Abstract
Background
Practice variation is likely to have an important impact on the effectiveness of endoscopy. Performing regular quality audits allows identification of potential underperformance and consequently can result in significant improvement in endoscopy quality. An annual audit was conducted in a community hospital in Egypt.
Aim
The aim of the study was to determine if practice and performance of endoscopy is influenced by a consistent audit process by looking for improvement in completeness of procedures over a 10-year period.
Patients and methods
A total of 3736 consecutive procedures were prospectively assessed between years 2004 and 2014.
Results
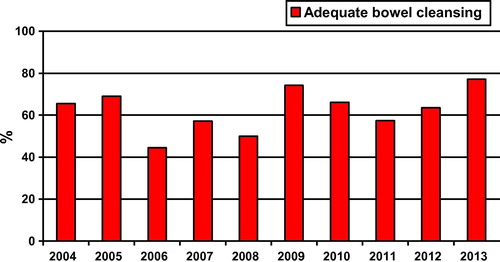
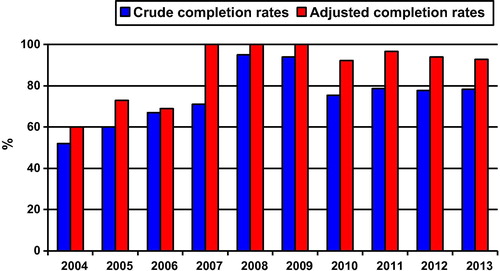
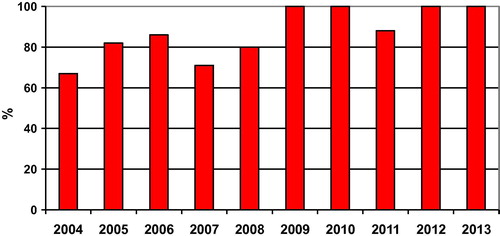
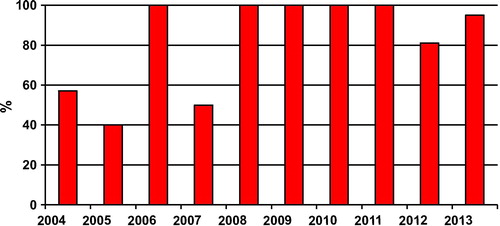
The completion rates improved consistently. Esophagogastroduodenoscopy (EGD) completion rate was 99.9% in 2004–2008 and 99% in 2009–2013 (P = 0.5). Initial hemostasis of EGD-gastrointestinal bleed increased from 82% in 2004–2008 to 86% in 2009–2013 (P = 0.04). Adequate bowel cleansing increased from 60% in 2004–2008 to 67% in 2009–2013 (P = 0.13). Crude completion rates increased from 66% in 2004–2008 to 79% in 2009–2013 (P = 0.007). Adjusted completion rates increased from 80% in 2004–2008 to 95% in 2009–2013 (P = 0.0001). Ileoscopy rates in patients with chronic diarrhea increased from 79% in 2004–2008 to 97% in 2009–2013 (P = 0.01). Endoscopic polypectomy rates increased from 65% in 2004–2008 to 94% in 2009–2013 (P = 0.0004). Complete polyp removal rates increased from 77% in 2004–2008 to 87% in 2009–2013 (P = 0.19). Complete polyp retrieval rates increased from 85% in 2004–2008 to 89% in 2009–2013 (P = 0.34).
Conclusion
Continuous audit over 10 years can enhance endoscopy performance, improve the quality of endoscopic procedures and lead to better outcomes.
