureteric extensive fat planes stranding (Arrow in C) and long segmental athologically proven inflammatory stricture (Arrow in D).
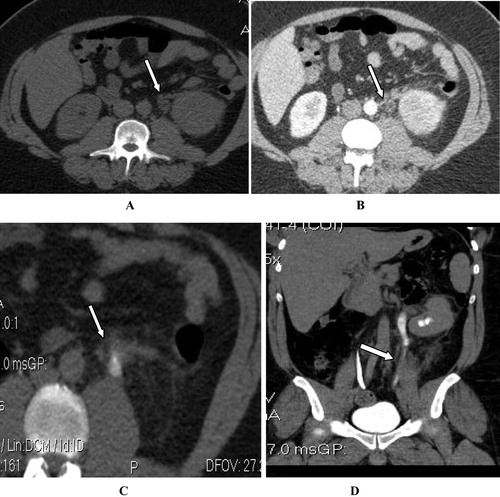
Fig. 10 Pyeloureteritis cystica: CTU excretory phase CRF (A and B) showing para-nephric fat planes stranding (Notched arrows), and multiple small cystic filling defects (Arrows).
Transitional cell carcinoma (TCC) was diagnosed by CTU in 3 cases of this study candidates (0.75%). TCC is a malignant tumor which arises from the urothelial cells lining the urinary tract from the renal calyces to the urinary bladder, including the ureters. Recently published epidemiological studies stated that upper urinary tract TCC (pelviureteric) is estimated to represent 5% of all urothelial cancers and in less than 10% of all renal tumors.Citation27 Evidences indicate that the frequency of upper urinary tract malignancies is increasing. The diagnosis of TCC in this study was based on the fact that it the commonest type of malignant ureteric tumors. TCC of the ureter could be radiologically seen at CTU excretory phase as intraluminal polypoidal filling defects or annular stricture at its early presentation (). Also, it is not uncommon to have simultaneous multifocal primary lesions at the time of presentation or later on at time intervals of months or even years i.e. synchronous or metachronus multiplicity. If missed for a while, as one of our patient, it could be presented with severe obstructive nephropathy secondary to a large ureteric expanding soft tissue ureteric mass lesion, which may infiltrate the adjacent structures. There is a described CTU sign named the goblet sign; which is highly suggestive (Not 100% pathognomonic) of ureteric TCC. This goblet sign is a cup like filling defect due to the soft tissue growth inside the ureter; however it is more conspicuous in retrograde not antegrade CT or conventional pyeloureterography.Citation28,Citation29
Fig. 11 CTU Excretory phase (A and B) CRF and (C) axial section corresponding to the locator site seen in B showing: two left ureteric small soft tissue filling defects (Arrows); relatively away from the PUJ, which supports the diagnosis of multifocal TCC rather than inflammatory processes.
The clinical and/or the laboratory presentation of painless hematuria are very important signs to consider pelviureteric and urinary bladder tumors, of which TCC is the most common. Still, there is a conflict in small ureteric lesions seen in CTU, as they may simulate ureteritis or malakoplakia. However, the distal ureteric location and the paucity of the lesions significantly favor the neoplastic etiology (). CTU diagnosis of urothelial tumors is much simpler in neglected cases, as seen in one patient of this study (), due to the looking of the aggressive expanding soft tissue swelling and extrinsic extension. CTU had been proven not only to be perfect imaging modality for detection and diagnosis of TCC but also in TNM staging of the tumor, which is crucial for management .
Fig. 12 CTU (A and B) Nephrogenic phase showing: large expanding slightly enhancing distal right ureteric sizable tubular soft tissue mass lesion causing severe tortious proximal right hydroureter and hydronephrosis with punctate calcification and extrinsic extension (Arrows). Suspected another smaller proximal lesion is seen, as well (Chevron in B).