1 Introduction
Over the last four decades, gastrointestinal endoscopy has become of paramount importance to diagnose, treat, and prevent diseases of the digestive tract. Over past decade there has been an increasing interest in quality issues in endoscopy in order to ensure that high-quality endoscopic procedures are performed in all cases. Practice variation however is likely to have an important impact on the effectiveness of endoscopy and can impair the delivery of high-quality endoscopic procedures. The American Society of Gastrointestinal Endoscopy (ASGE) and the British Society of Gastroenterology (BSG) have each published quality indicators in endoscopy that were updated in 2015.Citation1–Citation4 Selected performance targets were recommended for each quality indicator to serve as specific goals for measuring quality improvement.Citation1–Citation4 The European Society of Gastrointestinal Endoscopy (ESGE) has published a short list of key performance measures for lower gastrointestinal endoscopy in 2017.Citation5 ESGE recommended that endoscopy services across Europe adopt key performance measures for lower gastrointestinal endoscopy for measurement and evaluation in daily practice at a center and endoscopist level.Citation5
Having a guideline does not result in improved health outcomes per se; in order to improve quality, it is essential to implement guidance and measure performance. Performing regular quality audits allows identification of potential underperformance, which provides an opportunity for discussion and support for the endoscopist.Citation6 It is recommended that all units develop mechanisms for audit and feedback of endoscopists’ performance using quality markers. In addition, standards should be set with clear strategies on how to manage the performance of those who fall below the agreed standards, such as further training and mentoring.Citation6 There is clear evidence that implementing the above measures, along with additional measures such as structured training programs, can result in significant improvement in endoscopy quality. For example, in the United Kingdom, following a decade of quality improvement initiatives, cecal intubation rate improved nationally from 76.9% to 92.3%.Citation7 However despite the dramatic overall improvement, there was still unacceptable variation in quality, and more work is required.Citation7
Endoscopy units need to be sure that they are delivering high quality endoscopy at levels consistent with recognized standards.Citation8 It is therefore important to determine if endoscopists are achieving these standards by measuring key performance indicators.Citation8 The audit process is one tool for evaluating performance and producing local service improvement. Providing feedback to endoscopists on various parameters of endoscopy may serve to enhance performance. However, audit is often collected in an ad hoc manner and may not be consistent over a long period.Citation7 There is limited data on trends for key performance indicators and it remains uncertain whether the audit process enhances quality over time.Citation7
Completeness of procedure is one of the quality domains used as a performance measure of endoscopy.Citation5 Completeness of procedure has been found to be highly variable between endoscopists especially in colonoscopy.Citation6 There is evidence in the medical literature to support a disparity in colonoscopy performance with respect to cecal intubation rates.Citation9 Cecal intubation is one of the main goals of colonoscopy; however, complete colonoscopy rates vary considerably.Citation10 Incomplete colonoscopies pose a clinical concern because management strategies to assess patients with incomplete colonoscopies vary.Citation10
Bolak Eldakror Hospital is a secondary-care governmental hospital in Giza, Egypt. Esophagogastroduodenoscopy (EGD) and colonoscopy are performed. An endoscopy quality-assurance program was instituted in 2003 when quality indicators developed by the ASGE and BSG were implemented.Citation11 Initially it involved setting standards of practice and designing an approved training program. An annual audit was conducted to monitor performance. The aim of the study was to determine if practice and performance of endoscopy is influenced by a consistent audit process by looking for improvement in completeness of procedures over a 10-year period.
2 Patients and methods
The study was performed in Bolak Eldakror hospital which is a secondary-care governmental hospital in Giza, Egypt. The endoscopy unit is staffed with three endoscopists, one secretary and four nurses.
Completeness of endoscopic procedures was evaluated over a 10 year-period between January 2004 and January 2014. Completeness of procedure was measured through assessment of technical and therapeutic outcomes of endoscopy.Citation12 Technical aspects of the procedure include completion of the examination and therapeutic maneuvers.Citation1 Criteria of completion were identified. EGD was defined as complete if gastric retroflexion and visualization of the second part of the duodenum were performed. Patients with esophageal stenosis, gastric obstruction or incomplete examination due presence of blood were excluded. The agreed standard for EGD completion rate is ≥95% of all cases.Citation1,Citation3 Hemostasis of EGD bleeding was attempted at the time of initial endoscopy. Once an intervention has been undertaken, the procedure was considered successful if bleeding stopped and there was no recurrent bleeding within five days of intervention. In many prospective series that have evaluated different modalities for managing actively bleeding upper gastrointestinal lesions, immediate hemostasis rates from 90% to 100% have been achieved.Citation1,Citation3 At present, there are no currently accepted standards of hemostasis attainment in community practice from which to assign an evidenced-based performance target.Citation1,Citation3 All patients undergoing colonoscopy were prescribed a standard bowel preparation consisting of a low residue diet for 48 h, with clear fluids only for the last 24 h, and a purgative (caster oil) to be taken for the last 12 h before the procedure. An enema was given twice at night and immediately before the procedure. The quality of bowel preparation was graded as excellent (completely clear), good (clear liquid aspirable stool), fair (semisolid debris, adhering to the colonic mucosa and not allowing adequate vision of the whole mucosa), or poor (solid stool, not allowing adequate progression of the endoscope and leading to subsequent termination of the procedure).Citation1 The quality of bowel preparation was graded as: ‘excellent’ or ‘good’ for adequate bowel preparation, and ‘fair’ or ‘poor’ for inadequate bowel preparation.Citation13 The agreed standard for adequate bowel preparation is ≥85% in the United States and ≥90% in Europe and United Kingdom.Citation1–Citation5 Colonoscopy was defined as complete if the cecum was reached. Adjusted completion rate was calculated by excluding factors beyond the endoscopists‘ control and cecal intubation based on reliable landmarks only. The agreed standard for colonoscopy completion rate is ≥90% overall.Citation1–Citation5 Ileal intubation was systematically attempted in all patients with chronic diarrhea. Patients with bloody diarrhea and non-bloody diarrhea were included. Procedures with unavoidable and avoidable failures to reach cecum were excluded. The agreed standard for ileal intubation in patients with chronic diarrhea is ≥70%.Citation14 Polypectomy was routinely performed for all polyps identified with a retrieval of all removed polyps for histological analysis. The agreed standard for complete polypectomy of pedunculated polyps and sessile polyps less than 2 cm is ≥80% and for polyp recovery ≥90%.Citation1–Citation5
The first audit conducted on the completeness of endoscopic procedures was performed in 2003 and was retrospective. EGD completion rate was 86% but endoscopic therapy in patients with EGD-gastrointestinal bleed was not documented. The quality of colon preparation was not documented either. The crude completion rate was 50% and the adjusted completion rate were not documented nor the ileal intubation in patients with chronic diarrhea. Polypectomy was performed in 50% of patients with detected polyps but the completeness of removal and retrieval of the polyps were not recorded. The audit generally showed a lack of documentation of procedures completion and suboptimal performance in those that were documented.
In view of these deficiencies, a second prospective audit was designed. Procedure completion was monitored and documentation was regularly checked. A database was created for all procedures performed. A standardized data collection form (sheet) was completed after the procedure by each operator. Recorded information for each procedure included completion of procedure, criteria of completion, main reasons for incompletion and future management plan. Data were entered by the secretary. Microsoft Excel was used for storage and analysis of the data. Recorded data included EGD completion, identification of the bleeding lesion, description of bleeding stigmata, method of endoscopic hemostasis if any, success of endoscopic therapy, adequacy of bowel preparation, colonoscopy completion, ileal intubation in patients with chronic diarrhea, polypectomy in patients with detected polyps, completeness of removal and retrieval of resected polyps. Data was collected and evaluated. An annual audit was conducted to monitor performance. The results of the audits were presented to the team for information, analysis and identification of observed deviations. Corrective measures were implemented for any deviation from standards or suboptimal performance. Poor performance endoscopists were retrained or attended training courses. A total of 3736 consecutive procedures were prospectively assessed over a 10 year-period between January 2004 and January 2014.