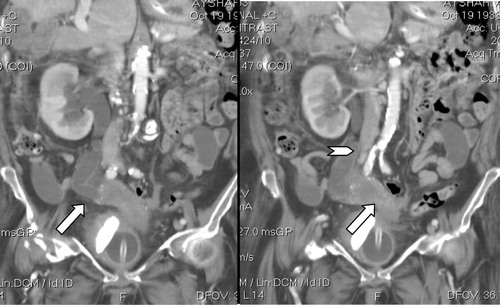
Table 2 TNM staging of ureteric TCC.
Primary retroperitoneal fibrosis (PRPF) was diagnosed in only one patient (0.025%), during the whole study (). It is a rare disease with an estimated incidence of 1.38/100,000 people. Some medications, abdominal aortic aneurysm, infections, malignancies, trauma, surgery, and radiation therapy have been accused to be causative pathology of RPF; however, it is commonly idiopathic. PRPF commonly occurs in individuals 40–60 years of age; with a male to female ratio of 3.3:1.Citation30,Citation31 It had been previously described as chronic periaortitis, as the pathological process is centered around the abdominal aorta. Histologically; it is a fibrotic reaction within the retroperitoneal tissues that encases the retroperitoneal structure causing bilateral medial ureteral traction and constriction. IVP can show the secondary effect of PRPF, which is bilateral medial ureteric deviation and obstructive uropathy. However, CTU will be more informative imaging tool, as it can clearly show the extent of the paraortic retroperitoneal fibrotic bands with its traction obstructive effect on the ureters. Also, it helps to show if there is a causative abdominal etiology like abdominal aortic aneurysm or retroperitoneal malignancy which are the common causes of secondary RPF.Citation32
Fig. 13 A 58 years male with PRPF; (A) MIP & (B) VR CRF CTU excretory phase showing asymmetrical medially deviated and kinked right ureter with secondary right sided minimal obstructive uropathy. (Arrows) (C–E) CTU arterial phase axial cuts showing entrapment of the aortic bifurcation and right common iliac vessels by retroperitoneal prevertebral irregular fibrous soft tissue swelling. The right ureter is significantly deviated medially and partially entrapped by the mass (notched arrows), in comparison with the normal posed left ureter, which is seen in front of the left psoas muscle (Chevrons).
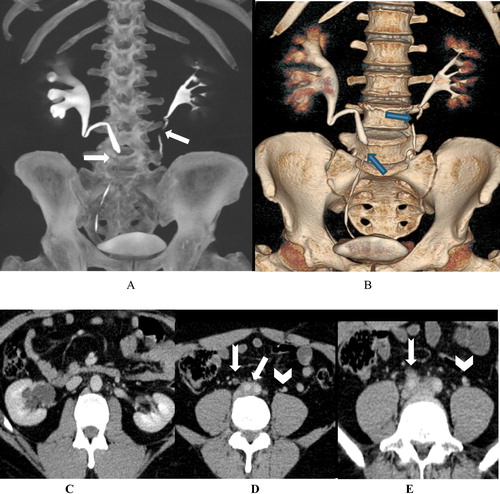
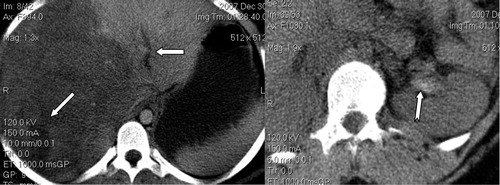
Ureteric trauma is a relatively uncommon but it may result in serious complications, due to the usual delayed diagnosis. The classic clinical presentation is post-traumatic loin or flank pain with hematuria. However these symptoms and signs may also be completely absent in up to 25% of patients, who may be lately presented with acute renal failure or severe acute abdomen. The detection of ureteric injuries is delayed for days or even weeks in about 60% of patients. There is a wide range of ureteric injuries; ranging from mucosal injury, ligation, partial or complete ureteric transection up to complete ureteric avulsion.Citation33,Citation34 18 RTA traumatized patients with post traumatic hematuria, were included in this study. CTU had diagnosed pelviureteric avulsion in only one patient, associated with displaced fracture of the lumbar spine and lower polar left renal laceration (). The other 17 patients’ CTU results were either normal or kidneys or bladder injuries. Hematuric blood clots could be seen in the non-contrast phase as hyperdense intraureteric fluid (>50 HU) (). Typically it appears as a vermiform like filling defect in the excretory phase. Also, the clot does not enhance in the contrast phases and changes position or completely resolves at follow-up imaging studies. However, in non-traumatized patients with hematuria; a small clot may be difficult to be distinguished from TCC at initial CTU, which may need ureteroscopy or short-interval follow-up imaging for confirmation.Citation35,Citation36
Fig. 14 CTU after severe RTA injury (A and B) CRF and (C) axial section showing fractured dislocation of the mid-lumbar spine (Notched arrow), lower left renal contusion (Arrow in A) with distorted pelviureteric junction (Arrow in B) and retroperitoneal extravasated contrast in the delayed scans (Arrow in C).