Statistical Analysis: Data entry, tabulation and figure presentation were done using Microsoft Excel sheet. Descriptive data presented as percentages and was performed to detect the differences between two categorical groups. Analyses were done using Microstate statistical program, t proportion (tp) and Z scoring was used to estimate differences between percentage values, P value was considered significant if it is <0.05.
3 Results
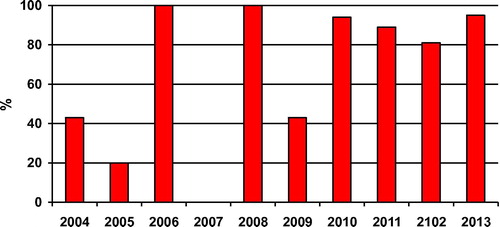
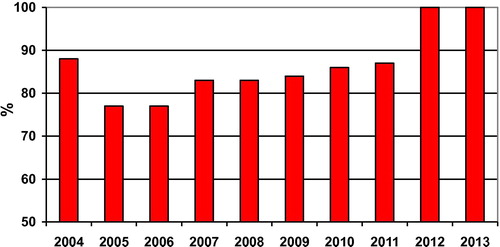
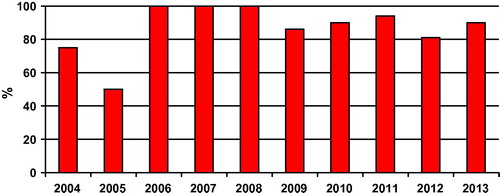
Audit data of completeness of 3282 EGD performed between 2004 and 2014 was assessed (). EGD completion rates ranged from 98.86% to 100%. EGD completion rate was 99.9% in years 2004–2008 and 99% in years 2009–2013 with no statistical significant difference (P = 0.5) (). One thousand one hundred and forty-three patients with acute upper gastrointestinal bleeding received endoscopic therapy at the time of initial endoscopy (). One thousand one hundred and thirty-three patients (99%) had endoscopically diagnosed bleeding varices and 10 (1%) had peptic ulcer and a visible vessel or active bleeding. Initial hemostasis following endoscopic therapy increased significantly (P = 0.04) from 82% in years 2004–2008 to 86% in years 2009–2013 (). Audit data of completeness of 454 colonoscopies performed between 2004 and 2014 was assessed (). Adequate bowel cleansing increased from 60% in years 2004–2008 to 67% in years 2009–2013 with no statistical significant difference (P = 0.13) (). Crude completion rates increased significantly (P = 0.007) from 66% in years 2004–2008 to 79% in years 2009–2013 (). Adjusted completion rates increased significantly (P = 0.0001) from 80% in years 2004–2008 to 95% in years 2009–2013 (). Seventy-two patients had chronic diarrhea (). Ileoscopy rates in patients with chronic diarrhea increased significantly (P = 0.01) from 79% in years 2004–2008 to 97% in years 2009–2013 (). Polyps were detected in one hundred and eighteen patients during colonoscopy (). Detected polyps were pedunculated or sessile and were <2 cm. Endoscopic polypectomy rates in patients with detected polyps increased significantly (P = 0.0004) from 65% in years 2004–2008 to 94% in years 2009–2013 (). Percentage of procedures in which polyps were judged completely removed increased from 77% in years 2004–2008 to 87% in years 2009–2013 with no statistical significant difference (P = 0.19) (). Polyp retrieval of ≥90% of all removed polyps increased from 85% in years 2004–2008 to 89% in years 2009–2013 with no statistical significant difference (P = 0.34) ().
Table 1 The EGD volume per year.
Table 2 The EGD completion rates among studied years.
Table 3 The initial hemostasis rates following endoscopic therapy of EGD-gastrointestinal bleed among studied years.
Table 4 The colonoscopy volume per year.