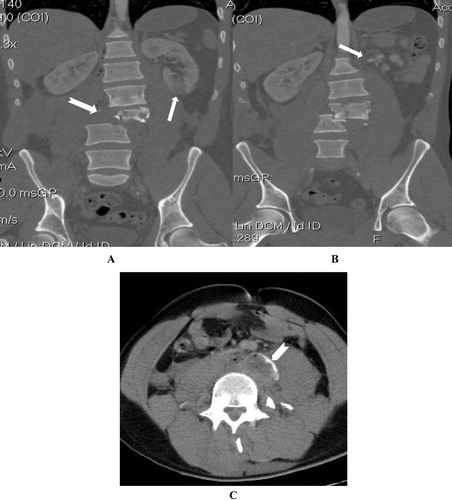
Fig. 15 Post RTA abdominal injury CTU non contrast axial sections show (A) Liver lacerations (Arrows) and (B) left renal pelvis hyperdense hematoma (Notched arrow).
Ureteric injuries are more commonly iatrogenic; most commonly during gynaecological procedures. Penetrating or blunt ureteric injuries are relatively uncommon; representing <1% of all urological trauma. Anatomically, ureteric injury could be classified into pelviureteric - upper third ureter (mostly due to blunt abdominal trauma and RTA), middle and distal thirds ureteric trauma, which is often following iatrogenic injury. CTU with intravenous contrast is the examination of choice for evaluation of ureteric trauma, as it clearly demonstrates the site and the extent of the injury. Also, it can accurately verify its type; whether avulsion or trans-section or ligation. In addition to its role in detection of associated other abdominal organ injuries and the resultant complications e.g. retroperitoneal hematoma, hydronephrosis, strictures and the resultant obstructive nephropathy ending if neglected into renal failure. Early diagnosis and appropriate correction of the cause- if possible- (e.g. removal of suture on tied ureter or reconstruction of induced ureteric strictures) will result in satisfactory outcome. Temporary ureteric stents or even percutaneous nephrostomy may be needed until full ureteric repair is done.Citation37
Despite the sensitivity of IVP in ureteric imaging, it has limitations of being in need for good renal excretory poor, lack of extra-ureteric adjacent structures evaluation and wide differential diagnosis of filling defects. Based upon the results of this study we recommend the use of CTU as a one-stop shop imaging technique for patients with suspected ureteric pathology, thereby saving time and hospital visits and leading to earlier diagnosis. This result is accepted at the expanse of the high dose radiation exposure, which may be not suitable for some patients, like pregnant females. However, the American Urological Association guidelines still equally recommend IV or CT urography as the initial imaging test for patients with asymptomatic microscopic hematuria.Citation3 In contrast to, the recent guidelines from the European Society of Urogenital Radiology which had supported the use of CTU. Contraindications to CTU are generally limited to those patients who cannot receive iodinated contrast because of renal insufficiency, prior severe reaction, or pregnancy.Citation38
6 Conclusion
CTU could be trusty used as a very sensitive diagnostic one-stop shop imaging tool in patients with clinically suspected ureteric lesions.
7 Limitations of the study
Pregnant females may suffer from different ureteric complaints; commonly colic due to ureteric stones or ureteric compression by the pregnant uterus. Considering the fact that, ionizing radiation has a carcinogenic and teratogenic hazards to the developing fetus, there is a considerable limitations to use CTU, especially in the first trimester. US and KUB are recommended as first imaging modalities; however sometimes CTU is mandatory e.g. RTA with suspected ureteric trauma.Citation39
Also, there are some considerations for radiation exposure in children, as children are considerably more sensitive to radiation than adults. Children have a longer life expectancy than adults, resulting in a larger window of opportunity for expressing radiation damage. Children commonly receive a higher radiation dose than necessary if CT settings are not adjusted for their smaller body size. All These facts encourage keeping CTU examinations as last resort in children after trials to obtain the diagnosis by other less hazardous tools. Also, we recommend the use of low kV and dual phase techniques if CTU is going to be done in children, in attempt to minimize the radiation dose exposure.Citation40
Also, due to the large group of ureteric pathologies as well as coast-effective facts in the private hospitals, there was limitation for comparison of our study CT results with other imaging modalities; as MRU.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 27 July 2017
References
- M.MasaraniM.DinneenUreteric colic: new trends in diagnosis and treatmentPostgrad Med J83200746947210.1136/pgmj.2006.055913
- C.M.LyeL.FasanoA.S.WoolfUreter myogenesis: putting Teashirt into contextJ Am Soc Nephrol2120102430
- S.G.SilvermanJ.R.LeyendeckerE.S.AmisWhat is the current role of CT urography and MR urography in the evaluation of the urinary tract?Radiology2502009309323
- R.D.NawfelP.F.JudyA.R.SchleipmanPatient radiation dose at CT urography and conventional urographyRadiology2322004126132
- S.A.JoffeS.ServaesS.OkonMulti-detector row CT urography in the evaluation of hematuriaRadiographics23200314411456
- P.DahlmanA.J.van der MolenM.MagnussonA.MagnussonHow much dose can be saved in three-phase CT urography? A combination of normal-dose corticomedullary phase with low-dose unenhanced and excretory phasesAJR Am J Roentgenol1992012852860
- R.K.KazaJ.F.PlattR.H.CohanE.M.CaoiliM.M.Al-HawaryA.WasnikDual-energy CT with single- and dual-source scanners: current applications in evaluating the genitourinary tractRadioGraphics322012353369
- P.J.KenneyCT evaluation of urinary lithiasisRadiol Clin N Am412003979999
- Sourtzis S, Thibeau JF, Damry N, et al. Radiologic investigation of renal colic: unenhanced helical CT compared with excretory urography. Am J Roentgentol 1999;172:1491–4.
- M.MahmoudAhmedMoawadMohamed S.El-ZawawyThe role of multidetector computed tomography urography in the evaluation of obstructive uropathyKorean J Radiol52004110
- Fernbach SK1, Feinstein KA, Spencer K, Lindstrom CA. Ureteral duplication and its complications. Radiographics 1997;17:109–27.
- Gatti JM, Cendron M. Ureteral duplication, ureteral ectopia, and ureterocele. http://emedicine.medscape.com/article/1017202-overview (Updated: Oct 09, 2015).