Table 5 The quality of bowel preparation among studied years.
Table 6 The crude completion rates among studied years.
Table 7 The adjusted completion rates among studied years.
Table 8 The ileoscopy rates in patients with chronic diarrhea among studied years.
Table 9 The Endoscopic polypectomy rates in patients with detected polyps among studied years.
Table 10 The complete polyp removal rates among studied years.
Table 11 The polyp retrieval rates among studied years.
The initial hemostasis rates after endoscopic therapy, quality of bowel preparation, crude completion rates, adjusted completion rates, ileoscopy rates in patients with chronic diarrhea, polypectomy rates, complete polyp removal rates and complete polyp retrieval rates among years studied are shown in –.
4 Discussion
Prospective audit is a standard technique that provides a snapshot of performance.Citation15 The audit process can drive performance improvement. The simple act of monitoring a service will improve performance (the Hawthorne Effect).Citation6 Once standards have been achieved it is necessary to continue to audit. Audits are intended to improve standards and make practitioners aware of need for continual improvement.Citation15 Regular feedback is also an important aspect of improvement because providing feedback to practitioners serves to enhance performance.Citation8
An annual audit was conducted in a community hospital in Egypt Completeness of procedures was continuously monitored with regular feedback to endoscopists. The aim of the study is to determine if practice and performance of endoscopy was influenced by a consistent audit process by looking for improvement in completeness of procedures over a 10-year period.
High EGD completion rates were achieved over the audit period 99.9% in 2004–2008 and 99% in 2009–2013. Davies et al. reported an EGD completion rate of 94.7%.Citation16 A protocol for management of upper gastrointestinal bleeding was designed to be within the available resources of the hospital and all patients presenting with acute upper gastrointestinal bleeding have been assessed and managed by this since 2004.Citation17,Citation18 The effectiveness of endoscopic therapy was monitored. Permanent hemostasis at the first endoscopic intervention increased significantly from 82% in 2004–2008 to 86% in 2009–2013. Zaltman et al. reported permanent hemostasis in 86% of patients with upper gastrointestinal bleeding at the first endoscopic intervention.Citation19 Variceal bleeding occurred in 20.45% of patients in the study by Zaltman et al. but in 99% of our patients, a result of the high rate of underlying liver disease in our community. Variceal bleeding is associated with significant morbidity and mortality.Citation20 Although overall survival has improved over the past 40 years, mortality is still closely related to failure to control bleeding or early re-bleeding.Citation20 Current endoscopic therapies are able to stop bleeding in nearly 90% of patients with acute variceal bleeding.Citation21,Citation22 Bambha et al. and Fallatah et al. reported successful hemostasis in 84% and 90% in patients with variceal bleeding respectively.Citation23,Citation24 Our EGD completion rates met the accepted standards.
Poor quality colonoscopy is associated with increased interval cancer rates.Citation25 Interval and missed colorectal cancers result from a variety of causes that include incomplete bowel cleaning and incomplete colonoscopy.Citation26 In our hospital caster oil and repeated enemas were used for purgation because polyethylene glycol electrolyte solution and phosphate solutions were not available. Adequate bowel cleansing was only 60% in 2004–2008. Poor preparation was, we felt, due to the type of preparation used, lack of compliance with instructions, and non-cooperation. We tried to improve the quality of bowel preparation by adding magnesium citrate (12 sachets twice daily on the previous day of the procedure), more time was spent with the patient to explain the importance of taking the preparation and following instructions in order to improve bowel preparation. Frail patients were admitted to the ward for bowel preparation. These measures were unsuccessful. Adequate bowel cleansing increased to only 67% in years 2009–2013 with no statistical significant difference. The quality of preparation would be improved by the use of modern proprietary formulations using polyethylene glycol with split dosing. Polyethylene glycol preparations became available in the hospital in 2014. The reported rate of inadequate bowel preparations ranges from 5% to 60%, with most studies citing around 25%.Citation27–Citation29 Inadequate bowel preparation was the most common reason for incomplete colonoscopy, accounting for nearly 25% of failed colonoscopies, in a 5-year complete audit of colonoscopy practice in a teaching hospital in the United Kingdom.Citation30 Never the less, crude colonoscopy completion rates did increase significantly from 66% in 2004–2008 to 79% in 2009–2013 and adjusted completion rates from 80% in 2004–2008 to 95% in 2009–2013. Published colonoscopy-completion rates vary substantially ranging from 76% to 99%.Citation31 Lower colonoscopy completion rates of 54% and 57% have been also reported.Citation31,Citation32 The value of audit as a tool for improving colonoscopy completion rates was demonstrated in a study by Bassi et al. where the completion rate improved from 75% to 89% in a colonoscopy audit in a large teaching hospital.Citation33 Routine ileoscopy is important in patients with chronic diarrhea and one of the major indications for terminal ileum intubation is to identify Crohn’s disease.Citation14 Terminal ileum intubation led to a positive diagnosis in 18% of patients with chronic diarrhea and increased to 36% in patients in whom a diagnosis of inflammatory bowel disease was suspected.Citation14 In our study ileoscopy rates in patients with chronic diarrhea increased significantly from 79% in 2004–2008 to 97% in 2009–2013. Terminal ileum intubation rates are variable with significant practice variation in the United States where an analysis of national endoscopic database showed it to be 28% in patients with chronic diarrhea.Citation34 Higher terminal ileum intubation was reported in other papers, 53.7% of patients with chronic non-bloody diarrhea and 79% to 95.5%.Citation35,Citation36 Successful polypectomy is crucial in colonoscopy, because incomplete resection is associated with the risk of interval colon cancer.Citation37 Incomplete polypectomy is considered the cause for up to 25% of interval colon cancers.Citation5 Polypectomy rates in our study increased from 65% in 2004–2008 to 94% in 2009–2013. Complete polyp removal rates also increased from 77% to 87% and polyp retrieval from 85% to 89% but with no statistical significant difference in either. Incomplete resection of polyps 5–20 mm in size, varies between 6.5% and 22.7% among endoscopists.Citation5 Fewer than 5% of resected polyps were not recovered in the United States and fewer than 10% in the United Kingdom.Citation7,Citation38 A nationwide colonoscopy audit in the United Kingdom in 2011 showed that 92.3% of resected polyps were retrieved.Citation7 Apart from bowel cleansing and crude completion rates, our colonoscopy completion rates met accepted standards. Improved crude completion rates could be achieved if we can correct reversible reasons for incomplete colonoscopy, mainly poor bowel cleansing.
There were important changes in practice and performance over the 10-year time period in our unit, completion rates improved consistently over the audit period so that high completion rates were achieved compared to published results. However, further improvements are possible if we can ensure optimal bowel preparation (≥85% target) and improve the crude completion rate (≥90% target).
Monitoring and regular feedback led to an increase in completion of endoscopies. The regular feedback to the endoscopists was an important aspect of the improvement, collecting, sharing and displaying data to the endoscopy team encouraged them to modify their performance in response to their awareness of being observed, they worked together towards a common goal and shared in their success. The improvement in performance may be a result of the audit process but other factors including general learning effects and the results of training, attendance at workshops and courses cannot be excluded.
This is the first study to date performed in a community hospital in Egypt. The gastroenterologists of the unit are representative of the ‘average gastroenterology specialist’ and may be representative of gastroenterologists across the nation. Our study findings provide evidence that quality monitoring in endoscopy can be applied in routine practice and they confirm the value of audit as a tool for improving endoscopy performance through improving completion rates. Continuous audit over 10 years can enhance endoscopy performance, improve the quality of endoscopic procedures and lead to better outcomes.