- B.AdiegoP.Martinez-TenJ.Perez-PedregosaAntenatally diagnosed renal duplex anomalies: sonographic features and long-term postnatal outcomeJ Ultrasound Med302011809815
- H.WilliamsRenal revision: from lobulation to duplication—what is normal?Arch Dis Child Educ Pract Ed922007152158
- T.BerrocalP.Lopez-PereiraA.ArjonillaJ.GutierrezAnomalies of the distal ureter, bladder, and urethra in children: embryologic, radiologic, and pathologic featuresRadioGraphics222002 1139–116
- J.KleinJ.GonzalezM.MiraveteCongenital ureteropelvic junction obstruction: human disease and animal modelsInt J Exp Pathol922011168192
- L.P.LawlerT.W.JarretF.M.CorlE.K.FishmanAdult ureteropelvic junction obstruction: insights with three dimensional multi-detector row CTRadioGraphics252005121134
- J.S.LamA.BredaP.G.SchulamUreteropelvic junction obstructionJ Urol177200716521658
- J.D.TsaiF.Y.HuangC.C.LinIntermittent hydronephrosis secondary to ureteropelvic junction obstruction: clinical and imaging featuresPediatrics1172006139146
- E.P.TammP.M.SilvermanW.P.ShumanEvaluation of the patient with flank pain and possible ureteral calculusRadiology228200331932910.1148/radiol.2282011726
- B.R.MatlagaO.D.ShahD.G.AssimosDrug induced calculiRev Urol52003227231
- J.P.HeneghanK.A.McGuireR.A.LederHelical CT for nephrolithiasis and ureterolithiasis: comparison of conventional and reduced radiation-dose techniquesRadiology229200357558010.1148/radiol.2292021261
- Dyer RB, Chen MY, Zagoria RJ. Classic signs in uroradiology. Radiographics 2004;24 Suppl 1 (suppl 1): S247–80. Radiographics (full text). http://doi:10.1148/rg.24si045509 – Pubmed citation.
- C.SebastiàS.QuirogaR.BoyéC.CantarellM.Fernandez-PlanasA.AlvarezHelical CT in renal transplantation: normal findings and early and late complicationsRadioGraphics21200111031117
- A.P.WasnikK.M.ElsayesR.K.KazaMultimodality imaging in ureteric and periureteric pathologic abnormalitiesAJR Am J Roentgenol197201110.2214/AJR.11.6623
- Kawashima A, Vrtiska TJ, Leroy AJ et-al. CT urography. Radiographics. 2004;24 Suppl 1 (suppl 1): S35–54.
- R.L.SiegelK.D.MillerA.JemalCancer statisticsCA Cancer J Clin662016730
- R.VikramC.M.SandlerC.S.NgImaging and staging of transitional cell carcinoma: part 2, upper urinary tractAJR Am J Roentgenol192200914881493
- R.F.BrowneC.P.MeehanJ.ColvilleTransitional cell carcinoma of the upper urinary tract: spectrum of imaging findingsRadiographics25200516091627
- A.VaglioC.SalvaraniC.BuzioRetroperitoneal fibrosisLancet3672006241251
- E.F.Van BommelI.JansenT.R.HendrikszA.L.AarnoudseIdiopathic retroperitoneal fibrosis: prospective evaluation of incidence and clinicoradiologic presentationMedicine (Baltimore)882009193201
- C.G.CroninD.G.LohanM.A.BlakeRetroperitoneal fibrosis: a review of clinical features and imaging findingsAJR Am J Roentgenol1912008423431
- B.PereiraM.OgilvieJ.Gomez-RodriguezA review of ureteral injuries after external traumaScand J Trauma Resusc Emerg Med1820106
- R.N.SrinivasaS.A.AkbarS.Z.JafriG.A.HowellsGenitourinary trauma: a pictorial essayEmerg Radiol1620092133
- A.ShinagareC.SadowSahniStuart G.SilvermanUrinary bladder: normal appearance and mimics of malignancy at CT urographyCancer Imaging112011100108
- P.L.ChoykeRadiologic evaluation of hematuria: guidelines from the American College of Radiology's appropriateness criteriaAm Fam Phys782008347352
- P.RamchandaniP.M.BucklerImaging of genitourinary traumaAJR Am J Roentgenol192200915141523
- A.J.Van der MolenN.C.CowanU.G.Mueller-LisseC.C.Nolte-EmstingS.TakahashiR.H.CohanCT urography: definition, indications and techniques-a guideline for clinical practiceEurRadiol182008417
- C.SadroT.DubinskyCT in pregnancy: risks and benefitsAppl Radiol422013616
- M.E.ArchD.P.FrushPediatric body MDCT: a 5-year follow-up survey of scanning parameters used by pediatric radiologistsAJR1912008611617