There are several limitations to this study that deserve mention. First, this is a single center study using self-reported endoscopy completion rates. Secondly, the data was obtained from an audit process rather than from a research project. Thirdly, recording and collecting data was time consuming and data recorded needed to be achievable within standard working practice.
Endoscopy has become enormously popular throughout the world because of its proven value in the diagnosis and treatment of digestive diseases. One problem is that the benefits are maximized only when procedures are performed at an optimal level of quality, which is not always the case.Citation39 Quality evaluation in the health care system is at present optional; but sooner or later it will become mandatory. Practice audit permits the evaluation of clinical practice to facilitate improvements in clinical care.Citation40
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Ethical approval: Not needed.
Patient consent: Not needed.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 12 September 2017
References
- D.J.BjorkmanJ.W.PoppMeasuring the quality of endoscopyGastrointest Endosc63Suppl2006S1S2
- Valori R. Quality and safety indicators for endoscopy; 2007. Internet. Available from: http://www.bsg.org.uk/attachments/170_bsg_grs_indic07.pdf.
- M.K.RizkM.S.SawhneyJ.CohenQuality indicators for all GI endoscopic proceduresGastrointest Endosc812015316
- Rees CJ, Gibson ST, Rutter MD, Baragwanath P, Pullan R, Feeney M et al. UK Key performance indicators and quality assurance standards for colonoscopy; 2013. Internet. Available from: http://www.bsg.org.uk/images/stories/docs/clinical/guidance/uk_kpi_qa_standards_for_colonoscopy.pdf.
- M.KaminskiS.Thomas-GibsonM.BugajskiPerformance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement InitiativeEndoscopy492017378397
- M.D.RutterC.R.ReesQuality in gastrointestinal endoscopyEndoscopy462014526528
- D.R.GavinR.M.ValoriJ.T.AndersonM.T.DonnellyJ.G.WilliamsE.T.SwarbrickThe national colonoscopy audit: a nationwide wide assessment of the quality and safety of colonoscopy in the UKGut622013242249
- A.FraserG.GambleT.RoseJ.DunnColonoscopy audit over 10 years—what can be learnt?J N Z Med Assoc12620132535
- W.SanchezG.C.HarewoodB.T.PetersenEvaluation of diagnostic yield in relation to procedure time on screening or surveillance colonoscopyAm J Gastroenterol99200419411945
- M.BrahmaniaJ.ParkS.SvartaJ.TongR.KwokR.EnnsIncomplete colonoscopy: maximizing completion rates of gastroenterologistsCan J Gastroenterol262012589592
- A.GadoB.EbeidA.AxonQuality assurance in gastrointestinal endoscopy, an Egyptian experienceArab J Gastroenterol172016153158
- S.R.GuruduF.C.RamirezQuality metrics in endoscopyGastroenterol Hepatol92013228232
- S.Morán SánchezE.TorrellaP.Esteban DelgadoColonoscopy quality assessmentRev Esp Enferm Dig1012009107112
- P.D.ThomasA.ForbesJ.GreenGuidelines for the investigation of chronic diarrhoea, 2nd editionGut52Suppl V2003V1V15
- Roland Valori. A guide to auditing quality and safety items of the endoscopy global rating scale; 2009. Internet. Available from: http://www.thejag.org.uk/downloads/Unit%20Resources/A%20guide%20to%20auditing%20quality%20and%20safety%20items%20of%20the%20Endoscopy%20GRS.pdf.
- J.B.DaviesS.K.RoySuccessful completion of upper gastrointestinal endoscopy: a retrospective comparative study on patients who had endoscopy with sedation and without sedationJ Digest Endosc420133338
- A.GadoB.EbeidA.AbdelmohsenA.AxonClinical outcome of acute upper gastrointestinal haemorrhage among patients admitted to a government hospital in EgyptSaudi J Gastroenterol1820123439
- A.GadoB.EbeidA.AbdelmohsenA.AxonPredictors of mortality in patients with acute upper gastrointestinal hemorrhage who underwent endoscopy and confirmed to have variceal hemorrhageAlex J Med512015295304
- C.ZaltmanH.S.P.SouzaM.E.C.CastroM.F.S.SobralP.C.P.DiasV.LemosJrUpper gastrointestinal bleeding in a Brazilian hospital: a retrospective study of endoscopic recordsArc Gastroenterol3920027480
- P.A.McCormickC.O’KeefeImproving prognosis following a first variceal haemorrhage over four decadesGut492001682685
- R.HarryJ.WendonManagement of variceal bleedingCurr Opin Crit Care82002164170
- A.ShararaD.RockeyGastroesophageal variceal hemorrhageN Engl J Med3452001669681
- K.BambhaW.KimR.PedersenJ.BidaW.KremersP.KamathPredictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosisGut572008814820
- H.FallatahH.NahdiM.KhatabiVariceal hemorrhage: Saudi tertiary center experience of clinical presentations, complications and mortalityWorld J Hepatol42012268273
- M.KaminskiJ.RegulaE.KraszewskaQuality indicators for colonoscopy and the risk of interval cancerN Engl J Med362201017951803
- S.FaissThe missed colorectal cancer problemDig Dis29suppl 120116063
- J.KingsleyS.KaranthF.L.RevereD.AgrawalCost effectiveness of screening colonoscopy depends on adequate bowel preparation rates – a modeling studyPLoS ONE112016e0167452
- B.DenisA.M.WeissA.PeterJ.BottlaenderB.ChiappaQuality assurance and gastrointestinal endoscopyGastroenterol Clin Biol28200412451255
- G.C.HarewoodV.K.SharmaP.de GarmoImpact of colonoscopy preparation quality on detection of suspected colonic neoplasiaGastrointest Endosc5820037679
- Sidhu S, Geraghty J, Karpha I, Wark L, Logan C, Sarkar S. Outcomes following an initial unsuccessful colonoscopy: a 5-year complete audit of teaching hospital colonoscopy practice. Gut 2011 Supp; 60:pA201.
- J.RomagnuoloR.EnnsT.PonichJ.SpringerD.ArmstrongA.BarkunCanadian credentialing guidelines for colonoscopyCan J Gastroenterol2220081722
- C.BowlesR.LeicesterC.RomayaE.SwarbrickC.B.WilliamsO.EpsteinA prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal screening tomorrow?Gut532004277283
- Bassi A, O'Toole P. Improving colonoscopy completion rates: the impact of audit. Gut 2003 Supplement 1;52:pA6.
- G.C.HarewoodN.C.MattekJ.L.HolubD.PetersD.A.LiebermanVariation in practice of ileal intubation among diverse endoscopy settings: results from a national endoscopic databaseAliment Pharmacol Ther222005571578
- R.MakkarR.LopezB.ShenClinical utility of retrograde terminal ileum intubation in the evaluation of chronic non-bloody diarrheaJ Digest Dis142013536542
- S.MoriniR.LorenzettiF.StellaM.MartiniC.HassanA.ZulloRetrograde ileoscopy in chronic nonbloody diarrhea: a prospective, case-control studyAJG98200315121515
- C.HassanA.RepiciPolypectomy: no training, no cancer prevention!Endosc Int Open52017E198E200
- D.RexJ.BondS.WinawerQuality in the technical performance of colonoscopy, the continuous quality improvement process for colonoscopy: recommendations of the US Multi-Society Task Force on Colorectal CancerAm J Gastroenterol9720021296
- P.B.CottonQuality endoscopists and quality endoscopy unitsJ Interv Gastroenterol120118387
- D.ArmstrongR.HollingworthD.MacIntoshPoint-of-care, peer-comparator colonoscopy practice audit: the Canadian Association of Gastroenterology Quality Program – endoscopyCan J Gastroenterol2520111320